Inertia has long been an understood reality of physics. Although he did not use the term “inertia,” Newton defined it as: “a power of resisting by which every body, as much as in it lies, endeavours to persevere in its present state, whether it be of rest or of moving uniformly forward in a right line.” (1)
From our school physical-science courses, we know the concept of inertia with more modern and simple language: “A body at rest or motion will stay at rest or in motion until acted upon by an external force.”
We often are unaware of this immutable concept because we ignore its applications in real life; after all, inertia occurs naturally, is in operation everywhere, and affects everything: including that long-haul phenomenon we call “aging.”
Physical and Biological Inertia
Aging increases inertia. How it does this is both insidious and in many instances avoidable.
Watch an elderly person get up from a chair. Compare that to how a child effortlessly springs up from sitting on the floor playing. Compare that even to how a middle-aged adult stands from sitting in an office chair.
Looks different, yes?
The geriatric wrestles with gravity, leaning far forward, pulling with their arms against the arms of the chair, all with the intent to move their center of mass into a favorable position to allow them to stand with as little hip, knee, and ankle movement as possible, often with the aid of a mechanical chair to overcome inertia. They move like a prototypical old person. And that begs a couple questions. Why do we, those over 60, start losing the fight against gravity? Why do we become objects of greater actual and perceived inertia compared to our younger selves?
One obvious explanation relates to mass. A larger mass has more inertia than a smaller one and we, the over-60s, are heavier than we were in our 20s — most likely a lot heavier, as it has been noted that the average person gains about a pound of body weight (0.45 kg) per year up until about 70 years of age (2). That is more mass, much more, hanging on our skeletons, resisting our efforts to move. How common is this weight gain? Current statistics suggest that about 42% of our age group are “obese.” Added to the 31% categorized as “overweight,” that means that 73% of people over 60 are affected to the point of creating a health or functional problem.
Most people generally associate fitness with being leaner; being skinner; being less fat. You can decide you don’t want to be fat and take action at any point of your life. However, life is not a pretty, straight line of perfection, it’s often a bit chaotic, and the weight can creep on without notice until one day you look in the mirror and think, “Who is that fat person?”
It can happen in your 30s. It can happen in your 60s. It can happen to anyone at any time, even if we know better. And that is absolutely OK; it can always be made better.
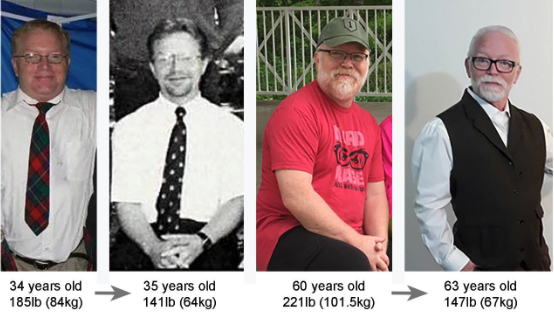
Figure 1: Being older does not mean weight gain is permanent; we can reduce inertial accumulations effectively at any age. The author is just like everyone else, life’s obstructive challenges and the call of the perfect donut are powerful impediments that can be overcome.
But weight gain is only one of many contributors to added inertia in the aged. It is also the composition of this weight gain that is problematic; older individuals tend to gain fat, not muscle. In fact, we tend to lose muscle with the passing years, even as we gain weight.
Atrophy, the loss of muscle cell and whole muscle size, compromises and diminishes the amount of contractile force we can generate. At the destructive end of prolonged atrophy during aging, sarcopenia, the progressive loss of muscle cells, occurs (3). Less mass and fewer cells means lesser muscle function. Up to a third of all people over 60 appear to be affected by sarcopenia (4). Atrophy and sarcopenia are directly associated with “frailty,” a medically defined term indicative of the vulnerability of the elderly to stressors that increase the risk for poor health outcomes, disability, and mortality (5).
So, the residual fat mass we have accrued over our lifespan coupled with less muscle to move it results in more of our remaining functional capacity being needed to simply stand up. A basic air squat may be near maximum ability, or supra-maximal, for many older folks. Greater relative inertia, via less force-generation capacity, means getting moving is simply harder for the aged. But again, there’s more.
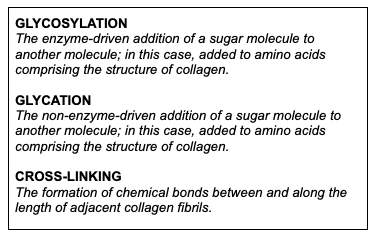
Most of our joints are built to reduce friction, to stretch and bend with ease, and to support and facilitate movement. But as we age, the collagen that comprises the ligaments and tendons of those joints changes. The amount of glycosylation and cross-linking in our collagen increases. The once elastic and motile tissue becomes stiffer and more brittle (6). By definition, “stiff” means “not easily bent,” and if we compare the range of motion between young and elderly subjects, we find that this has a profound real-world expression in a significantly smaller range of motion in the oldest of us (7):
In the aged, any increase in resistance to bending of the joints adds to the effects of increased body mass and reduced muscle mass in creating an amplified relative inertia. It is legitimately harder to move through any range of motion.
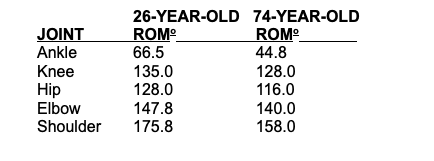
Figure 2: The author at a national event at 20 (left, 56-kg class) and at an international event at 60 (right, 77-kg class). The complete range of motion is smaller (loss indicated in red), and achier 40 years later, but the movement can still be done with correct technique and through a relatively complete range of motion.
This set of circumstances is problematic beginning in those over the age of 50. Not being able to sit down on the floor then stand up without using support points (hand, forearm, side of leg, etc.) during the process seems to be strongly associated with all-cause mortality in the subsequent six years (8). A simple test of range of motion, basic strength, and balance points to a catastrophic outcome for the least fit of us over 50. It might seem silly to predict mortality with a test measuring the ability to stand up, but the data from other studies provide corroborating evidence AND a glimpse into the magnitude of the problem. An estimated quarter of people over 60 have some degree of clinically diagnosed mobility problem (9). Over half of individuals over 65 in the US have difficulty stooping, bending, and kneeling (10). In several studies of those between the ages of 65 and 88, loss of mobility was strongly associated with all-cause mortality (11,12,13).
It is apparent that the inability to overcome inertia in the strict physical sense has dire ramifications. But there’s even more to the picture.
Perceptual Inertia
The perception of pain — simple aches or any other pain — changes with advanced age. The mechanism is poorly understood if understood at all, but the functional outcome is that over 50% of the population over 65 report activity-limiting pain, and that number goes up to over 80% in those in residential-care facilities (14). Of those over 65 who do report chronic pain, a whopping 69% classify the level of pain to be severe or greater (15). Achy joints are not a stereotype, they are a fact of life.
Stiffer, reduced range of motion, more pain with movement or even while just sitting around? This is where the physical world crashes into the behavioral world. Pain is not just physiology at work, it has a significant psychological component.
Trainers need to realize that scaling and movement modifications are absolute necessities when beginning training someone over 60. They need to understand that baseline pain and pain induced by acute movement are a reality; “of course it hurts when I do that; it hurts just to stand up.” But that doesn’t mean that the elderly cannot be fully capable of virtually any physical task when prepared for it logically, progressively, and over time.
Pain management is a complex physiological and behavioral topic within the medical community, and it is not a new one. The oldest joke the author knows was learned from seeing Danny Thomas at the Horseshoe Casino in the mid-sixties.
“I went to a doctor and said, ‘Doctor, Doctor, my arm hurts when I do this.’ Doctor told me, ‘Don’t do that.’ Then he handed me the bill.”
Although corny and not particularly accurate, it’s exactly what most of us who hit advanced age do when our perceived pain levels increase from the plethora of reasons life throws at us. If it hurts to do a full–range-of-motion squat, we modify our movement behaviors to strategies that do not require full-range-of-motion squats. We avoid movements or conditions that we associate with being painful. Avoidance then begets a change in self-belief. “It aches to do that” leads to “I won’t do that to avoid aches” and then that leads on to the mindset “I can’t do that, my body is broken.”
This plays directly into changing our overall lifestyle. Belief that the body is broken, worn out, and incapable from age decimates our engagement with virtually anything that requires movement. We become sedentary, the proverbial couch potato, with few if any interactions with the world.
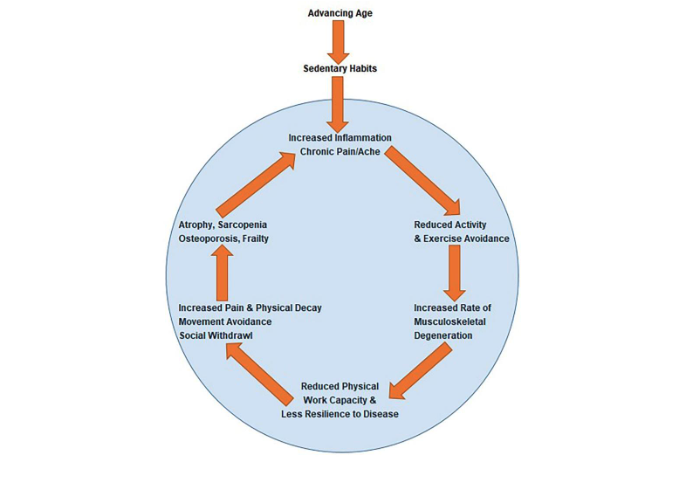
Figure 3: The Vicious Cycle of Aging While Sedentary. Essentially, things hurt, and as a result, we stop moving. This may transiently reduce aches and pains, but it also erodes our functional capacity. Further, it allows muscles, tendons, ligaments and bones to become smaller, weaker, and more brittle — and they still ache in inactivity, probably more. Then we descend into an ever more severe spiral through the cycle until loss of independence is a certainty.
It is a difficult concept for the older individual to accept. It is easier to explain our functional limits and decay through the notion that we are broken, the inevitable result of “wear and tear,” bad genes, or just bad luck. But really, the majority of us are broken only if we accept or believe convention and simply, voluntarily, stop.
Social and Behavior Inertia
About 55% of the over-60 population categorize themselves as “lonely,” often as a reflection of their lack of mobility beyond home and the easy chair. And we don’t give this outcome much thought. But we should.
The loss of function, the increase in perceived pain, the comfort of limiting range of motion and avoiding activities that may increase aches, even transiently, and the resultant lack of activity becomes and is considered unavoidable and the new normal for the rest of our lives. Societal and cultural influences and stereotypes reinforce resignation to and acceptance of being old and feeble. When governmental and health-professional organizations say that walking or gardening — or any random movement — is enough if you do it often enough to accumulate an arbitrary number of active minutes mathematically associated with a loose collective of “risks,” why would the general public disbelieve them?
Even considering getting in just enough movement to reduce disease risk (governmental and medical recommendations), how many over-60s get enough? Considering that about half are completely sedentary (16) and only 26% meet or exceed those guidelines, we aren’t faring very well. Three out of four of us are failing. But even if we all did meet activity guidelines, that is not enough to maintain a robust physical capacity and range of motion, or defeat the atrophic, sarcopenic, fat-accumulated, connective-tissue-stiffened, and pain-limited inertia of age. Only about 8% of us actually do exercise and train enough for that (17).
But there’s good news — well, it’s not news; we’ve known but ignored it for decades — we don’t have to become the prototypical decrepit old person. While low levels of miscellaneous physical activity may aid in staving off some disease (an admirable goal in itself), the acquisition of even moderate amounts of fitness, through consistent and progressive exercise and training, can provide for longer-term functional independence. We can fix our decayed fitness levels, we can fix our inertia-increasing body mass, we can mute aging’s amplified pain perception, and we can fix some, but not all, of the age-related biochemical changes that alter our architecture and metabolism. Aging does bring with it some inevitable decay — an estimated 3% reduction in physiological function per decade after 40 — but that number is only relevant if you quit moving. It applies if you give in to inertia permanently, become comfortable in the idea that sedentarism and dependency is the norm for the aged, and premature death is something that happens to other people.
Getting to the gym and training to improve fitness can slow many of these processes. Being fit can’t truly prevent disease, BUT it provides the resilience to maintain high function during disease, facilitates convalescence, and augments speedy recovery.
But this is where another powerful inertia manifests: the inertia of inaction. Over 70% of people 60 or over do not plan to make any changes in lifestyle habits; activity, exercise, diet, or otherwise (16).
Overcoming Inertia
It should be obvious, and every trainer and coach should be cognizant that the aging population is a multifaceted and compounding problem of literal and figurative inertia. We hear it again and again: “I too old, I can’t do that any more,” “I’m too old to start,” “I’m too far gone to get better,” “I was never good at sports,” “I HATED P.E. in school,” and so many more are given as the rationale for living life on the couch. The elderly are conditioned to accept, willingly and often aggressively, physical decay and limitation of mobility.
But we can do it: We can move, we can exercise. All of us.
Think about Clark Holland and Joke Dikhoff, the oldest male and female competitors in the CrossFit Age-Group Semifinals. Both are over 70 and competing against much younger athletes for spots at the CrossFit Games, where the average age in the oldest age group (65+) is 65.2 years men and 66.9 for women. Think about Katsuji Okiura, who at 71 years of age and 163 lb (74 kg) did a full-range-of-motion squat with 402.3 lb (182.5 kg). If we choose to strive to challenge and defeat inertia, we can.
Some may read this and say hand-picked examples can’t prove anything. Then think about all of those older CrossFit Open participants with no preconceived notion of becoming a Games athlete who also completed the workouts, either as prescribed or scaled, and performed every movement properly. These are just regular folks who once yielded to inertia but now strive to make the most of life by getting to a CrossFit affiliate. They know that no matter how they were shaped or how low fit they were, that they could be, can be, will be fitter, healthier, and better for themselves and their families for longer.
We can do a lot in old age; however, many seniors, masters, geriatrics, elderly, or whatever term you use to describe the over-60 population can feel limited, prevented from exercising or playing sports due to the presence of disease:
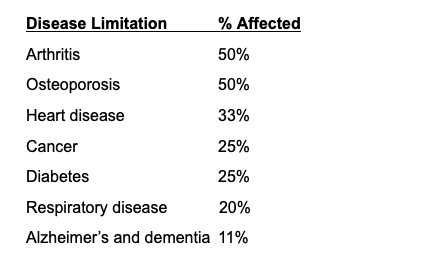
It may seem odd to the CrossFit athlete — because we have the relevant information — that disease conditions that can be improved with exercise training are used as a reason to avoid exercise. But the older diseased population generally does not have proper fitness advice, even from their physician. Less than one in three older patients have discussed exercise with their primary-care physician (18). Further, getting fitness information out to the elderly has historically been a challenge and frequently ignored by the intended recipients. Gyms have been generally reliant on word of mouth to get their offerings for the aged disseminated to the public. That’s not an extraordinarily efficient means of information delivery or marketing. Over the past decade, technology use by the 60-plus population — if ownership can be indicative of use — has increased, with 55% now owning a computer, 61% owning a smartphone, and 45% having a social-media presence of some type. Connecting with the aging population is becoming viable, and digital access may provide a means to convince them to get to the gym.
But there are two other limitations that are very relevant here:
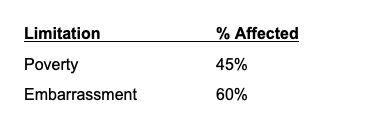
The first is a problem across all social domains. It is a commonly held conception that retirement is a cozy and comfortable time spent not working and doing the things that the retiree has always wanted to do. With retirement household annual income averages ranging by state from $43,601 (DC) down to $22,998 (KS), maybe this is a reality for some. But if, as data suggests, 45% of the population over 60 have annual incomes below the level indicative of poverty ($13,590 for an individual in the US, according to Health and Human Services Guidelines), there is very little room for discretionary spending on gym memberships, or anything else. But there are provisions in Medicare (supplemental programs) that can help defray the cost, IF the gym participates in the program. We in the fitness industry have to be creative in order to serve as many people over 60 as we can without them, or the trainers, going broke.
Finally, there is the one limitation that is ubiquitous across age groups but is even more manifest in the 60-plus population: embarrassment. Whether it is embarrassment from being out of shape and being unable to do even the simplest of exercise movements, embarrassment from having a disease condition, embarrassment from body size, embarrassment from lack of knowledge, embarrassment regarding affordability, or embarrassment from just being old, this is a powerful barrier.
Some of this is driven by misunderstanding of what exercise and training actually is, complete lack of awareness of the concept of scaling, and a misbegotten belief that they will be expected to be an “athlete.” Our message to over-60s must be clear and persuasive, clearly articulating an understanding of their age-specific issues, and accepting and catering to their individual needs:
“Our understanding is that the needs of Olympic athletes and our grandparents differ by degree, not kind. One needs functional competence to stay out of the nursing home. The other one wants functional dominance to win medals.” —Greg Glassman
An outgoing, knowledgeable, and patient trainer or coach and an overwhelmingly supportive gym community can make massive changes in the fitness and quality of life for any aging and sedentary person. To make that happen, we have to remove the inertial dampers. We need to instantiate self-belief in the over-60s regarding their abilities. We need to create first-steps programs that tread the fine line of acceptance and challenge. Those tiny behavioral and social steps, tiny challenges leading to tangible rewards, open the door for greater physical development in the aged, enabling broader participation and greater immersion in the world around them.