Cardiovascular guidelines in the U.S. (1) and elsewhere (2) generally establish LDL cholesterol (LDL-C) as the primary marker for heart disease risk and consequently focus on treatments to lower LDL-C. The widely cited diet-heart hypothesis proposes elevated levels of LDL cholesterol increase heart disease risk, though this association has been disputed.
This 2015 trial analyzed Womens’ Health Study (WHS) data, including 1,070 coronary events over 17.2 years from a pool of 27,533 female health-care professionals, to assess the relative accuracy of LDL-C compared to three alternative lipid biomarkers: LDL particle number (LDL-P), apoB particle number (apoB), and total non-HDL cholesterol (NHDL-C).
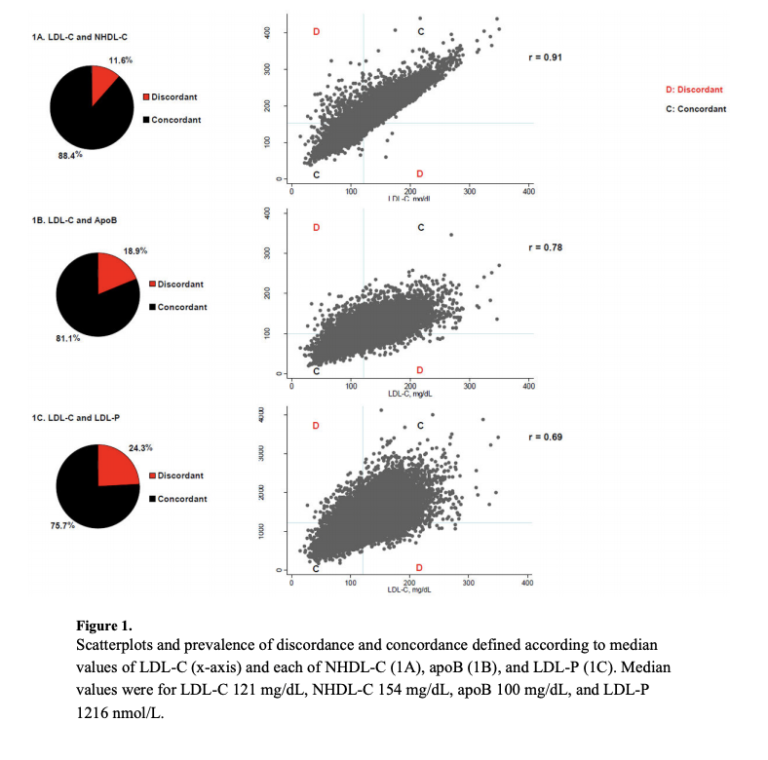
For the majority of the population, these markers are concordant — that is, they are above the median in both LDL-C and these alternative measures or below the median in both. However, a meaningful minority of individuals show discordance between these alternative measures and their LDL-C levels — that is, their LDL-C level is above the median, and one or more of these other markers is below the median, or vice versa (Figure 1).
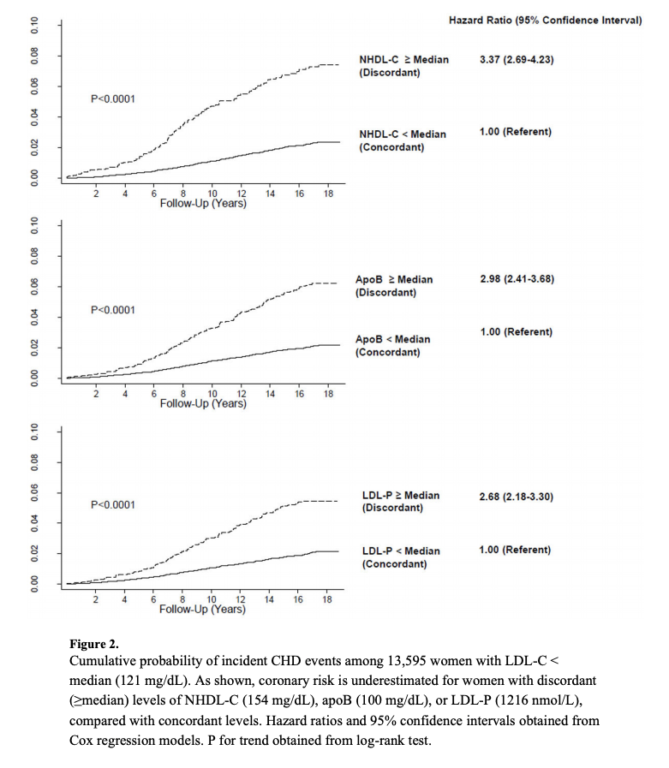
Among study subjects, 11.6% had either high LDL-C and low NHDL-C or vice versa. In other words, these subjects’ markers showed a discordance between their LDL-C and NHDL-C levels. Those with low LDL-C but high NHDL-C had over three times as many cardiovascular events (per person-year) as their peers with low levels on both measures.
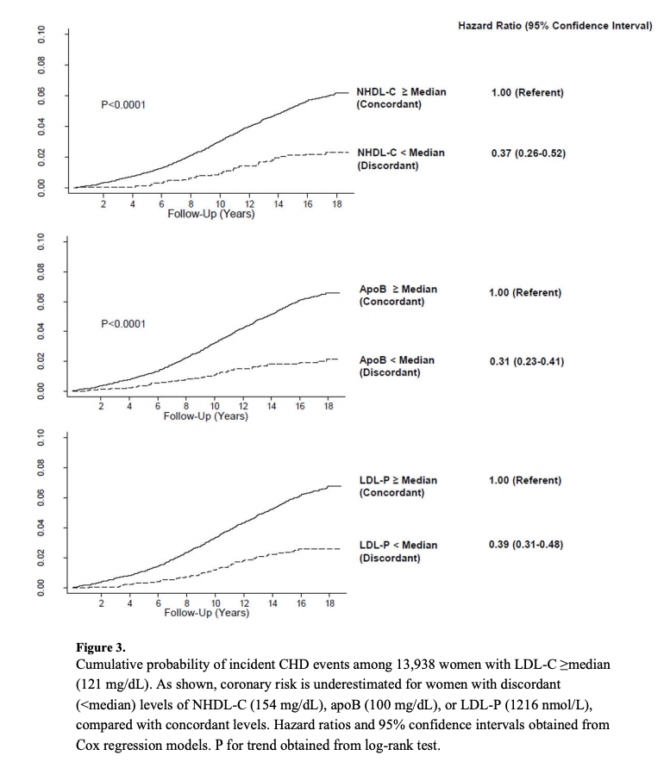
Similarly, those with high LDL-C but low NHDL-C had approximately one-third as many cardiovascular events as those who scored high on both measures. The apoB and LDL-P markers had similar predictive value; subjects with low LDL-C but high apoB or LDL-P experienced 2.5 to three times as many cardiovascular events as their concordant peers, and subjects with high LDL-C and low apoB or LDL-P experienced 30-40% as many events as their peers (Figures 2 and 3).
Discordantly high LDL-P, apoB, or NHDL-C levels are indicative of small, dense, cholesterol-poor LDL particles and were more common in subjects with higher BMI, greater insulin resistance, and higher triglyceride levels. Discordantly low values of these alternative measures, conversely, indicates large, cholesterol-rich particles.
In sum, this study indicates LDL-C alone substantially over- or underestimates heart disease risk in a nontrivial share of the population. In individuals with low levels of insulin resistance — such as those following a low-carb diet alongside regular exercise — high LDL-C levels may not indicate elevated heart disease risk, but insulin-resistant individuals with low LDL-C levels may still be at a high risk of heart disease.
REFERENCES
- Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults and 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines
- The task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS) and The fifth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice and 2012 update of the Canadian Cardiovascular Society guidelines for the diagnosis and treatment of dyslipidemia for the prevention of cardiovascular disease in the adult.
Comments on Discordance of Low-Density Lipoprotein (LDL) Cholesterol With Alternative LDL-Related Measures and Future Coronary Events
Meanwhile the European Society of Cardiology and the European Atherosclerosis Society updated their cholesterol guidelines saying "there is no lower limit of LDL cholesterol that is known to be unsafe," and we should strive to "go as low as you can go." So, if I'm following a low carb diet and exercising regularly (a CrossFitter, perhaps) and I have an LDL-C value that is outside of the proverbial box, what then? Oh, of course, put me on a statin.
Discordance of Low-Density Lipoprotein (LDL) Cholesterol With Alternative LDL-Related Measures and Future Coronary Events
1