“Studies show …” sounds an alarm that you are about to read exaggerated claims, questionable science, and only occasionally, real information. “Red meat causes diabetes,” “Eggs and cholesterol will make you sick,” and “low-carbohydrate diets will kill you.” Those of us trained in the physical sciences are astounded at the confusion and poor scientific logic that are rampant. At the same time, we are seeing major steps forward in nutritional medicine: Three recent papers show that, for many people, Type 2 diabetes can be cured with diet (1-3). And yet, the medical journals and popular media trumpet the most unreliable results. It’s pretty hard for scientists to penetrate some studies, and it is obviously worse for the end user: the person who simply wants to know what to eat. Oddly, there are warnings by many, including editors of the medical journals, that much of what is published — half is a common figure — is unreliable, unreproducible, and ultimately false (4). They don’t say which half. And mostly they don’t explain how they, the editors, the presumed gatekeepers, let this happen. It often seems that despite having more information now than in the past, you are pretty much on your own in deciding what is true and what is bogus.
The good news that makes things better than they once were is that you can often go back to the original scientific or medical paper and see for yourself. You really can be the judge. Good science is consistent with intuition, common sense, and basic honesty. Your intuition tells you that in a food supply with hundreds of different items, it is unlikely that something like eggs or red meat will, by itself, have a big impact on your susceptibility to disease or lifespan. A scientific study that says otherwise must have a very convincing argument and overwhelming data (which they never do). Also, while there is a nutritional medical establishment that is very reactionary and still maintains significant power, things are changing. There is, for instance, the increased availability of information on social media, including large numbers of meetings on alternative theories and methods (There’s a low-carbohydrate conference virtually every month). These, and the proliferation of scientific studies, make the old ways increasingly untenable. Here, the average end user finds allies among established professional scientists.
If you wish truly to be the judge, here are some guides to reading the nutritional medical literature:
- The burden is on the author of a scientific paper to make things clear. The goal of a scientific paper is to teach. There are complexities in science, but the job is to explain things in as straightforward a way as possible. Technical terms may have to be researched — many are only a Google away — but you should be sensitive to any attempt on the part of the authors to snow you.
- What scientists look for first in a paper are the pictures. I know it sounds funny, but in fact, figures are almost always better than tables. Whole books have been written about this idea. An experimental scientific paper that has no pictures should be viewed with suspicion.
- Observational studies, such as epidemiological studies, simply record outcomes. It is universally understood that observational studies can only show associations that are not necessarily causal in nature. The principle is frequently stated in papers that, nonetheless, then strongly suggest causality even as they offer the disclaimer. Such papers are obviously misleading, and it is important to attend to how much causality is implied. As described by The Rise and Fall of Modern Medicine (5), epidemiology “is constrained in its search for the causes of disease by only being able to measure that which is measurable in people’s lives. It cannot, by definition, discover hitherto unknown biological phenomena such as the new bacterium [at the time, in 1999,] helicobacter.” Modern biology advances most on mechanism. The author must explain the biology if it is not obvious. This is one of the criteria that has been established in science and courts of law.
- Be suspicious of arbitrary rules, “levels of evidence,” and “gold standards.” These are unknown in the physical and biological sciences, and there is nothing in medical research that changes that. The best experimental method is one that answers the scientific question. The Emperor of All Maladies (6) described the original observations on cigarette smoke and lung cancer. In the original cohort (cohort is the common term for a well-identified experimental group in a scientific study), there were 789 deaths, of which 36 were attributed to lung cancer. When the researchers asked how many of these were smokers, they found it was all 36. No statistics needed.
- Distinguish between statistical significance and biologic or clinical significance. If a scientific paper says, for example, that an association that was found between red meat and cancer is statistically significant, that only means that there is a very low probability that the association arose simply by chance. What it doesn’t say is that if you redid the analysis with another set of data testing the same parameters, you would get the same result. More important, “statistically significant” is a mathematical result. It does not tell you anything about biological or physical significance — that is, whether there is any reason for you to reduce red meat in order to avoid cancer. That comes only from experience and knowledge of the biology. If an experimental study shows you that a particular diet was associated with a statistically significant loss of 1 kilogram over several weeks, you know this is not meaningful, because you can lose a kilogram overnight. Statistics is a tool. Scientists are not cost accountants.
- It is frequently said that observational studies can only generate hypotheses. That is not right. They test hypotheses. They are not neutral. Single observations may generate a hypothesis, but observational studies constitute an attempt to support that hypothesis. If you study the association between fat and cardiovascular disease, you have something in mind, and you suspect that fat is the cause. If the association is weak, you have to reject your hypothesis.
- Excluding theories is more important than showing consistency. Consistency must always be tested against. Of course, a theory can only truly be excluded if it is mathematically excluded or leads to a logical contradiction. On the other hand, while an association is not necessarily linked to causality, a lack of association is an argument for a lack of causality.
- Note: Before considering further details, some points on language are important. The numbers in nutritional epidemiology are expected to show an association between some food or dietary practice and a medical outcome. This outcome is usually presented as odds ratio (OR), relative risk (RR), or hazard ratio (HR), which compare the effect of, say, high red meat consumption versus low red meat consumption on risk of cancer. These quantities are obviously relative statistics. They are mathematically somewhat different, but for the cases of interest here (generally low incidence of disease), they can be taken as equivalent. From the name, you can see that they are relative values and have the limitation of obscuring absolute values. “Risk” in statistics means probability. (It is important not to confuse this with the commonly used meaning of susceptibility to poor outcome. Statistically, risk may refer to the probability of getting better.) Probability is, by analogy with betting, the number of ways of winning divided by all the possible outcomes.
- Considering all the caveats above, how do you tell when epidemiological or observational studies can be taken to support causality? In answering that question, the standard is the criteria proposed by Bradford Hill, who performed the original work on cigarette smoke and lung cancer. Hill was clear that there were not formal rules but rather reasonable ideas that derive from common sense and shared experience. There are several discussions of Hill’s rules (7), and not all will apply to every case, but the most important is the one that Hill considered as first: the strength of the association. Hill’s own work on cancer showed, “The death rate from cancer of the lung in cigarette smokers is nine to ten times the rate in non-smokers and the rate in heavy cigarette smokers is twenty to thirty times as great.” Hill was concerned that even a ratio of 2-to-1 for smokers vs. nonsmokers for incidence of heart disease was marginally reliable. It is a rare paper in the epidemiological literature that even gets close to 2-to-1. Odds of 2-to-1 are usually a minimum in a court of law to introduce epidemiological data into evidence. The persistent acceptance of low relative-risk values actually leaves almost all of nutritional epidemiology open to question.
- Sometimes it’s easier to visualize odds ratios by converting to a rough estimate of odds. A simple way to do that is to add 1 to the odds ratio and take the reciprocal. For example, if the odds ratio is 1.5, add 1 to get 2.5 and the reciprocal is 0.4, which is the lower odds; that is, 1.5 is the same as 60-to-40 – or close to even – odds. Ask yourself how much you would change your lifestyle for 60-to-40 odds.
- Is there evidence of bias? Are value judgments stated as fact? “Healthy,” and “evidence-based” are value judgments, and it is for the reader, not the author, to decide. Even one of those can turn a scientific paper into an infomercial. In the Rashmi Sinha paper discussed below, the categories of red meat are referred to as “high-, medium-, and low-risk meat diet.” This is obviously trying to manipulate the readers. That’s not kosher.
- The basic idea of most of the recommendations here is to be critical and skeptical of the paper you’re reading. There are, however, criticisms that are not relevant. You must assume that the data are reported honestly — falsification is very serious and cannot be considered without clear evidence. You can be very critical of the authors’ analysis, but you must assume that the data are as they say.
An example
To demonstrate some of the 12 points, I will review a study that I discussed in Nutrition in Crisis (4). Sinha, et al. (8) was one of several studies that claim to have found that red meat consumption is a risk for cancer or other disease states, or that, in fact, high consumption of red meat increases chance of death by any cause. In this study, there were two cohorts of 322,263 men and 223,390 women. The subjects were given a questionnaire on their lifestyle and eating habits, and their consumption of red meat and white meat was determined. Sinha, et al. broke the cohorts into five groups (quintiles), each according to the amount of red meat consumed, keeping as many other parameters as possible constant across quintiles. (Different studies might use tertiles, quartiles, etc. The generic term is quantile.) Let’s look at the risk for death from cancer. That’s supposed to be the big risk with red meat. So what did Sinha, et al. discover?
First, there are no pictures. A little discouraging. There are several mind-numbing tables with much data. An excerpt of Table 2 from the paper is shown in Figure 1.
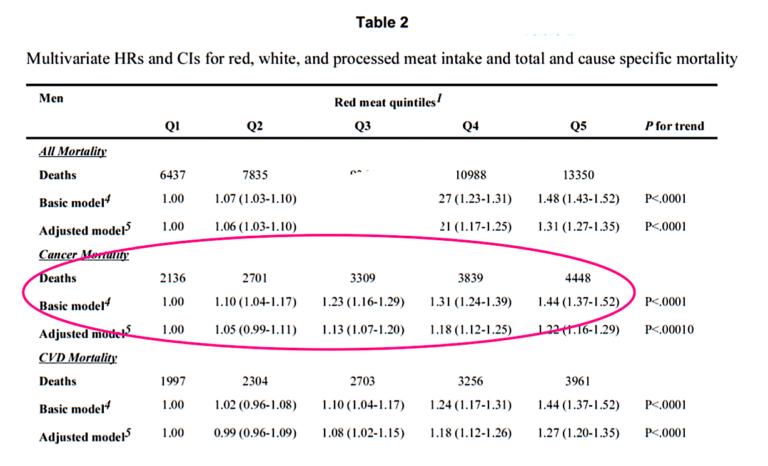
Figure 1: Hazard ratios (HR) for mortality associated with red meat consumption. Excerpt of Table 2 from Sinha, et al. (9).
This is discouraging. Lots of numbers and statistics. And when you try to get the bottom line from the abstract, which is supposed to give you the bottom line, you get the following (don’t try to read this):
There were 47,976 male deaths and 23,276 female deaths during 10 years of follow-up. Men and women in the highest vs lowest quintile of red (HR, 1.31 [95% CI, 1.27-1.35], and HR, 1.36 [95% CI, 1.30-1.43], respectively) and processed meat (HR, 1.16 [95% CI, 1.12- 1.20], and HR, 1.25 [95% CI, 1.20-1.31], respectively) intakes had elevated risks for overall mortality …
This is as hard to read for scientists as for everybody else. There is no obligation to put all the statistics in the abstract; it only makes it hard to read. The general principle is that style is not independent of substance. Our first principle above was that the first goal in writing a paper is to teach.
Let’s try to extract the numbers we need, namely the risk — that is, the probability, which, again, is the number of ways of getting a particular result divided by all possible outcomes. Here all possible outcomes are the number, n, in each quintile. We are just looking at men, and there were 322,263 men in the study. So n for each quintile is 322,263/5 = 64,453.
Now, looking at Table 2, we see 4,448 deaths from cancer in Q5 (the group with the highest red meat consumption). So the probability of death from cancer as a big red meat consumer is 4,448/64,453 = 0.069 or 6.9 %. This does not sound like big risk, but it’s something, and we have to compare it to the risk of the group with low red meat consumption. There were 2,136 deaths from cancer in Q1 (the group with the lowest red meat consumption). So the probability of death from cancer as a low red meat consumer is 2,136/64,453 = 0.033 or 3.3 %, which is even lower. We can similarly calculate the risk for each quintile, and we can make the figure that we wanted to see for ourselves:
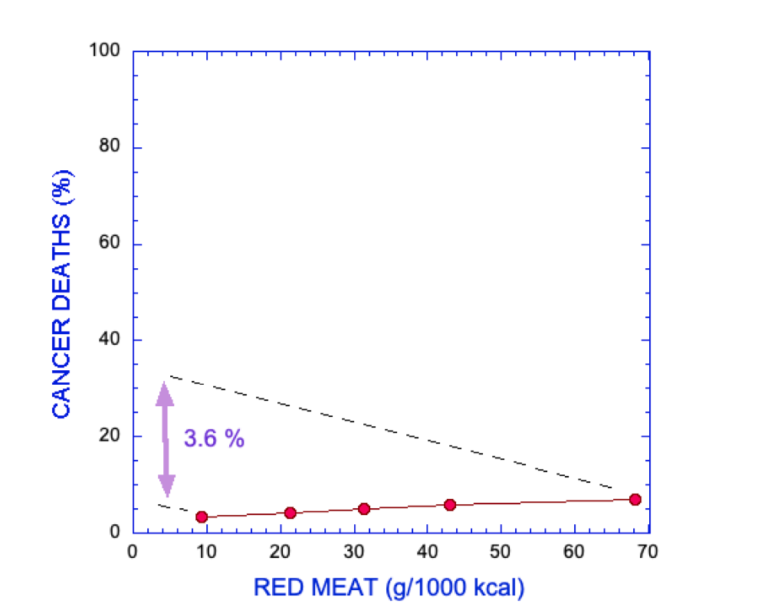
Figure 2: Cancer deaths (percent of quintile) as a function of red meat consumption — values correspond to quintile number from left to right. Data from Sinha, et al. (9).
This is somewhat underwhelming. The overall risk in the experiment is low, and a large (seven-fold) increase in red meat gives us only a 3.6% increase in risk. What about the odds ratio? Well, 6.9/3.3 = 2.1, which would actually conform to Hill’s criterion. However, if you look at Table 2, the authors show a HR (again, roughly the same as OR) of only 1.44 or 1.22, depending on how the data are treated. The problem is that there are other factors that could contribute to cancer deaths. The so-called confounders have to be corrected for.
Confounders
Sinha, et al. point out that dividing people by red meat consumption produces groups that have other differences. The authors note, “Subjects who consumed more red meat tended to be married, more likely of non-Hispanic white ethnicity, more likely a current smoker, have a higher body mass index, and have a higher daily intake of energy, total fat, and saturated fat, and they tended to have lower education and physical activity levels and lower fruit, vegetable, fiber, and vitamin supplement intakes” (my emphasis). They then correct the data for these variables, and in their “adjusted model,” the HR goes down to 1.44. This last paragraph sets off all kinds of alarms to the scientist who’s reading this.
It turns out that confounders are symmetrical; in other words, if red meat is a risk and has to be corrected for smoking, that’s the same thing as saying that smoking is a risk and has to be corrected for red meat. Which makes more sense? You know that smoking is a risk; so it’s more likely that the primary effect is the smoking, not the red meat. And the errors are worse because the assumption in correcting for confounders is that there’s a linear relationship: the effect due to smoking plus the effect of red meat. That’s a big assumption. If red meat is a risk at all, that risk may be modified if you’re a smoker — made worse or better (unlikely to be better) — because if there’s any risk in red meat at all, smokers may respond worse because smoking has a global effect. In fact, all the confounders may be in nonlinear relationships with each other. And there are some missing confounders, like carbohydrate. Most of us think that red meat in a lettuce wrap may have different effects than beef Wellington.
All this would be okay if we were actually seeing a big effect, if it were even 2.1-to-1, as we found with the raw data. But the HR is only 1.44. What does that mean? If high red meat and low red meat had the same risk, the RR would be 1.0; in other words, 50-to-50 odds. Using our quick calculator above, 1.44 is the same as 59-to-41. Again, are we really going to give up a steak for those odds?
There’s another thing to understand: This is what is called in statistics “two-tailed.” That means if the risk for eating red meat goes down, the risk for not eating red meat goes up. To make that clear, consider that not everybody who smokes gets lung cancer, and not everybody who gets lung cancer is a smoker, but nobody thinks smoking simply has a smaller risk for some people. It’s just that some are less susceptible. One-tailed statistics applies. Cigarette smoke is a toxin. You either get lung cancer, or you’re immune, or it hasn’t caught up to you yet. But for red meat in the diet, you don’t know before you do the experiment. In fact, many people, particularly the elderly, probably don’t get enough red meat. If red meat were a risk, it might also be that replacing red meat with something else might also be a risk for some reason.
Finally, Sinha, et al. bring out an additional point. We have suspicions in dietary experiments about whether the independent variable is reliable and accurately measured. A principle not explicitly considered by Hill is that error assessment must apply to the independent variable — in this case, the consumption of red meat. If there is significant error in the measurement of red meat consumption, you would have to have a very strong RR to be convinced of an effect. In fact, “The correlations for red meat consumption assessed from the food frequency questionnaire compared with two 24-hour recall diaries were 0.62 for men and 0.70 for women, as reported previously.” An error of 30 to 38 % could move individuals from one quintile to the next.
Bottom line: To read the medical literature, be skeptical and trust common sense. The burden is on the author to make things clear, to teach.
References
- Lennerz B, et al. Management of Type 1 Diabetes With a Very Low–Carbohydrate Diet. Pediatrics 141.6(2018).
- Hallberg SJ, et al. Effectiveness and Safety of a Novel Care Model for the Management of Type 2 Diabetes at 1 Year: An Open-Label, Non-Randomized, Controlled Study. Diabetes Ther. 9(2018): 583–612.
- Saslow L., et al. Outcomes of a Digitally Delivered Low-Carbohydrate Type 2 Diabetes Self-Management Program: 1-Year Results of a Single-Arm Longitudinal Study. JMIR Diabetes, 2018.
- Feinman RD. Nutrition in Crisis. White River Junction, Vermont: Chelsea Green, 2019.
- LeFanu J. The Rise and Fall of Modern Medicine. New York: Carroll & Graf, 1999.
- Mukherjee S. The Emperor of All Maladies. New York, Scribner: 2010.
- Hill AB. The Environment and Disease: Association or Causation? Proceedings of the Royal Society of Medicine. 58(1965): 295-300.
- Sinha R., et al. Meat intake and mortality: a prospective study of over half a million people. Arch Intern Med. 169.6(2009): 562‑571.
 Richard David Feinman, Ph.D., is a professor of cell biology at the State University of New York Downstate Medical Center in Brooklyn, where he has been a pioneer in incorporating nutrition into the biochemistry curriculum. A graduate of the University of Rochester and the University of Oregon, Dr. Feinman has published numerous scientific and popular papers. He is the founder and former co-editor-in-chief (2004–2009) of the journal Nutrition & Metabolism. He is currently researching the application of ketogenic diets to cancer.
Richard David Feinman, Ph.D., is a professor of cell biology at the State University of New York Downstate Medical Center in Brooklyn, where he has been a pioneer in incorporating nutrition into the biochemistry curriculum. A graduate of the University of Rochester and the University of Oregon, Dr. Feinman has published numerous scientific and popular papers. He is the founder and former co-editor-in-chief (2004–2009) of the journal Nutrition & Metabolism. He is currently researching the application of ketogenic diets to cancer.
Reading the Nutritional Literature: A Skeptic’s Guide