The following excerpt is reprinted with permission from The Trouble With Medical Journals (Taylor & Francis, 2000).
Medical journals have existed for 200 years, but will they continue? The answer must be that they will if they do something that people value and that isn’t done more effectively or more cheaply by some other means. This iron law of economics applies to everything. So what do journals do that people value and who are their customers?
Scientific journals exist primarily to disseminate and record science, but many medical journals, although they include science, have been about more than simply recording science. Around 40 medical journals were begun in Britain between 1640 and the end of the 18th century (53). None survives. Journals are like restaurants (or any small business): many start, few survive long term. Another 100 journals began in Britain between 1801 and 1840, and one of these — the Lancet, which began in 1823 — does survive. The Lancet has always been a fascinating, energetic journal, reflecting its aggressive, combative, crusading and controversial founder, Thomas Wakley (54). At the prompting of his radical friend William Cobbett, he started the Lancet as a 28-year-old general practitioner with a mission to ‘inform and reform’. That formula persists today, and perhaps the current editor, Richard Horton, who became editor at 33, is closer in spirit to Wakley than any other Lancet editor has been.
Wakley from the beginning produced the Lancet for ‘the profession at large’ rather than ‘the eminent few’. Doctors outside the main cities in Britain were, he observed on the first page of the first issue, ‘almost without the means of ascertaining its [medicine’s] progress’. An important feature of his journal was reports on lectures given by prominent doctors in London. The doctors charged for these lectures and objected to them being reproduced in the Lancet without permission. There were many legal actions. Wakley also provided medical news, case descriptions and non-medical articles that would entertain and instruct the general public as well as medical practitioners. So there was little or no science, entertainment was a specific aim, and the journal was aimed at the public as well as doctors.
But Wakley’s other aim — and perhaps his primary aim — was reform, and in wildly intemperate language he attacked nepotism, incompetence, quackery and corruption, all of which were rife in early 19th century British medicine (and perhaps still are). Libel actions were ‘plenty as blackberries’, but Wakley had hit on a formula that was commercially acceptable. We can easily imagine a provincial but progressive practitioner — like George Eliot’s creation Dr. Lydgate in Middlemarch — reading the Lancet not only to find out what was new and to improve his knowledge but also to be amused and excited by Wakley’s latest attack on the establishment.
Eliot does not tell us whether Lydgate read the Lancet, but the traditional, and incompetent, doctors suspect him of doing so.
‘Hang your reforms!’ said Mr. Chichely. ‘There’s no greater humbug in the world. You never hear of a reform, but it means some trick to put in new men. I hope you are not one of the Lancet‘s men, Mr. Lydgate — wanting to take the coronership out of the hands of the legal profession: your words appear to point that way.’
‘I disapprove of Wakley,’ interposed Dr. Sprague, ‘no man more: he is an ill-intentioned fellow, who would sacrifice the respectability of the profession, which everybody knows depends on the London Colleges, for the sake of getting some notoriety for himself. There are men who don’t mind about being kicked blue if they can only get talked about.’
(I’ve heard almost exactly those words said about Richard Horton.)
The BMJ, which doesn’t merit a mention in Middlemarch, got off to a much duller start (9). It was founded in 1840 as the journal of the Provincial and Medical Surgical Association, which was formed by Charles Hastings, a Worcester doctor, and eventually became the British Medical Association (BMA) (55). The first issue of the Provincial Medical and Surgical Journal was 16 pages long and the longest items were the editor’s introductory address and a report of the annual meeting and dinner of the association’s eastern branch. What could be more boring?
The editors announced that the aims of the journal were the same as those of the association — the promotion of the medical profession. There were clinical papers, case notes, a summary of a medical reform bill and some book reviews. At least one of these was lively: Charles Waller’s Practical Treastise on the Function and Diseases of the Unimpregnated Womb was described as ‘200 scanty pages of commonplace professional twaddle’. The editors also took a swing at the Lancet by boasting that they had ‘received as many advertisements (in proportion to the quantity of letter press) for our first number, as the most popular Medical Journal of the present day after 17 years of existence’. This was empty boasting: advertisers are always attracted by novelty — at least briefly.
(Anybody who would like to read this fascinating material for themselves will soon be able to do so courtesy of the National Library of Medicine in Washington. It is digitizing the whole of the BMJ and many other journals. Stephen Lock, my predecessor, told me, however, that the only thing that was interesting in old BMJs was the advertisements — and they are not being digitized.)
The BMJ thus shared the aim of the Lancet in wanting to inform practitioners, and it was in some ways a development of the Midland Medical and Surgical Reporter, which recorded pathological observations made in provincial hospitals and other aspects of medicine and medical practice in the Midlands. But even with its role of informing it can be seen that its bill of fare was less attractive than that of the Lancet, which was including up to the minute lectures from leading practitioners. In addition, the BMJ lacked the reforming zeal of Wakley’s Lancet. A description of the annual dinner of the eastern branch would not make such good reading as an attack on the wickedness of a leading London practitioner. It’s not surprising that while the Lancet flourished commercially the BMJ struggled for most of its first 25 years.
The Lancet is highly unusual in not being linked to a medical organization. All the other ‘big five’ medical journals are owned by medical organizations. The Annals of Internal Medicine is owned by the American College of Physicians, the BMJ by the BMA, JAMA by the American Medical Association, and the New England Journal of Medicine by the Massachusetts Medical Society. Journals owned by associations can degenerate to being simply mouthpieces of the association, suppressing anything that for whatever reason doesn’t suit the aims of the association. Journals tend to fight with their owners and my (wholly biased) judgement is that journals flourish when they are most independent of their owners.
One issue that seems to be constantly debated in medical journals is how political they should be (56). ‘Politics’ says Chambers Dictionary is ‘the art or science of government, the management of a political party, political affairs or opinions, manœuvring and intriguing, policy making, as opposed to administration, the civil rather than the military aspects of government.’ Rudolf Virchow, a great 19th century doctor and editor, famously said that medicine was ‘a social science, and politics nothing but medicine on a grand scale’. For him and many others — including Wakley and Ernest Hart, the leading 19th century editor of the BMJ — it made no sense to think of an ‘apolitical’ medical journal. There is also the argument that being ‘apolitical’ is in itself a political position — usually one that supports the status quo.
Nevertheless, a great many readers of medical journals object strongly to them being political. Tony Delamothe, deputy editor of the BMJ, wrote an editorial asking ‘How political should a general medical journal be?’ and quoted a correspondent who wrote in response to a letter describing the pattern of injuries suffered by Palestinians in the Israeli occupied territories, ‘I am terribly sorry to learn that … the British Medical Journal has become a politically motivated journal … I hope that this would be the first and last political letter published in this journal’ (57). I can’t help observing that if the correspondent imagined this letter in 2002 to be the first political letter to appear in the BMJ he’d either never read the journal before or had a very strange idea of what constituted a political letter.
Another correspondent wrote in response to Delamothe’s editorial (58):
The problem with medical journals entering into politics is that it subjects them to the accusation of bias … You may disagree with your government’s stance on [the coming war in] Iraq, but that disagreement has no place in a medical journal … Cataloguing the health effects of weapons of mass destruction or debating (honestly and fairly) the merits and demerits of smallpox vaccine are appropriate for the pages of the journal. It isn’t appropriate, however, for you to use your influential position to trumpet your own political biases. Continuing to do so only discredits the journal. How will we know you haven’t rejected papers simply because their findings disagree with your politics?
In the 19th century it probably seemed impossible to separate medicine from politics. Life expectancy improved dramatically in the industrial world towards the end of the century not because of medical practice but because of improvements in sanitation and housing, reductions in poverty, better nutrition, the spread of education and other social developments. These are still the major influences on health and it wasn’t until antibiotics, other drugs and modem surgery were developed in the middle of the 20th century that medicine began to have some appreciable effect on how long people lived. It then began to be possible to imagine a general medical journal that would not be political. It would restrict itself to physiology, pathology and therapeutics. It wouldn’t stray into public health and the wider determinants of health.
When discussing the damage to health caused by tobacco, for example, this apolitical journal would restrict itself to material describing the effect of tobacco on the body and the steps that individual doctors might take to stop individual patients smoking. There would be no discussion of the price or promotion of tobacco or the malignant activities of the tobacco industry: these are clearly political issues. The journal would not even consider the availability of smoking cessation services or whether nicotine replacement therapy should be available on prescription, both issues that have been the cause of intense political argument in Britain recently. I wonder whether or not such a journal — where the editor watches with an eagle eye to exclude any political material — is even theoretically possible. Can medicine and politics be separated? I don’t think they can, but even if they could I can’t see the point. Any journal that wants to have any influence on health and medicine will have to deal with the political.
The real question is not whether a journal should be political but rather, as Delamothe asked, how political should it be? We at the BMJ were somewhat taken aback by the extensive coverage that the Lancet gave to the attacks on New York and Washington on 11 September 2001. This was clearly a major geopolitical event and there were many deaths. We carried news stories and first person accounts of being caught up in the attacks. The Lancet, in contrast, carried nine articles, several having what seemed to us tenuous links to health or medicine. Much of its coverage was similar to that in newspapers and the weekly news magazines.
This seemed to us a step too far. We felt the need to maintain a link with ‘health’. Thus we joined the debate on whether or not there should be an attack on Iraq but always within the context of what the casualties might be. Yet we published a piece that argued that the main reason behind the war was the need of the United States to gain access to cheap oil (59). The link to health was the possible effects of this on global warming with its undoubted consequences for health. The author of this piece — Ian Roberts, a professor of health policy — also pointed out that many journals that tried to be ‘apolitical’ were publishing a great deal on bioterrorism. This meant, argued Roberts, that they were being political because bioterrorism was a minor influence on health but a major part of the argument for going to war (60).
When we published Delamothe’s editorial we held a vote on our website in which we asked readers how much space we should devote to political issues. In all 366 people answered and in comparison with current coverage, 45% wanted more or much more coverage, 31% the same and 22% less or much less.
The possible functions of journals are thus informing, reforming, disseminating science, educating, providing a forum for a community to debate the issues of the day, entertaining and making money. I believe that a good journal will do all of these things, trying always to maintain a balance. Some journals do perform all the functions, but most don’t. Many current journals, particularly specialist ones, are primarily concerned with disseminating science, informing in a small way (with occasional editorials) and making money. They don’t see it as their business to reform and the idea that they might entertain they find silly. Medical journals, they believe, should be serious. Unfortunately, many — even if they don’t intend to be — are pompous. They fail to understand that humour well used is not only entertaining but also a powerful tool for informing, reforming and educating.
Many also imagine that journals are about changing what doctors do, bringing their practice up to the minute. That’s what I thought myself when I first joined the BMJ and many, including journal editors, believe that journals are a major engine — perhaps the major change and improvement. But it isn’t like that at all. We have overwhelming evidence that there is a substantial gap between what the published evidence suggests is best practice and what doctors and other healthcare workers do. The influential Institute of Medicine in the United States labelled the gap ‘a chasm’ — and there is no reason to think that it is worse in the United States than in any other country (61).
Why don’t medical journals change practice? The main reason is that change is hard, involves many factors, and can rarely be achieved by words on paper alone (62). Sending practitioners written guidelines changes little (62, 63). Other interventions are needed in addition — for example, one to one meetings, feedback on performance, organizational change or sessions with people called in the jargon of marketing ‘opinion leaders’ (64). And guidelines give specific information on what actions to take with patients with specific problems. Journals, in contrast, contain a hotchpotch of different sorts of information, little of which is ‘actionable’. Even when the information seems to give a clear message on the best actions to take it would probably be unwise for a doctor immediately to take that action. Much of the evidence in medical journals is in evolution. It’s undigested. Much is shot down. Publication is not the end of the peer review process but a part of it.
David Slawson and Allan Shaughnessy, two American doctors who have taken a great interest in trying to help doctors through the jungle of medical information, have described a formula that helps assess the utility of information in various sources available to doctor (8).
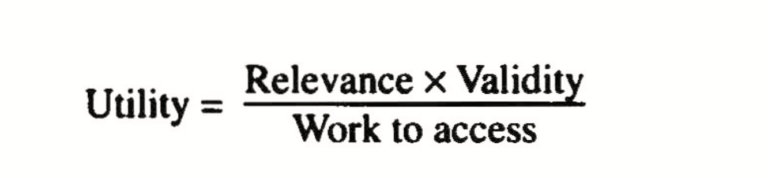
If we consider the original research in journals we can see that any given study is likely to be of limited relevance to any particular doctor. Some studies have high validity, but many do not. And the work to access the information in original research is high: it takes a long time to read research and critically appraising it is difficult and needs special skills that many doctors lack. So the usefulness of individual studies to a particular doctor at a particular time is low, but their usefulness overall may not be low. They need to be systematically combined with other studies.
Many studies have shown that when doctors have questions that they need answering they mostly go to colleagues, even though they may say that they use journals (65). Colleagues can give answers that are directly relevant. They are easy to access and (with luck) will provide valid answers.
After listening to a Ugandan PhD student describe the characteristics that made information useful to health workers in rural Uganda, I added ‘interactivity’ to the top of Slawson and Shaughnessy’s formula. This explains still further why doctors go to colleagues for information: they can discuss (an old fashioned word for interact) the question with them and get the answer clear in a way that can’t be done with a journal article. David Slawson says that ‘interactivity’ is simply a function of ‘relevance’ and ‘work to access’, not something independent. I’m unconvinced.
The thinking behind this formula has led various people, including the BMJ Publishing Group when I was there, to try and come up with ‘knowledge tools’ that will be more useful to doctors than journals. The BMJ Publishing Group has, for example, produced something called Clinical Evidence, a compendium of regularly updated, evidence-based (jargon for valid) answers to clinical questions on treatment commonly asked by doctors and patients (66). Clinical Evidence has been made available to all healthcare workers in Britain, 500,000 doctors in the United States and 300,000 doctors in Italy. It’s available not only in English but in Spanish, Italian, Russian, French, German and Japanese.
For a while I found myself wondering why we needed the BMJ and other journals when we had knowledge tools like Clinical Evidence. But it goes back to Wakley’s original formula of informing, reforming, debating and entertaining. At the BMJ we went as far — inspired by my days at the Stanford Business School — as developing a ‘mission statement’ (67). The journal had survived 150 years without one, but I believe it to be a useful exercise to define together what you are trying to do. How, otherwise, could you know if you were succeeding? Increasingly journals — along with hospitals, practices and many other medical institutions — have mission statements.
I thought that it would be useful to include our mission statement here. Such a statement should last for decades and every word in the statement should matter — but the thinking is often clear to those who devise it and less clear to those who read it. So I will explain the thinking behind the statement.
To publish rigorous, accessible and entertaining material that will help doctors and medical students in their daily practice, lifelong learning, and career development. In addition, to be at the forefront of the international debate on health.
To produce sufficient surplus to develop the primary mission and in good years to invest in the rest of the group and contribute to the activities of the BMA.
Publish means more than putting words and pictures on paper. It certainly includes putting words and pictures on screens but also creating talks, videos and meetings. If journals have a future then it is likely to be multimedia.
Rigorous: we might have chosen the word ‘scientific’, but the BMJ includes much material that is not scientific — and we wanted our news, views and even humour to be rigorous.
Accessible means not only readable but also easy to find and understand and attractive to look at.
Entertaining: we wanted reading the BMJ to be a pleasure, not a chore.
Material: we wanted constantly to broaden the range of things we published. We long ago moved beyond simply publishing research papers, but the journal has a long way to go with publishing more than words and pictures. Some journals are now beginning to include podcasts on their websites.
Help: if we could be helpful we would prosper. Sometimes we ‘preach at’, but we try not to do so too often. Being helpful certainly includes ‘bringing new and possibly uncomfortable material to the attention of doctors’, and it probably includes providing leadership.
Doctors and medical students: this means doctors and medical students everywhere, not just in Britain. We knew that the BMJ is read by many people who are neither doctors nor medical students, and we were pleased that they enjoyed the BMJ — but we thought it important to focus on doctors and medical students. By concentrating on helping them we would, we hope, help others.
In their daily practice: we aspired to be helpful to doctors and medical students every day, by providing information that would help them not only with clinical problems but also with issues like ethics, the law, science, education, communication, critical appraisal, improvement methods, management, statistics, economics and the many other subjects that modern doctors and medical students have to understand. The BMJ could not be in the business of teaching specialist skills to specialist groups because most of our readers do not belong to that specialist group, but we wanted to help doctors and medical students with the skills, both clinical and otherwise, that are important to them all.
Lifelong learning: to continue to learn throughout their careers matters greatly to doctors and their patients. The BMJ wanted to help them do this not only by providing material on medicine and science but also by providing material on learning and teaching.
Career development: many doctors and medical students are confused about their careers and the skills needed to develop them. The BMJ aimed to be an unequalled source of advice for doctors and medical students everywhere.
To be at the forefront of the international debate on health: the BMJ had ever since its beginning been international, but the World Wide Web and the dozen or so local editions of the BMJ offered unprecedented means of reaching out beyond Britain. The BMJ was concerned not just with medicine and healthcare but also with health. We might have chosen the word ‘lead’ instead of ‘be at the forefront of’, but that seemed too pretentious a step.
Debate is a crucial word for the BMJ. We wanted to be a place where almost every view can be expressed and follow the teachings of John Milton, the great British poet. ‘Give me,’ he wrote, ‘the liberty to know, to utter, and to argue freely according to conscience, above all liberties. Truth was never put to the worse in a free and open encounter … . It is not impossible that she [truth] may have more shapes than one … . If it come to prohibiting, there is not ought more likely to be prohibited than truth itself, whose first appearance to our eyes bleared and dimmed with prejudice and custom is more unsightly and implausible than many errors … Where there is much desire to learn there of necessity will be much arguing, much writing, many opinions; for opinion in good men is but knowledge in the making’ (68).
I found this guidance of Milton’s more useful than any other in my time as editor of the BMJ. There were many circumstances in which people were infuriated by what they read in the BMJ and wanted the words retracted and the author punished. Milton’s quote was useful to me then not only because I had it ringing in my ears but also because I sent it to the critics. Usually it shut them up.
To produce sufficient surplus to develop the primary mission and in good years to invest in the rest of the group and contribute to the activities of the BMA: the BMJ, like every other organization, has to think about finance. Members of the BMA tend to think that much of their subscription to the BMA comes to the BMJ — because the BMJ is what they see every week. In fact none of it does. Money flows from the BMJ Publishing Group to the BMA — over £9m in 2003. The BMJ itself is also profitable, with income from subscriptions, advertising and several other sources. Our financial mission was to be able to invest to develop the BMJ itself and also, when profits were good, to invest in the rest of the publishing group and in the activities of the BMA.
The BMA has now made clear, however, that it expects profits from the BMJ Publishing Group — and it is right that the owners should set the mission of the journal. They will destroy a journal if they interfere with day-to-day editorial decisions, but it’s surely right that the owners should set the mission, approve the strategy for achieving it and monitor progress with the strategy. I will return to this theme in chapter 12 on editorial independence, but nobody from the BMA told me what they wanted from either the BMJ or the BMJ Publishing Group. My predecessor simply told me, ‘make sure the journal comes out on time and don’t introduce American spelling’.
Partly because our mission statement was hard to remember, the BMJ also had a vision of what we would like to be:
To be the world’s most influential and widely read medical journal.
We didn’t want to be the world’s richest, biggest, most profitable or even most scientific journal; we simply wanted to be the world’s most influential and widely read medical journal. One snag with influence is that it’s hard to measure, but we kept trying to develop a score — without success.
While it’s important for an organization or journal to know what it is trying to do, it’s equally important for it to identify its customers — and I’m using the word in the broad sense of not just people who hand over money for what the organization or journal has to sell but also all those people who have to be satisfied if it is going to flourish. Another word is ‘stakeholders’. So, who are medical journals for?
The BMJ‘s mission statement mentioned doctors and medical students. These were the people at whom we aimed the BMJ, and we mean doctors and medical students everywhere. This would not have been the case when the Provincial Medical and Surgical Journal began. At some point — probably in the later part of the 19th century — the BMJ aspired to become an international journal. But perhaps initially it was ‘a showcase of British medicine’. I wanted it to be truly international, gathering material from everywhere. But we knew we had a long way to go. To many we were irredeemably (but sometimes attractively) British. Furthermore, some British doctors wanted us to stay firmly British and resented us publishing material that they did not see as directly relevant to them.
Other journals also aspire to be global, but none succeeds completely. Many journals, however, are very much national or regional. They distinguish themselves by understanding the issues of that country or region in a way that no international journal can match.
The mission statement of the BMJ Publishing Group (as opposed to the journal alone) mentioned groups other than doctors — ‘members, other health professionals, the scientific community and the public’. By members we meant members of the BMA and members of organizations with which we co-own journals, like, for example, the British Cardiac Society. Many journals are sent to members of medical organizations as part of their membership fee and those publications may put the needs of the members of that organization first.
Most journals are read predominantly by particular professional groups. Doctors read medical journals. Nurses read nursing journals. Health managers read newspapers, the Economist and perhaps the Harvard Business Review, but don’t really read anything that looks like a medical journal. There are some health professionals who read across the divide, but they are rare. Many people have observed that one of the barriers to improvement in healthcare is the professional tribalism. Wouldn’t it be marvellous if somebody could create a journal that crossed these professional divisions? Nobody has succeeded.
Wakley set out to create a journal that could be read by the public. He failed, but it was a bold idea. We live in a world where there is increasing evidence that health will be improved if doctors and patients work together as partners rather than in the traditional role with doctors as authority figures making decisions on behalf of patients (69, 70). This logic suggests that there should be publications that are aimed at both health professionals and patients. But then, as I’ve just written, nobody has yet succeeded in producing a publication for all those within healthcare let alone patients as well.
Those in health publishing have looked enviously at the Economist. It is a publication that started at about the same time as the BMJ and has broken out of the ghetto of its discipline. It’s also become a major international force with its readership numbered in millions, including United States presidents and other world leaders. Why couldn’t a medical publication do the same? Many have dreamt of a medical equivalent of the Economist — called perhaps ‘Health’ — but it is just a dream. Economics, like it or not, drives the world. Everything — war, politics, even football — can be legitimately and insightfully analysed using economic thinking.
But doesn’t health similarly encompass everything? The World Health Organization (WHO) famously defined health as complete physical, mental and social wellbeing — prompting one wag to suggest that it was thus achieved only at the point of mutual orgasm. Disraeli said that the health of its people should be the first concern of a government. Now the WHO’s Commission on Macroeconomics and Health, a commission mostly of financiers not health experts, has said that investment in health hastens economic development more than any other investment: health is not a benefit that comes from development but an engine of development (71).
Despite all this, those of us interested in health do not have a means to comment on the world in a way that brings fresh and exciting understanding in the same sense that economics can. We may deal with the eternals of birth, death, pain and sickness, but we are mostly preaching to each other. Some members of the public stumble into medical journals, particularly through the World Wide Web. Some like what they find enough to keep visiting, and some of the most positive comments I ever received about the BMJ came from non-doctors — usually husbands, wives or children of doctors. They have perhaps a sense of discovering a secret garden, but if the garden is thrown open to the public nobody is much interested. Perhaps the next breakthrough in medical journalism and editing will be to find a way to make health one of the great discourses along with politics, business, the environment and the arts. I think it could be done.
Scientists or researchers are customers of medical journals, but more perhaps as authors than readers. Brian Haynes, a physician from Canada with a great interest in information in healthcare, classifies journals as ‘researcher to researcher’, ‘researcher to clinician’ and ‘clinician to clinician’. A journal like Nature Medicine is a ‘researcher to researcher’ journal. The only practising doctors who read it are those few who are also involved in research in basic science. I’ve hardly met an ordinary doctor who reads Nature Medicine. Many specialist journals are ‘researcher to clinician’ journals and they can be the great unread journals if they are not careful. Journals like Clinical Medicine or the Postgraduate Medical Journal are ‘clinician to clinician’ journals and usually of low status. The major medical journals might best be described as ‘researcher and clinician to researcher and clinician’ journals and the mix can be uneasy. Basic scientists are often scornful of medical journals, judging them to be scientifically weak and containing too much of what they dismiss as ‘soft science’ — science with its roots in the social rather than biological sciences.
Journals live with a constant tension between the needs of authors and readers, and traditionally they were much more concerned with authors. Some journals, often highly profitable ones, have been ‘sausage machines’ for processing authors’ studies. Authors got the credit for having their papers published. Librarians got copies to add to their collections. Publishers got paid well for their journals. Everybody was happy and nobody was much bothered that nobody read the journals. Half the journals in the BMA library are not photocopied once in a year. Half of the articles published in journals are never cited, not even once. The joke is that publishers are like mustard makers — they make their money from material that is never used. I once saw a senior manager from Reed Elsevier, the biggest science publisher, describe the 27 strategic relationships of publishers. The 27th was ‘readers’, which she described as ‘the great unknown’. The company had decided that it wanted to know more about them, but I found it astonishing (until I reflected further) that a publisher could be so large and profitable without having bothered to think about readers.
Nevertheless, authors are essential to journals. Little of what appears in most journals is written by the editors. Most of the material comes from authors who submit their valuable material for free and then traditionally hand over copyright to the journals and publishers. A journal like the BMJ receives 6000 submissions a year and publishes less than 10%. This might make it blasé about authors and the BMJ had a rather brutal triage system that left some authors feeling almost abused. But there is great competition among journals for the best papers and authors. Franz Ingelfinger, the great editor of the New England Journal of Medicine, made the journal preeminent by banging on the doors of all the major researchers in Boston and persuading them to submit their best studies to the journal. The Lancet has had something it calls ‘Project Capture’ to attract to the Lancet studies that might otherwise be published in the New England Journal of Medicine.
So pleasing authors is important but not at the expense of readers. Authors usually want longer papers with more data, more references, more explanation and more reflection on what the study might mean (often nothing in reality, but the moon to the authors). Readers, in contrast, want papers that are shorter and sweeter. One of the important talents of an editor has been to balance the needs of both authors and readers, but the arrival of the electronic world potentially means that both can be fully satisfied. Long versions of studies can be published on the web and shorter versions on paper. The BMJ calls this systems ELPS — ‘electronic long, paper short’ (72). Eventually the short version might be a piece written by journalists rather than the authors.
The owners of journal are clearly important stakeholders, and the relationship between owners and editors is often fraught. In the past five years the editor of one major American journal, JAMA, has been fired, and the editor of another, the New England Journal of Medicine, did not have his contract renewed. A few years before that the editors of the third major American journal, the Annals of Internal Medicine, left the journal after a dispute with the chief executive of the American College of Physicians, the owners of the journal. George Lundberg, the fired editor of JAMA, told me sometime before he was fired that the remarkable thing was that he hadn’t been fired already. Many of the editors of JAMA have been fired and the man who fired George was himself subsequently fired. Not only the editor but also the deputy editor of the Canadian Medical Association Journal were fired early in 2006. Editors in many other countries, including Australia and Ireland, have been fired, but, as far as I can tell, no editor of the BMJ has been fired — although there was a major dispute between the BMA and the journal in the middle of the 20th century, as is described in chapter 12.
Editors are usually fired because of disputes over politics or money. With JAMA it’s often been politics. The American Medical Association (AMA), the owner of JAMA, is a right wing, Republican organization comprised mainly of older doctors who hanker after the days of ‘fee for service’ medicine (when doctors were paid for what they did and ‘managed care’ had not been invented). Only about 30% of American doctors belong to the AMA. Yet the editors of JAMA are trying to produce a journal that will appeal to all doctors and not just to doctors in the United States. It’s inevitable that tensions will arise. The BMJ doesn’t have the same problem because 80% of doctors (and 60% of medical students) belong to the BMA, its owner, making it a broad church.
The problem for the New England Journal of Medicine is more money. The Massachusetts Medical Society has grown very fat on the huge profits of the journal and needs the money badly. It is keen to increase the profits of the journal by exploiting the brand, thus creating tension with the editors, who see themselves as responsible for upholding the quality of the journal and therefore the brand. Bud Reiman, one of the editors of the journal, used to joke that the society would like to create ‘New England Journal fried chicken’ if it could be profitable. Because the society needs the profits of the journal it is also likely to be wary of developments that might make the journal less profitable.
The BMJ began to have this problem. The BMJ Publishing Group has become steadily more profitable, whereas the BMA has seen a growing gap between its income from members’ subscriptions and expenditure on professional activities. Once a journal is viewed by its owner as a ‘money machine’ there is lots of scope for tension.
Advertisers are the final group of stakeholders I want to discuss. Some journals are dependent on advertisers and the advertisers are mainly the pharmaceutical industry. Because the industry has not in most countries been allowed to advertise directly to the public it has concentrated its advertising spend on journals. Most countries have medical newspapers that are sent free to doctors funded by pharmaceutical advertising. With these newspapers advertisers come first and editorial staff second. Editorial material will be cut if advertising is cut, and editors have quickly to produce more material if extra advertising is forthcoming. Most journals have other sources of income, usually subscriptions from institutions, and so are less dependent on advertising. They thus tend to have policies of editorial matters first and advertising matters second. Editors are willing to publish material that they know will offend advertisers, and the journals are not willing to place advertisements beside particular articles at the request of authors.
Many journals are, however, becoming more dependent on advertising and pressure then increases to please advertisers. Increasingly journals are willing to tell advertisers what they are going to publish and then to sell advertising space beside particular articles. Readers might then see a study showing advantages for a drug side by side with advertisements for that drug. The next effectively destroys the independence and value of a journal — is to publish studies that support the advertisers’ products and to decline those that don’t. ‘Freedom of the press in Britain,’ said Hannen Swaffer, ‘is freedom to print such of the proprietor’s prejudices as the advertisers don’t object to.’
Medical journals have many functions and diverse customers. They seem to be good at stirring up debate but poor at affecting change. Traditionally they have been more concerned with authors than readers, but their future — if they have a future — lies in being more concerned with readers.
More From The Trouble With Medical Journals
- Introduction: Medical Journals Are Probably a Force for Good but Need Considerable Reform
- Why Bother With Medical Journals and Whether They Are Honest?
References
- Wakefield AJ, Murch SH, Linnell AAJ et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis and pervasive developmental disorder in children. Lancet 1998;351:637-41.
- Laumann E, Paik A, Rosen R. Sexual dysfunction in the United States: prevalence and predictors. JAMA 1999;281:537-44 (published erratum appears in JAMA 1999;281:1174).
- Moynihan R. The making of a disease: female sexual dysfunction. BMJ 2003;326:45-7.
- Hudson A, Mclellan F. Ethical issues in biomedical publication. Baltimore: Johns Hopkins University Press, 2000.
- Sackett DL, Haynes RB, Guyatt GH, Tugwell P. Clinical epidemiology: a basic science for clinical medicine. London: Little, Brown, 1991.
- Haynes RB. Where’s the meat in clinical journals? ACP Journal Club 1993;119:A23-4.
- Altman DG. The scandal of poor medical research. BMJ 1994;308:283-4.
- Shaughnessy AF, Slawson DC, Bennett JH. Becoming an information master: a guidebook to the medical information jungle. J Fam Pract 1994;39:489-99.
- Bartrip P. Mirror of medicine: a history of the BMJ. Oxford: British Medical Journal and Oxford University Press, 1990.
- Chen RT, DeStefano F. Vaccine adverse events: causal or coincidental? Lancet 1998;351:611-12.
- Pobel D, Vial JF. Case-control study of leukaemia among young people near La Hague nuclear reprocessing plant: the environmental hypothesis revisited. BMJ 1997;314:101.
- Horton R. A statement by the editors of the Lancet. Lancet 2004;363:820-1.
- Murch SH, Anthony A, Casson DH et al. Retraction of an interpretation. Lancet 2004;363:750.
- Smith R. The discomfort of patient power. BMJ 2002;324:497-8.
- Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction and stroke in high risk patients. BMJ 2002;324:71-86.
- Cleland JGF. For debate: Preventing atherosclerotic events with aspirin. BMJ 2002;324:103-5.
- Bagenal FS, Easton OF, Harris E et al. Survival of patients with breast cancer attending Bristol Cancer Help Centre. Lancet 1990;336:606-10.
- Fox R. Quoted in: Smith R. Charity Commission censures British cancer charities. BMJ 1994;308:155-6.
- Richards T. Death from complementary medicine. BMJ 1990;301:510.
- Goodare H. The scandal of poor medical research: sloppy use of literature often to blame. BMJ 1994;308:593.
- Bodmer W. Bristol Cancer Help Centre. Lancet 1990;336:1188.
- Budd JM, Sievert ME, Schultz TR. Phenomena of retraction. Reasons for retraction and citations to the publications. JAMA 1998;280:296-7.
- McVie G. Quoted in: Smith R. Charity Commission censures British cancer charities. BMJ 1994;308:155-6.
- Smith R. Charity Commission censures British cancer charities. BMJ 1994;308:155-6.
- Feachem RGA, Sekhri NK, White KL. Getting more for their dollar: a comparison of the NHS with California’s Kaiser Permanente. BMJ 2002;324:135-41.
- Himmelstein DU, Woolhandler S, David OS et al. Getting more for their dollar: Kaiser v the NHS. BMJ 2002;324:1332.
- Talbot-Smith A, Gnani S, Pollock A, Pereira Gray D. Questioning the daims from Kaiser. Br J Gen Pract 2004;54:415-21.
- Ham C, York N, Sutch S, Shaw A. Hospital bed utilisation in the NHS, Kaiser Permanente, and the US Medicare programme: analysis of routine data. BMJ 2003;327:1257-61.
- Sanders SA, Reinisch JM. Would you say you ‘had sex’ If…? JAMA 1999;281:275-7.
- Anonymous. lfs over, Debbie. JAMA 1988;259:272.
- Lundberg G. ‘lfs over, Debbie,’ and the euthanasia debate. JAMA 1988;259:2142-3.
- Smith A. Euthanasia: time for a royal commission. BMJ 1992;305:728-9.
- Doyal L, Doyal L. Why active euthanasia and physician assisted suicide should be legalised. BMJ 2001;323:1079-80.
- Emanuel EJ. Euthanasia: where The Netherlands leads will the world follow? BMJ 2001;322:1376-7.
- Angell M. The Supreme Court and physician-assisted suicide-the ultimate right N Eng J Med 1997;336:50-3.
- Marshall VM. lfs almost over — more letters on Debbie. JAMA 1988;260:787.
- Smith A. Cheating at medical school. BMJ 2000;321:398.
- Davies S. Cheating at medical school. Summary of rapid responses. BMJ 2001;322:299.
- Ewen SWB, Pusztai A. Effects of diets containing genetically modified potatoes expressing Galanthus nivalis lactin on rat small intestine. Lancet 1999;354:1353-4.
- Horton A. Genetically modified foods: ‘absurd’ concern or welcome dialogue? Lancet 1999;354:1314-15.
- Kuiper HA, Noteborn HPJM, Peijnenburg AACM. Adequacy of methods for testing the safety of genetically modified foods. Lancet 1999;354:1315.
- Bombardier C, Laine L, Reicin A et al. Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. N Eng J Med 2000;343:1520-8.
- Curfman GO, Morrissay S, Drazen JM. Expression of concern: Bombardier et al., ‘Comparison of Upper Gastrointestinal Toxicity of Rofecoxib and Naproxen in Patients with Rheumatoid Arthritis.’ N Eng J Med 2000;343:1520-8. N Eng J Med 2005;353:2813-4.
- Curfman GO, Morrissey S, Drazen JM. Expression of concern reaffirmed. N Eng J Med 2006;354: 1193.
- Laumann E, Paik A, Rosen A. Sexual dysfunction in the United States: prevalence and predictors. JAMA 1999;281:537-44 (published erratum appears in JAMA 1999;281:1174).
- Smith A. In search of ‘non-disease.’ BMJ 2002;324:883-5.
- Hughes C. BMJ admits ‘lapses’ after article wiped £30m off Scotia shares. Independent 10 June 2000.
- Hettiaratchy S, Clarke J, Taubel J, Besa C. Bums after photodynamic therapy. BMJ 2000;320:1245.
- Bryce A. Bums after photodynamic therapy. Drug point gives misleading impression of incidence of bums with temoporfin (Foscan). BMJ 2000;320:1731.
- Richmond C. David Horrobin. BMJ 2003;326:885.
- Enstrom JE, Kabat GC. Environmental tobacco smoke and tobacco related mortality in a prospective study of Californians, 1960-98. BMJ 2003;326:1057-60.
- Roberts J, Smith A. Publishing research supported by the tobacco industry. BMJ 1996;312:133-4.
- Lefanu WR. British periodicals of medicine 1640-1899. London: Wellcome Unit for the History of Medicine, 1984.
- Squire Sprigge S. The life and times of Thomas Wakley. London: Longmans, 1897.
- Bartrip PWJ. Themselves writ large: the BMA 183~1966. London: BMJ Books, 1996.
- Delamothe T. How political should a general medical journal be? BMJ 2002;325:1431-2.
- Gedalia A. Political motivation of a medical joumal [electronic response to Halileh and Hartling. Israeli-Palestinian conflict]. BMJ 2002. http:/lbmj.com/cgi/eletters/324173331361#20289 (accessed 10 Dec 2002).
- Marchetti P. How political should a general medical journal be? Medical journal is no place for politics. BMJ 2003;326:1431-32.
- Roberts I. The second gasoline war and how we can prevent the third. BMJ 2003;326:171.
- Roberts IG. How political should a general medical journal be? Medical journals may have had role in justifying war. BMJ 2003;326:820.
- Institute of Medicine. Crossing the quality chasm. Anew health system for the 21st century. Washington: National Academy Press, 2001.
- Oxman AD, Thomson MA, Davis DA, Haynes RB. No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. Can Med Assoc J 1995;153:1423-31.
- Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet 1993;342:1317-22.
- Grol R. Beliefs and evidence in changing clinical practice. BMJ 1997;315:418-21.
- Smith R. What clinical information do doctors need? BMJ 1996;313:1062-8.
- Godlee F, Smith A, Goldman D. Clinical evidence. BMJ 1999;318:1570-1.
- Smith R. The BMJ: moving on. BMJ 2002;324:5-6.
- Milton J. Aeropagitica. World Wide Web: Amazon Press (digital download), 2003.
- Coulter A. The autonomous patient ending paternalism in medical care. London: Stationery Office Books, 2002.
- Muir Gray JA. The resourceful patient. Oxford: Rosetta Press, 2001.
- World Health Organization. Macroeconomics and health: investing in health for economic development. Report of the commission on macroeconomics and health. Geneva: WHO, 2001.
- Mullner M, Groves T. Making research papers in the BMJ more accessible. BMJ 2002;325:456.
Comments on What and Who Are Medical Journals For?
It’s a bizarre thing to even consider that a product be focused on its creator more than its eventual recipient, especially when said product is some form of writing and its recipient is the reader. This conjures up multiple layers of questions, regardless of whether or not the reader is the medical professional or the patient. If we want a customer/patient first world, it would seem prudent to move in a direction of reader focused journals, as to create an environment where the one thing that really matters (the treatment or advice), is done so in an environment where doctor and patient are both well informed.
After all, in reflection, it seems to me that anything I’ve ever read (of benefit or enjoyment), was indeed written for me, the reader.
What and Who Are Medical Journals For?
1