Prior to this 2016 trial by Robert Lustig et al., evidence investigating the metabolic impact of sugar consumption was confounded by four major factors:
- Studies that rely on dietary recall (i.e., that ask subjects how much sugar they consume) are known to provide unreliable estimates of actual sugar consumption;
- Many studies, especially short-term studies, have tested doses of fructose that do not match real-world consumption in either their quantity or their nature;
- Many studies have been confounded by weight gain—that is, fructose/sugar restriction studies have induced weight loss, and fructose/sugar dosing studies have induced weight gain—making it impossible to understand which effects were caused by the change in weight and which were due to the dietary shift;
- Other studies have been confounded by changes in the number or nature of calories subjects were fed. For example, if sugars are removed from the diet and either not replaced or replaced by fat or protein, then any observed effects could be attributed to a change in calorie or carbohydrate intake.
This short-term trial was designed to isolate the specific effects of a reduction in dietary fructose on various markers of metabolic health.
Forty-three Latino and African-American adolescents were tested for nine days. All subjects were fed a diet similar to their baseline diet (51% carbohydrate, 16% protein, 33% fat by calories), but the share of total calories coming from dietary sugar was reduced from 27.7% to 10.2%. The exchange was performed by swapping sugar-containing foods for low-sugar or sugar-free substitutes, purchased from local grocery stores. Any caloric deficit was refilled by adding starch to the diet. Subjects were provided all their food, prepared at the UCSF Bionutrition Core, for the duration of the study. This was a single-arm design where each subject served as his/her own control, and the difference between metabolic markers at baseline and at 10 days was used to infer the effect of sugar restriction.
Over 10 days, subjects showed a variety of metabolic changes, mostly improvements, including:
- 4.9 mmHg decrease in mean diastolic BP (but no change in systolic BP);
- 53% reduction in fasting insulin and a 0.3 mmol/L decrease in fasting glucose, alongside similarly large improvements in glucose and insulin AUC as measured by OGTT;
- 46% reduction in fasting triglycerides, 0.3 mmol/L reduction in LDL-C and 0.1 mmol/L reduction in HDL-C;
- significant reduction in AST and non-significant reduction in ALT (markers of liver health); and
- unintended 0.9 kg mean weight loss (Researchers attempted to feed subjects enough calories to maintain weight, but 33 out of 43 subjects reported they were unable to finish all the calories they were provided).
In sum, the data suggests nine days of dietary sugar restriction results in a reduction in hyperinsulinemia, increased peripheral lipolysis and fatty acid oxidation, and possibly increased liver health.
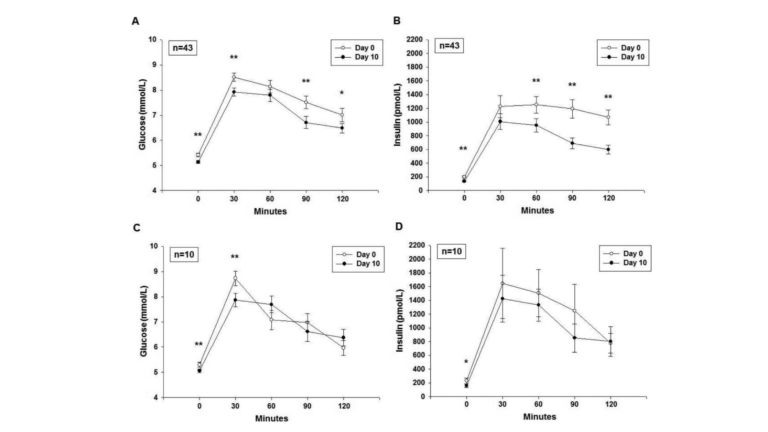
a) Glucose, and b) insulin responses (Mean±SEM) to OGTT on Day 0 and 10 for all 43 participants. c) Glucose, and d) insulin responses to OGTT on Day 0 and 10 for the ten participants in the post-hocsensitivity analysis who gained weight during the study interval.
* p<0.05 paired t-test (Day 10 vs. Day 0) at each individual time point
** p<0.01 paired t-test (Day 10 vs. Day 0) at each individual time point
This study provides an especially rigorous test of the hypothesis that dietary sugar restriction has unique and specific metabolic benefits. Subjects were fed a processed-food-based, “kid-friendly” diet that differed from their baseline diets in a single way: less sugar. It is important to note that the subjects received the same amount of calories and the same amount of total carbohydrates as their baseline diets. This single specific change—a reduction in sugar intake—led to a variety of metabolic improvements in only nine days.
The research team concluded:
Concerns surrounding the role of sugar consumption in chronic disease have previously focused on its caloric equivalence, and its role in fomenting increases in weight. Furthermore, previous clinical studies have relied upon excessive sugar administration, which introduces experimental artifact. This study mitigates all three of these concerns, by intervening in children who are already sick with metabolic syndrome, and by adjusting for effects of calories, weight gain, and adiposity. This study argues that the health detriments of sugar, and fructose in specific, are independent of its caloric value or effects on weight. Further studies will be required to determine whether sugar restriction alone can impact metabolic syndrome in adults, and whether such effects are short-lived or long-term.
Comments on Isocaloric fructose restriction and metabolic improvement in children with obesity and metabolic syndrome
I am also really surprised that only 9 days has this much effects. The body is an extraordinary resilient machine! Give it what it needs and it will function really well.
That makes me wonder how long does it take to completely derailed this? What is the impact of one big "cheat meal" full of sugar on a healthy person?
I am interested in the reduction in AST and ALT after only 9 days. Imagine what might happen in a month or even a year? This would have a tremendous impact on NAFLD.
This study supports the negative impact of added sugar, specifically fructose, independent of calories and weight. It’s impressive that only 9 days of dietary changes results in metabolic improvement. Quite sad that everyday I see so many kids drinking sugar sweetened beverages. We need to stop poisoning our youth.
Isocaloric fructose restriction and metabolic improvement in children with obesity and metabolic syndrome
3