Question: Does a low-carbohydrate diet without caloric restriction, delivered through a community clinic, lead to significant improvements in metabolic health among diabetic patients?
Takeaway: This retrospective cohort study found a low-carbohydrate diet (< 20 grams of carbohydrate per day) led to significant improvements in HbA1c and weight loss alongside discontinuation of anti-hyperglycemic medications in diabetic patients. Growing evidence supports the use of low-carbohydrate diets in the treatment of diabetes.
More than a dozen studies since 2005 have shown low-carbohydrate, high-fat diets (LCHF) lead to significant improvements in glycemic control and weight in diabetics, and in many cases support discontinuation of medications to treat hyperglycemia, hypertension, and other comorbidities (1). These changes occur alongside shifts in cardiovascular risk markers (including HDL cholesterol, LDL particle size, and triglyceride-to-HDL ratio), which indicates reduced cardiovascular risk as well (2). Some meta-analyses have found the impact of low-carbohydrate diets on glycemic control are inconsistent (3), but these reviews have often combined studies using moderate carbohydrate restriction (e.g., diets in which 40% of calories are carbohydrate) with studies of more severe carbohydrate restriction, thus diluting the perceived impact of the latter on glycemic control.
This October 2019 piece investigated the effects of a low-carbohydrate, high-fat diet on a cohort of Type 2 diabetics.
Researchers instructed 49 patients at two Johns Hopkins Community Physicians practices to follow a LCHF diet for three months. The patients were told to limit net carbohydrate intake to <20 grams per day, with 20-25% of calories coming from protein and the remainder (65-70%) coming from fat. Patients were told to eat when hungry without deliberately restricting caloric intake. All patients placed on an LCHF diet discontinued sulfonylurea and reduced their insulin doses at diet initiation to prevent hypoglycemia. These patients were compared to controls, matched for age and baseline BMI, who received dietary advice in line with American Diabetes Association (ADA) recommendations (4). The study used a retrospective cohort design, comparing the outcomes of patients given these differing forms of treatment in the course of typical clinical care. Patients were followed for three months and tracked across four monthly visits.
Mean changes in HbA1c and body weight are summarized in the figures below. Patients following the LCHF diet showed an immediate, significant reduction in HbA1c that was maintained for the entire three-month observation period. This occurred alongside continuous weight loss. At the end of the three-month study period, mean HbA1c had declined by 1.29% among the LCHF diet patients (to 6.67%). No significant decline was observed in patients receiving usual care (UC). Mean weight loss was 12.3 kg greater in the LCHF group than the UC group. Mean fasting plasma glucose decreased by 43.5 mg/mL in the LCHF group, with no significant decrease in controls. Plasma lipid values did not change significantly in either group.
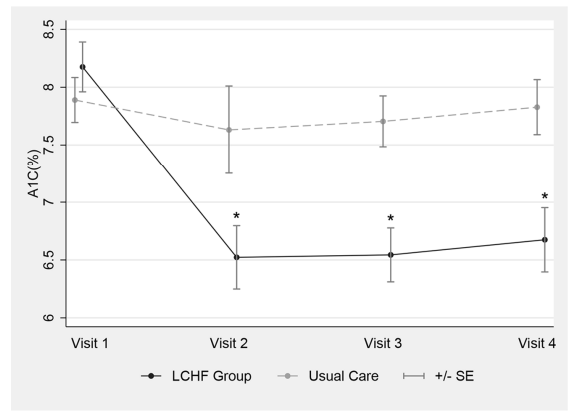
Figure 1: Mean change in HbA1c in patients following a low-carbohydrate, high fat (LCHF) diet or receiving usual care over three months
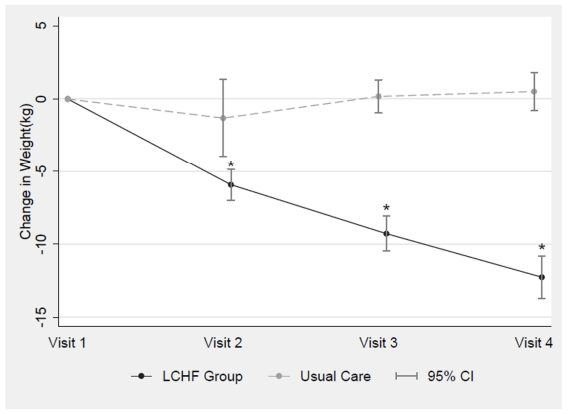
Figure 2: Mean change in weight in patients following a low-carbohydrate, high fat (LCHF) diet or receiving usual care over three months
The figures below summarize changes in medication usage between groups. All 21 LCHF diet patients who began the study on insulin either reduced their daily insulin dose (63.2%) or discontinued insulin entirely (36.8%) over three months. LCHF subjects’ mean daily insulin dose decreased significantly by the first check-in and continued to decrease through all subsequent visits. In patients receiving usual care, a greater share increased their insulin dose over this three-month period (35.9%) than reduced or discontinued insulin (18.0% and 5.1%, respectively). All LCHF subjects remained off sulfonylureas for the three-month observation period.
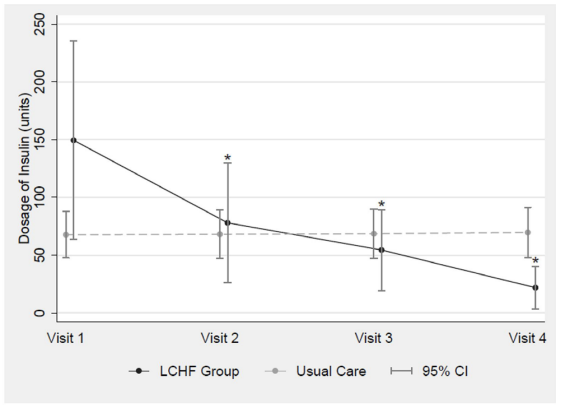
Figure 3: Mean daily insulin dose in patients following a low-carbohydrate, high fat (LCHF) diet or receiving usual care over three months
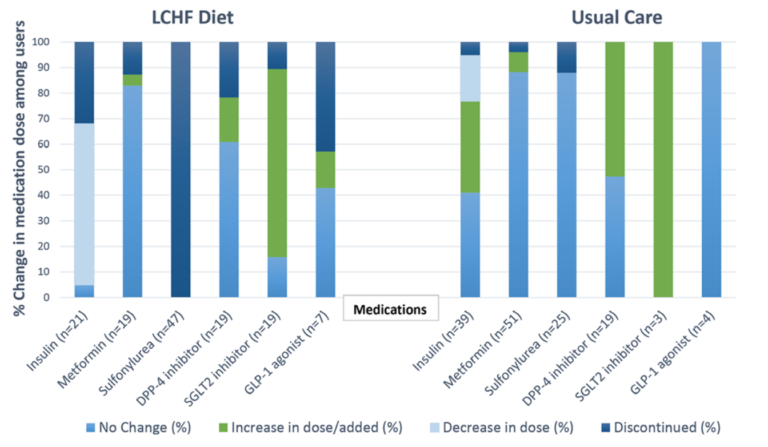
Figure 4: Changes in medication use in patients following a low-carbohydrate, high fat (LCHF) diet or receiving usual care over three months
Meta-analyses and reviews since the mid-2000s have argued there is insufficient evidence to define the best diet for the treatment and prevention of Type 2 diabetes, though most agree diets that cause weight loss generally improve glycemic control (5). While this study cannot isolate the impact of weight loss from the impact of carbohydrate restriction in these patients, it adds to a growing body of evidence indicating carbohydrate-restricted diets lead to rapid and durable improvements in metabolic health in diabetics. The magnitude of improvement in HbA1c and weight seen here is similar to findings from studies by the Virta group. Subjects in the Virta studies demonstrated a mean HbA1c reduction of 1.5% over one year after following a ketogenic diet and exhibited similar rates of medication discontinuation (6).
The LCHF diet establishes glycemic control within days, prior to any weight loss, simultaneously reducing the need for exogenous insulin and allowing the use of stored fat as fuel (7). Over time, this reduction in endogenous fat stores improves the function of metabolic organs (including the liver, pancreas, and muscle) and improves insulin sensitivity. A growing body of evidence suggests insulin use in diabetics may directly increase cardiovascular risk through similar mechanisms (8), which suggests there may be further long-term benefits associated with effective treatment of diabetes, as is seen here.
The United States spends $106 billion each year on prescription medications to treat diabetes (9). Intensive low-carbohydrate diet programs, while effective, can cost thousands of dollars without insurance, placing them out of reach for many patients (10). This study presents an example of a low-carbohydrate diet delivered via a low-cost, scalable, and accessible methodology.
In sum, this study is part of a growing body of evidence that supports the use of low-carbohydrate diets for the treatment of diabetes.
Notes
- Long term successful weight loss with a combination biphasic ketogenic Mediterranean diet and Mediterranean diet maintenance protocol; Comparison of low- and high-carbohydrate diets for type 2 diabetes management: A randomized trial; Improvements in glucose metabolism and insulin sensitivity with a low-carbohydrate diet in obese patients; Comparative study of the effects of a 1-year dietary intervention of a low-carbohydrate diet versus a low-fat diet on weight and glycemic control in type 2 diabetes; Effect of weight loss with lifestyle intervention on risk of diabetes; Effects of an energy-restricted low-carbohydrate, high unsaturated fat/low saturated fat diet versus a high-carbohydrate, low-fat diet in type 2 diabetes: a 2-year randomized clinical trial; Short-term safety, tolerability and efficacy of a very low-calorie-ketogenic diet interventional weight loss program versus hypocaloric diet in patients with type 2 diabetes mellitus; The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus; Effect of a low-calorie versus low-carbohydrate ketogenic diet in type 2 diabetes; Ketogenic diet to treat type 2 diabetes; Twelve-month outcomes of a randomized trial of a moderate-carbohydrate versus very low-carbohydrate diet in overweight adults with type 2 diabetes mellitus or prediabetes; Effectiveness and safety of a novel care model for the management of type 2 diabetes at 1 year: An open-label, non-randomized controlled study; Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet
- Dietary carbohydrate restriction induces a unique metabolic state positively affecting atherogenic dyslipidemia, fatty acid partitioning, and metabolic syndrome; Effects of low-carbohydrate diets versus low-fat diets on metabolic risk factors: A meta-analysis of randomized controlled clinical trials; Effect of short-term low- and high-fat diets on low-density lipoprotein particle size in normolipidemic subjects
- Ibid., Effects of low-carbohydrate- compared with low-fat diet interventions on metabolic control in people with type 2 diabetes: A systematic review including grade assessments
- ADA recommendations emphasize eating a variety of nutrient-dense foods without providing specific guidelines for carbohydrate, fat, or protein intake.
- Reduction of the incidence of type 2 diabetes with lifestyle intervention or metformin; Beneficial health effects of modest weight loss; A network meta-analysis on the comparative efficacy of different dietary approaches on glycaemic control in patients with type 2 diabetes mellitus; Effectiveness of lifestyle-based weight loss interventions for adults with type 2 diabetes: a systematic review and meta-analysis; Prevention and management of type 2 diabetes: dietary components and nutritional strategies
- Effectiveness and safety of a novel care model for the management of type 2 diabetes at 1 year: An open-label, non-randomized, controlled study
- Ketogenic diets for weight loss: A review of their principles, safety and efficacy; Twenty-four hour profiles and pulsatile patterns of insulin secretion in normal and obese subjects; Effect of insulin on plasma free fatty acids of normal subjects; Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes
- Insulin use and increased risk of mortality in type 2 diabetes: A cohort study; Glucose-lowering with exogenous insulin monotherapy in type 2 diabetes: Dose association with all-cause mortality, cardiovascular events and cancer; Association between serious ischemic cardiac outcomes and medications used to treat diabetes; Association of second-line antidiabetic medications with cardiovascular events among insured adults with type 2 diabetes
- ADA: Economic costs of diabetes in the U.S. in 2017
- The Virta treatment: How it works
Effects of the Low Carbohydrate, High Fat Diet on Glycemic Control and Body Weight in Patients With Type 2 Diabetes