Question: Is the relationship between chronic disease and increased COVID-19 risk consistent across different groups?
Takeaway: This paper indicates across multiple datasets that diabetes and heart disease are correlated with increased COVID-19 risk and mortality. This demonstrates a meaningful increase in disease risk is related to chronic illness.
Multiple individual analyses have indicated chronic disease increases the severity of and mortality associated with COVID-19 (1). However, the preliminary nature of the data, and the fact that the apparent prevalence and mortality rates have differed significantly across samples, increases the possibility that individual samples may not be representative of all COVID cases. This April 2020 paper analyzed multiple existing studies to assess the strength and consistency of the relationship between chronic disease and increased COVID-19 severity and mortality among infected patients.
The authors found three chronic conditions significantly increased risk of COVID-19. Cardiovascular disease (CVD) and hypertension increased risk of severe disease among infected patients with an odds ratio (OR) of 2.92 and 3.84, respectively. The CVD studies were notably consistent, exhibiting relatively little variance in effect size across studies (I^2 = 3.5%). Chronic kidney disease more than doubled risk of severe COVID (OR 2.22). Diabetes had a similar effect size to the other conditions, with an OR of 2.61 for severe disease.
The tables below show forest plots summarizing the studies surveyed.
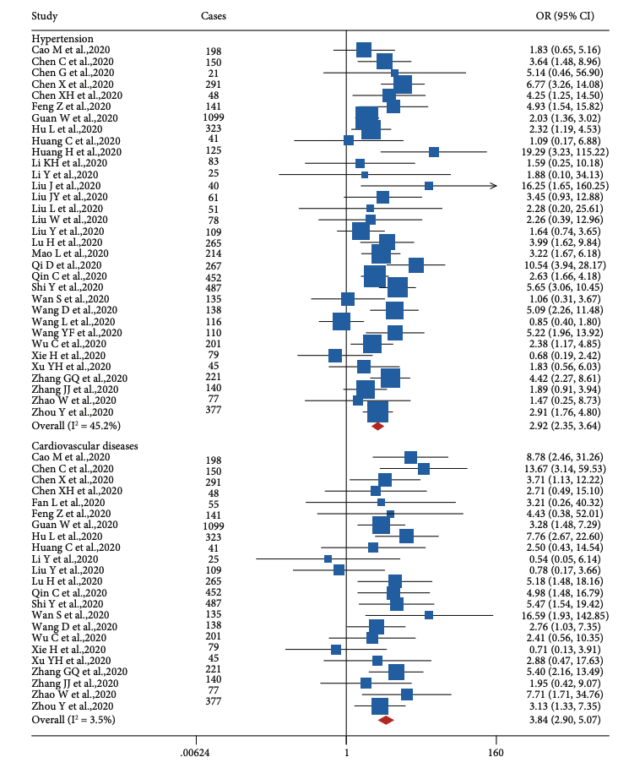
Figure 1: Forest plot of the associations between hypertension and COVID-19 severity, and cardiovascular disease and COVID severity, among infected patients
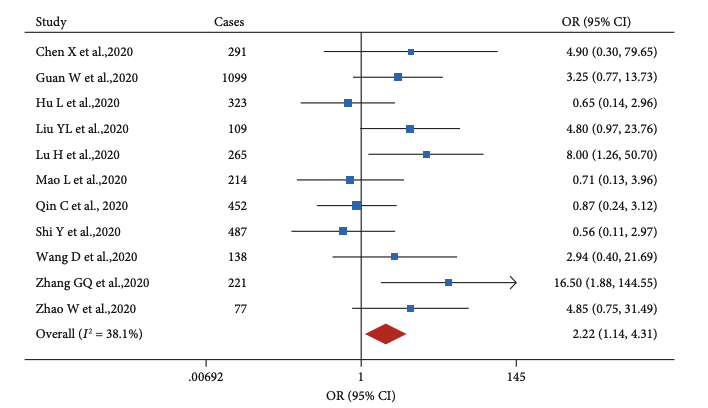
Figure 2: Forest plot of the associations between hypertension and COVID-19 severity, and cardiovascular disease and COVID severity, among infected patients
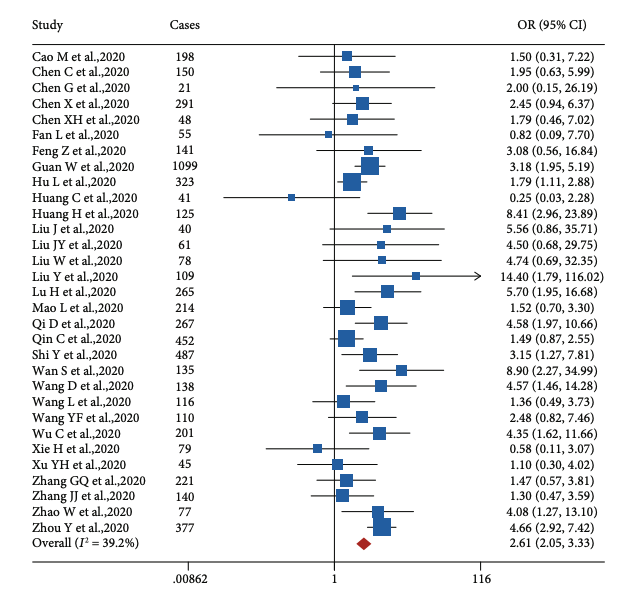
Figure 3: Forest plot of the associations between hypertension and COVID-19 severity, and cardiovascular disease and COVID severity, among infected patients
The authors note acute cardiac injury and acute kidney disease are both prognostic of severe COVID among hospitalized patients and may directly contribute to mortality. A significant share of COVID patients develop cardiovascular and/or renal complications (2); this pattern is similar to that seen in the SARS epidemic, in which acute kidney injury was a strong predictor of mortality. Acute liver injury, as indicated by elevated AST and ALT levels at baseline, is also predictive of COVID-19 disease severity and mortality (3). The mechanism by which COVID-19 causes acute kidney, liver, and cardiovascular injury, or exacerbates underlying injury is not completely understood but may be related to the cytokine storm (4), hypoxia (5), infection of ACE2-expressing tissues (6), or drug-related toxicity (7). Patients with preexisting conditions that affect these same organs may be more susceptible to these acute injuries and thus to the more severe forms of the disease.
The link between diabetes and COVID-19 is similar in consistency and magnitude to that seen in the SARS and MERS-CoV epidemics. In these previous coronavirus-derived conditions, both diabetes and hyperglycemia independently predicted increased disease severity and doubled the risk of complications and/or death (8). Diabetes has been linked to impaired outcomes in a variety of respiratory conditions (9), but the magnitude of these effects suggests additional disease-specific complications.
The authors conclude a “strong correlation” exists between the severity of a COVID-19 infection and preexisting metabolic (cardiovascular disease, kidney disease, diabetes) illness. Five potential mechanisms are provided in summary:
- SARS-CoV-2 attacks organs that are already negatively affected by these conditions and more susceptible to organ failure.
- Impairments associated with metabolic illness may prevent an effective immune response.
- Certain drugs currently being tested to treat COVID-19 can cause organ damage (including chloroquine, ribavirin, and lopinavir).
- Acute respiratory distress can cause hypoxia and cause further organ damage.
- Secondary infections provide yet another avenue for organ damage.
These and other mechanisms may explain why, across a variety of populations, individuals with chronic conditions are more likely to experience increased severity or death with COVID-19.
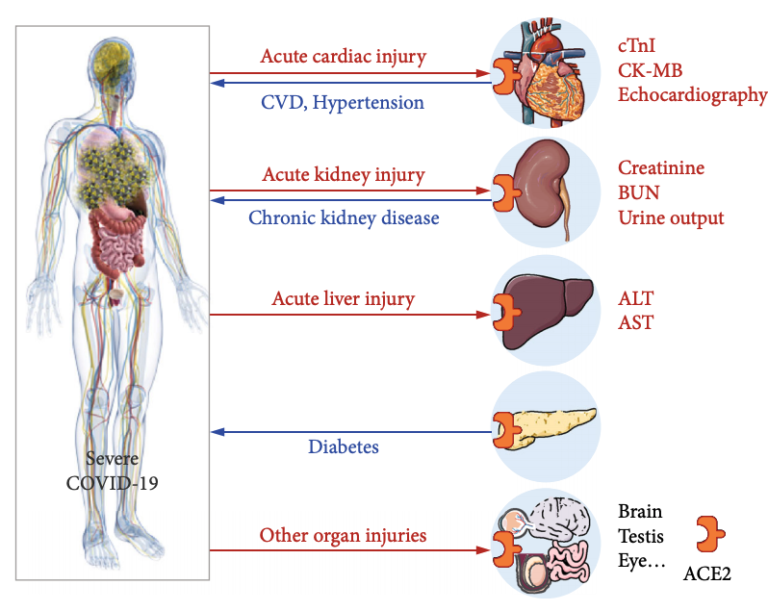
Figure 4: Summary diagram provided by the authors. CVD, hypertension, chronic kidney disease, and diabetes all increase COVID-19 severity, while severe COVID-19 leads to damage to the cardiovascular system, kidneys, liver, and other organs, all of which express ACE2. This suggests COVID-19 infection may trigger a vicious cycle among patients with existing disease in these organs.
Notes
- Clinical features of patients infected with the 2019 novel coronavirus (COVID-19) in Shanghai, China; Epidemiological and clinical features of 291 cases with coronavirus disease 2019 in areas adjacent to Hubei, China: A double-center observational study; Detectable serum SARS-CoV-2 viral load (RNAaemia) is closely associated with drastically elevated interleukin 6 (IL-6) level in critically ill COVID-19 patients; Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China; Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: A systematic review and meta-analysis; Hypertension and its severity or mortality in Coronavirus Disease 2019 (COVID-19): a pooled analysis
- Left ventricular performance in patients with severe acute respiratory syndrome: A 30-day echocardiographic follow-up study; Altered lipid metabolism in recovered SARS patients twelve years after infection; SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS; Acute renal impairment in coronavirus-associated severe acute respiratory syndrome
- Clinical characteristics of coronavirus disease 2019 in China
- Advances in the research of cytokine storm mechanism induced by corona virus disease 2019 and the corresponding immunotherapies
- Hypoxia signaling in human diseases and therapeutic targets; Hypoxia and hypoxia-inducible factors in kidney injury and repair
- Immune-epidemiological parameters of the novel coronavirus – a perspective; Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes; Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis
- Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro; Chloroquine cardiomyopathy with conduction disorders; Fatal cardiomyopathy associated with pegylated interferon/ribavirin in a patient with chronic hepatitis C; Tenofovir disoproxil fumarate co-administered with lopinavir/ritonavir is strongly associated with tubular damage and chronic kidney disease
- Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS; Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): A systematic review and meta-analysis
- Diabetes and COVID-19
Comorbid Chronic Diseases and Acute Organ Injuries Are Strongly Correlated With Disease Severity and Mortality Among COVID-19 Patients