“Eat less, move more.”
This has been the standard response to the obesity problem for decades.
“Now we know it is not that simple,” writes Alessio Fasano, M.D., and co-author Susie Flaherty in their 2021 book, “Gut Feelings: The Microbiome and Our Health.”
The authors point to a number of environmental factors that influence the condition, including “sleep deprivation, disruption to circadian rhythms, chronic stress, changes in food composition, labor-saving devices, drugs (including antibiotics), and endocrine disruptors” as well as socioeconomic factors.
They also reference a study identifying more than 250 genes associated with obesity, and report that “80 percent of the approximately 200 genetic loci” — a locus is the physical location of a gene on a chromosome — “are primarily expressed in the brain.” The pair cite work by Lee Kaplan, M.D., the director of the Obesity, Metabolism & Nutrition Institute in Massachusetts, positing obesity as the result, in part, of a genetic response to environmental factors.

In their work, Fasano and Flaherty add another variable to the mix: the gut microbiome, the ecosystem of microorganisms in and on the human body. However, rather than implicating the microbiome as a direct cause of obesity, they discuss its potential role as a “transducer” of those environmental signals that influence how the brain regulates metabolism.
“When we look at the gut microbiome, it is uniquely positioned, physiologically speaking, between the environment and the host with the capacity to mediate those signals to the brain,” the authors write.
In other words, the brain listens to the gut.
“Even though they appear so different in their structure and function, developmentally speaking, the brain and the gastrointestinal system are interrelated,” the authors write. In fact, the gut is sometimes referred to as the “second brain” due to the presence of a system of nerves, neurons, and neurotransmitters located along the entirety of the digestive tract.
If that’s true, then perhaps manipulating the gut microbiome can alter how a genetic predisposition to obesity is expressed.
Fasano and Flaherty point to a 2005 study by Jeffrey Gordon. Gordon and his team of researchers at Washington University demonstrated that “mice with a gene mutation resulting in obesity had a different mix of gut bacteria than their lean littermates, even when they shared the same diet.”
Researchers then transplanted the gut microbiota from the genetically obese mice into germ-free normal mice — who then “became fatter compared to the germ-free mice that received the gut microbiota from lean animals.”
In subsequent studies, Gordon transplanted gut microbiota of twin human girls — one lean and one obese — into germ-free mice. The mice who received the microbiota of the obese twin demonstrated increased body fat and metabolic abnormalities, while the those who received the lean twin’s microbiota were “lean and metabolically healthy” despite consuming the same amount of food.
“This natural microbiome transfer experiment demonstrated that the lean donor’s microbiome performed functions missing from the obese donor’s microbiome, which seemed to prevent obesity,” Fasano and Flaherty write.
So, if our microbiome can influence genetic expression, what influences the microbiome? Very likely, diet.
“Changes in diet can change microbiome functions even if the microbiome composition remains the same,” our authors continue.
Fasano and Flaherty do not indicate how specific foods or diets might affect the microbiome, noting only that “there are many lifestyle factors that can ultimately affect the composition and function of the gut microbiome, which is highly influenced by the quantity and, more important, by the quality of the food we ingest.”
But other researchers have. In a 2021 clinical trial, researchers from the Stanford School of Medicine tested the effects of two 10-week diets: one high in fermented foods and the other high in fiber. The former resulted in increased microbiome diversity and decreased inflammation; in the latter, microbiome diversity remained stable.
“This is a stunning finding,” said study author Justin Sonnenburg, Ph.D. “It provides one of the first examples of how a simple change in diet can reproducibly remodel the microbiota across a cohort of healthy adults.”
It’s the kind of research we need more of. As Fasano and Flaherty noted, replicating the kind of study Gordon performed with mice is impossible with humans, as microbiota transfers in humans can’t be done in a germ-free setting. Additionally, the human response to the presence or absence of certain microorganisms in the gut is vastly varied.
The authors quote Kaplan: “‘The primary discovery work in the microbiome, working with probiotics, prebiotics, etc., has got to be in the human.’”
They also compare obesity to cancer to indicate the necessity for a personalized approach to treatment.
“Obesity has all the levels of complexity that cancer has in cell growth and differentiation in cancer pathology … different therapies are needed because the mechanism to create cancer as the end result is different in each individual. A similar personalized approach is needed to treat obesity,” Fasano and Flaherty write. “The lesson that the microbiome seems to be teaching us again and again, that there is no ‘one size fits all’ in treatment, is also reflected in obesity.”
But even if there’s no “one size fits all” when it comes to a menu for combating inflammation and obesity, we can at least agree the best interventions fall under the umbrella of quality. And if quality is the most influential factor in how food intake affects the microbiome — which in turn might affect gene expression — then we’ve got you covered:
“Eat meat and vegetables, nuts and seeds, some fruit, little starch, and no sugar. Keep intake to levels that will support exercise but not body fat.”
This has been CrossFit’s nutrition recommendation since 2002, and it allows plenty of room for variation — in fact, the CrossFit Nutrition I Course explains in detail how to follow it regardless of dietary restrictions, food allergies, or preferences.
It’s certainly possible that future research may reveal ways to tweak diet to alter the microbiome, and consequently, body composition. But it’s sort of like buying weightlifting shoes before you can squat below parallel.
Master the basics — eat meat and vegetables, nuts and seeds, some fruit, little starch, and no sugar — then fine-tune them accordingly.
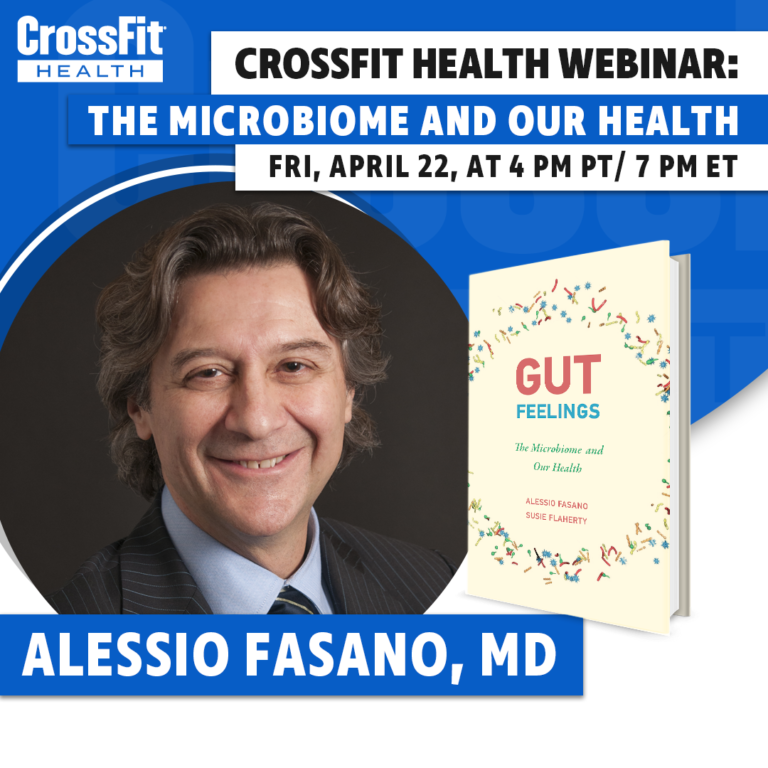
On Friday, April 22, at 4 p.m. PT/5 p.m. MT/7 p.m. ET, Alessio Fasano, M.D., will join Mike Giardina for a live Q&A-style webinar focusing on the connections between the human microbiome and health. Learn more and register here.
Comments on Obesity and the Microbiome
Does anyone still doubt natural herbs? I've seen the great importance of natural supplements and the wonderful work they have done in people's lives. I wonder why people still spend their money on surgery, injections and drugs each time they are sick. Natural herbs can cure all kinds of illness. +2347063982352 drofenmu@gmail.com,
Obesity and the Microbiome
3