“Science … warns me to be careful how I adopt a view which jumps with my preconceptions, and to require stronger evidence for such belief than for one to which I was previously hostile. My business is to teach my aspirations to conform themselves to fact, not to try and make facts harmonize with my aspirations.”
—Thomas Huxley, 1860
In an era when dietary advice is dispensed freely by virtually everyone from public health officials to personal trainers, well-meaning relatives, and strangers on check-out lines, one recommendation has rung through 3 decades with the indisputable force of gospel: Eat less salt and you will lower your blood pressure and live a longer, healthier life. This has been the message promoted by both the National Heart, Lung, and Blood Institute (NHLBI) and the National High Blood Pressure Education Program (NHBPEP), a coalition of 36 medical organizations and six federal agencies. Everyone, not just the tens of millions of Americans who suffer from hypertension, could reduce their risk of heart disease and stroke by eating less salt. The official guidelines recommend a daily allowance of 6 grams (2400 milligrams of sodium), which is 4 grams less than our current average. This “modest reduction,” says NHBPEP director Ed Roccella, “can shift some arterial pressures down and prevent some strokes.” Roccella’s message is clear: “All I’m trying to do is save some lives.”
So what’s the problem? For starters, salt is a primary determinant of taste in food — fat, of course, is the other — and 80% of the salt we consume comes from processed foods, making it difficult to avoid. Then there’s the kicker: While the government has been denouncing salt as a health hazard for decades, no amount of scientific effort has been able to dispense with the suspicions that it is not. Indeed, the controversy over the benefits, if any, of salt reduction now constitutes one of the longest running, most vitriolic, and surreal disputes in all of medicine.
On the one side are those experts — primarily physicians turned epidemiologists, and administrators such as Roccella and Claude Lenfant, head of NHLBI — who insist that the evidence that salt raises blood pressure is effectively irrefutable. They have an obligation, they say, to push for universal salt reduction, because people are dying and will continue to die if they wait for further research to bring scientific certainty. On the other side are those researchers — primarily physicians turned epidemiologists, including former presidents of the American Heart Association, the American Society of Hypertension, and the European and international societies of hypertension — who argue that the data supporting universal salt reduction have never been compelling, nor has it ever been demonstrated that such a program would not have unforeseen negative side effects. This was the verdict, for instance, of a review published last May in the Journal of the American Medical Association (JAMA). University of Copenhagen researchers analyzed 114 randomized trials of sodium reduction, concluding that the benefit for hypertensives was significantly smaller than could be achieved by antihypertensive drugs, and that a “measurable” benefit in individuals with normal blood pressure (normotensives) of even a single millimeter of mercury could only be achieved with an “extreme” reduction in salt intake. “You can say without any shadow of a doubt,” says Drummond Rennie, a JAMA editor and a physiologist at the University of California (UC), San Francisco, “that the [NHLBI] has made a commitment to salt education that goes way beyond the scientific facts.”
At its core, the salt controversy is a philosophical clash between the requirements of public health policy and the requirements of good science, between the need to act and the institutionalized skepticism required to develop a body of reliable knowledge. This is the conflict that fuels many of today’s public health controversies: “We’re all being pushed by people who say, ‘Give me the simple answer. Is it or isn’t it?’ ” says Bill Harlan, director of the office of disease prevention at the National Institutes of Health (NIH). “They don’t want the answer after we finish a study in 5 years. They want it now. No equivocation. … [And so] we constantly get pushed into positions we may not want to be in and cannot justify scientifically.”
The dispute over salt, however, is an idiosyncratic one, remarkable in several fundamental aspects. Foremost, many who advocate salt reduction insist publicly that the controversy is a) either nonexistent, or b) due solely to the influence of the salt lobby and its paid consultant-scientists. Jeremiah Stamler, for instance, a cardiologist at Northwestern University Medical School in Chicago who has led the charge against salt for 2 decades, insists that the controversy has “no genuine scientific basis in reproducible fact.” He attributes the appearance of controversy to the orchestrated resistance of the food processing industry, which he likens to the tobacco industry in the fight over cigarettes, always eager to obfuscate the facts. “My considerable experience indicates that there is no scientific interest on the part of any of these people to tell the truth,” he says.
While Stamler’s position may seem extreme, it is shared by administrators at the NHBPEP and the NHLBI, which funds all relevant research in this country. Jeff Cutler, director of the division of clinical applications and interventions at NIH and an advocate of salt restriction for over a decade, told Science that even to publish an article such as this one acknowledging the existence of the controversy is to play into the hands of the salt lobby. “As long as there are things in the media that say the salt controversy continues,” Cutler says, “they win.” Roccella concurs: To publicize the controversy, he told Science, serves only to undermine the public health of the nation.
After interviews with some 80 researchers, clinicians, and administrators throughout the world, however, it is safe to say that if ever there were a controversy over the interpretation of scientific data, this is it. In fact, the salt controversy may be what Sanford Miller calls the “number one perfect example of why science is a destabilizing force in public policy.” Now a dean at the University of Texas Health Sciences Center, Miller helped shape salt policy 20 years ago as director of the Center for Food Safety and Applied Nutrition at the Food and Drug Administration. Then, he says, the data were bad, but they arguably supported the benefits of salt reduction. Now, both the data and the science are much improved, but they no longer provide forceful support for the recommendations.
The salt controversy is the “number one perfect example of why science is a destabilizing force in public policy.”
—Sanford Miller
That raises the second noteworthy aspect of the controversy: After decades of intensive research, the apparent benefits of avoiding salt have only diminished. This suggests either that the true benefit has now been revealed and is indeed small, or that it is nonexistent, and researchers believing they have detected such benefits have been deluded by the confounding influences of other variables. (These might include genetic variability; socioeconomic status; obesity; level of physical exercise; intake of alcohol, fruits and vegetables, or dairy products; or any number of other factors.)
The controversy itself remains potent because even a small benefit — one clinically meaningless to any single patient — might have a major public health impact. This is a principal tenet of public health: Small effects can have important consequences over entire populations. If by eating less salt, the world’s population reduced its average blood pressure by a single millimeter of mercury, says Oxford University epidemiologist Richard Peto, that would prevent several hundred thousand deaths a year: “It would do more for worldwide deaths than the abolition of breast cancer.” But even that presupposes the 1-millimeter drop can be achieved by avoiding salt. “We have to be sure that 1- or 2-millimeter effect is real,” says John Swales, former director of research and development for Britain’s National Health Service and a clinician at the Leicester Royal Infirmary. “And we have to be sure we won’t have equal and opposite harmful effects.”
Decades have passed without a resolution because the epidemiologic tools are incapable of distinguishing a small benefit from no benefit or even from a small adverse effect. This has led to a literature so enormous and conflicting that it is easy to amass a body of evidence — what Stamler calls a “totality of data” — that appears to support a particular conviction definitively, unless one is aware of the other totality of data that doesn’t.
Over the years, advocates of salt reduction have often wielded variations on the “totality of data” defense to reject any finding that doesn’t fit the orthodox wisdom. In 1984, for instance, David McCarron and colleagues from the Oregon Health Sciences University in Portland published in Science an analysis of a national health and nutrition database suggesting that salt was harmless. They were taken to task in these pages by Sanford Miller, Claude Lenfant, director of NHLBI, and Manning Feinleib, then head of the National Center for Health Statistics. Among their criticisms was that McCarron and colleagues had not “attempt[ed] to square their conclusions with the abundance of population-based and experimental data suggesting that dietary sodium indeed plays an important role in hypertension.” At the time of the letter, however, Lenfant’s NHLBI was about to fund perhaps the largest international study ever done, known as Intersalt, precisely to determine whether salt did play such a role. And even Stamler, the motivating force behind Intersalt, was describing the literature on salt and blood pressure at the time as “replete with inconsistent and contradictory reports.”
One-sided interpretations of the data have always been endemic to the controversy. As early as 1979, for instance, Olaf Simpson, a clinician at New Zealand’s University of Otago Medical School, described it as “a situation where the most slender piece of evidence in favor of [a salt-blood pressure link] is welcomed as further proof of the link, while failure to find such evidence is explained away by one means or another.” University of Glasgow clinician Graham Watt calls it the “Bing Crosby approach to epidemiological reasoning” — in other words, “accentuate the positive, eliminate the negative.” Bing Crosby epidemiology allows researchers to find the effect they’re looking for in a swamp of contradictory data but does little to establish whether it is real.
This situation is exacerbated by a remarkable inability of researchers in this polarized field to agree on whether any particular study is believable. Instead, it is common for studies to be considered reliable because they get the desired result. In 1991, for instance, the British Medical Journal (BMJ) published a 14-page, three-part “meta-analysis” by epidemiologists Malcolm Law, Christopher Frost, and Nicholas Wald of the Medical College of St. Bartholomew’s Hospital in London. Their conclusion: The salt-blood pressure association was “substantially larger” than previously appreciated. That same year, Swales deconstructed the analysis, which he describes as “deeply flawed,” at the annual meeting of the European Society of Hypertension in Milan. “There was not a single person in the room who felt the [BMJ] analysis was worth anything after that,” says clinician Lennart Hansson of the University of Uppsala in Sweden, who attended the meeting and is a former president of both the international and European societies of hypertension. Swales’s critique was then published in the Journal of Hypertension.
Just 2 years later, however, the NHBPEP released a landmark report on the primary prevention of hypertension, in which the government first recommended universal salt reduction. The BMJ meta-analysis was cited repeatedly as “compelling evidence of the value of reducing sodium intake.” This spring, however, it was still possible to get opinions about the BMJ review from equally respected researchers ranging from “reads like a New Yorker comedy piece” and the “worst example of a meta-analysis in print by a long shot” to “competently done and competently analyzed and interpreted” and a seminal paper in the field.
Crystallizing a debate
The case against salt begins with physiological plausibility. Eat more salt, and your body will maintain its sodium concentration by retaining more water. “If you go on a salt binge,” says Harvard Medical School nephrologist Frank Epstein, “you will retain salt and with it a proportionate amount of water until your kidneys respond and excrete more salt. In most people, you will detect a slight increase in blood pressure when body fluids are swollen like this, although there is a very broad spectrum of responses.”
Behind this spectrum is a homeostatic mechanism that has been compared to a Russian novel in its complexity. The cast of characters includes some 50 different nutrients, growth factors, and hormones. Sodium, for instance, is important for maintaining blood volume; potassium for vasodilation or constriction; and calcium for vascular smooth muscle tone. Increase your caloric intake, and your sympathetic nervous system responds to constrict your blood vessels, thus raising your blood pressure. Decrease your calories, and your blood pressure falls. To make matters still more complicated, the interplay of these variables differs with age, sex, and even race. Most researchers believe that a condition known as salt sensitivity explains why the blood pressure of some individuals rises with increased salt but not others, but even that is controversial, says Harlan. No diagnostic test exists for salt sensitivity other than giving someone salt and seeing what happens, which still won’t predict whether the sensitivity is lifelong or transitory. Despite this complexity, most researchers still believe it makes physiological sense that populations with high-salt diets would have more individuals with high blood pressure than those with low salt diets, and that lowering salt intake would lower blood pressure.
“You can say without any shadow of a doubt that the [NHLBI] has made a commitment to salt education that goes way beyond the scientific facts.”
—Drummond Rennie
By the 1970s, when the government began recommending salt reduction to treat hypertension — defined as systolic blood pressure higher than 140 mmHg and diastolic higher than 90 mmHg (140/90 mmHg) — the physiological plausibility had been supplemented by a grab bag of not particularly definitive studies and clinical lore. In the 1940s, for instance, Duke University clinician Wallace Kempner demonstrated that he could successfully treat hypertensive patients with a low-salt, rice-and-peaches diet. For years Kempner’s regimen was the only nonsurgical treatment for severe hypertension, a fact that may have done more than anything to convince an entire generation of clinicians of the value of salt reduction. In a seminal 1972 paper, Lewis Dahl, a physician at Brookhaven National Laboratory in Upton, New York, and the primary champion of salt reduction in this country until his death in 1975, claimed it was proven that a low-salt diet reduced blood pressure in hypertensives. When it didn’t, he said, that only proved that the patient had fallen off the diet, “all protestation to the contrary, notwithstanding.” Whether it was low salt that explained the diet’s effect is still debatable, however. Kempner’s regimen was also extraordinarily low in calories and fat and high in potassium, factors that themselves are now known to lower blood pressure.
Dahl furthered the case for a salt-blood pressure link by breeding a strain of salt-sensitive hypertensive rats. Researchers still cite this work as compelling evidence for the role of salt in human hypertension. As Simpson pointed out in 1979, however, Dahl’s rats became hypertensive only if fed an amount of salt equivalent to more than 500 grams a day for an adult human — “probably outside the area of relevance,” Simpson noted. Lately, researchers have been touting a 1995 study of chimps fed a high-salt diet. But Harlan notes that “it’s unlikely” that any existing animal models of hypertension are particularly relevant to humans.
Throughout the early years of the controversy, the most compelling evidence against salt came from a type of epidemiologic study known as an “ecologic” study, in which researchers compared the salt intake of indigenous populations — the Yanomamo Indians of Brazil, for instance — that had little or no hypertension and cardiovascular disease to that of industrialized societies. Inevitably the indigenous populations ate little or no salt; the industrialized societies ate a lot. While the Yanomamo ate less than a gram of salt daily, for instance, the northern Japanese ate 20 to 30 grams — the highest salt intake in the world — and had the highest stroke rates. Such findings were reinforced by migration studies, in which researchers tracked down members of low-salt communities who had moved to industrialized areas only to see both their salt intake and blood pressure rise.
The findings led researchers to postulate an intuitive Darwinian argument for salt reduction: Humans evolved in an environment where salt was scarce, and so those who survived were those best adapted to retaining salt. This trait, so the argument goes, would have been preserved even though we now live in an environment of salt abundance. By this logic, the appropriate intake of salt is that of the primitive societies — a few grams a day — and all industrialized societies eat far too much and pay it for it in heart disease and stroke.
The catch to this accumulation of data and hypotheses was that it only included half the data. The other half was the half that didn’t fit — in particular, data from the epidemiologic studies known as intrapopulation studies. These compared salt intake and blood pressure in individuals within a population — males in Chicago, for instance — and invariably found no evidence that those who ate a lot of salt had higher blood pressure than those who ate little. Among the intrapopulation studies that came up negative were an analysis of 20,000 Americans conducted by the National Center for Health Statistics around 1980.
“All I’m trying to do is save some lives.”
—Ed Roccella
Neither kind of study was capable of giving a definitive answer, however. The ecologic studies were certainly the least sound scientifically, and epidemiologists today put little stock in them. The potentially fatal flaw in ecologic studies is always the number of variables other than the one at issue that might differ between the populations and explain the relevant effect. Populations that eat little salt, for instance, also consume fewer calories; eat more fruits, vegetables, and dairy products; are leaner and more physically active; drink less alcohol; and are less industrialized. Any one of these differences or some combination of them might be responsible for the lower blood pressure. Indigenous people also tend to die young from infectious diseases or trauma, notes Epstein, while industrialized societies live long enough to die of heart disease.
Both ecologic and intrapopulation studies also suffer from the remarkable difficulty of accurately assessing average blood pressure — which can vary greatly from day to day — or a lifetime intake of salt. Most of the early ecologic studies based their assessments of salt intake on guesses rather than measurements. In 1973, when University of Michigan anthropologist Lillian Gleibermann published what’s still considered a seminal paper linking salt and blood pressure, she based her conclusions on 27 ecologic studies, only 11 of which actually tried to measure sodium intake. A 24-hour collection of urine is considered to be the best assessment of salt intake, because we quickly excrete in our urine all the salt we consume. But even that will only reflect the salt intake of those 24 hours, not necessarily of an entire month, year, or lifetime. “You need at least five to 10 measures of sodium in urine collected on different days to get a measure of habitual intake,” says Daan Kromhout, a nutritional epidemiologist at the National Institute of Public Health and the Environment in the Netherlands. “You can’t do that in an epidemiologic field situation.”
To researchers who accept the salt-blood pressure hypothesis, these measurement problems served to explain why intrapopulation studies wouldn’t see an association even if one existed. Quite simply, the link between salt and blood pressure, however potent, would likely be washed out by the measurement errors. Moreover, any experiment large enough to have the statistical power to overcome these errors would be prohibitively expensive.
In the early 1980s, London School of Tropical Medicine and Hygiene epidemiologist Geoffrey Rose suggested another reason why the intrapopulation studies might fail to detect benefits of salt reduction that could still have a significant public health impact. Rose speculated that if the entire developed world consumed too much salt, as ecologic studies suggested, then epidemiology would never be able to link salt to hypertension, regardless of how causal the relationship. Imagine, he wrote, if everyone smoked a pack of cigarettes daily; then any intrapopulation study “would lead us to conclude that lung cancer was a genetic disease … since if everyone is exposed to the necessary agent, then the distribution of cases is wholly determined by individual susceptibility.” Thus, as with salt and high blood pressure, the clues would have to be “sought from differences between populations or from changes within populations over time.” By the same logic, cutting salt consumption a small amount might have little effect on a single individual — just as going from 20 cigarettes to 19 would — but a major impact on mortality across an entire population.
Although Rose’s proposition made intuitive sense, it still rested on the unproven conjecture that avoiding salt could reduce blood pressure, a conjecture that was beginning to seem extraordinarily resistant to any findings that might negate it. In 1979, for instance, Stamler and his Northwestern colleagues tested the hypothesis in an intrapopulation study of Chicago schoolchildren. They compared blood pressure in 72 children to salt intake, estimated from seven consecutive 24-hour urine samples, enough to reliably reflect habitual sodium intake. They reported a “clear-cut” relationship between sodium and blood pressure in the children but then tried twice to reproduce the result and failed twice.
Opinions on one study range from “reads like a New Yorker comedy piece” and the “worst example of a meta-analysis in print by a long shot” to “competently done and competently analyzed and interpreted.”
“A variety of potential explanations of this phenomenon could be advanced,” the authors wrote, one of which was the obvious: “No relationship in fact exists between sodium and [blood pressure]. …” They then listed five reasons why they might have missed the expected relationship — insensitive measurement techniques, for instance, or genetic variability obscuring the role of sodium, or the possibility that “the true relationship is not yet evident in children.” Because the first of the three studies was positive, Stamler and his colleagues concluded that their data were “not wholly negative” and “do in fact suggest a weak and inconsistent relationship.”
This logic served to manifest what Simpson called “the resilience and virtual indestructibility of the salt-hypertension hypothesis. Negative data can always be explained away.”
“Another thing I must point out is that you cannot prove a vague theory wrong. … Also, if the process of computing the consequences is indefinite, then with a little skill any experimental results can be made to look like the expected consequences.”
—Richard Feynman, 1964
Through the early 1980s, the scientific discord over salt reduction was buried beneath the public attention given to the benefits of avoiding salt. The NHBPEP had decreed since its inception in 1972 that salt was an unnecessary evil, a conclusion reached as well by a host of medical organizations, not to mention the National Academy of Sciences and the Surgeon General. By 1978, the Center for Science in the Public Interest, a consumer advocacy group, was describing salt as “the deadly white powder you already snort” and lobbying Congress to require food labeling on high-salt foods. In 1981, the FDA launched a series of “sodium initiatives” aimed at reducing the nation’s salt intake.
Not until after these campaigns were well under way, however, did researchers set out to do studies that might be powerful enough to resolve the underlying controversy. The first was the Scottish Heart Health Study, launched in 1984 by epidemiologist Hugh Tunstall-Pedoe and colleagues at the Ninewells Hospital and Medical School in Dundee, Scotland. The researchers used questionnaires, physical exams, and 24-hour urine samples to establish the risk factors for cardiovascular disease in 7300 Scottish men. This was an order of magnitude larger than any intrapopulation study ever done with 24-hour urine samples. The BMJ published the results in 1988: Potassium, which is in fruits and vegetables, seemed to have a beneficial effect on blood pressure. Sodium had no effect.
With this result, the Scottish study vanished from the debate. Advocates of salt reduction argued that the negative result was no surprise because the study, despite its size, was still not large enough to overcome the measurement problems that beset all other intrapopulation studies. When the NHBPEP recommended universal salt reduction in its landmark 1993 report, it cited 327 different journal articles in support of its recommendations. The Scottish study was not among them. (In 1998, Tunstall-Pedoe and his collaborators published a 10-year follow-up: Sodium intake now showed no relationship to either coronary heart disease or death.)
The second collaboration was Intersalt, led by Stamler and Rose. Unlike the relentlessly negative Scottish Heart Health Study, Intersalt would become the most influential and controversial study in the salt debate. Intersalt was designed specifically to resolve the contradiction between ecologic and intrapopulation studies. It would compare blood pressure and salt consumption, as measured by 24-hour urine samples, from 52 communities around the globe, from the highest to the lowest extremes of salt intake. Two hundred individuals — half males, half females, 50 from each decade of life between 20 and 60 — were chosen at random from each population. In effect, Intersalt would be 52 small but identical intrapopulation studies combined into a single huge ecologic study.
After years of work by nearly 150 researchers, the results appeared in the same 1988 BMJ issue that included the Scottish Heart Health Study. Intersalt had failed to confirm its primary hypothesis, which was the existence of a linear relationship between salt intake and blood pressure. Of the 52 populations, four were primitive societies like the Yanomamo with low blood pressure and daily salt intake below 3.5 grams. They also differed, however, in virtually every other imaginable way from the 48 industrialized societies that had higher blood pressure. The remaining 48 revealed no relationship between sodium intake and blood pressure. The population with the highest salt intake, for instance — in Tianjin, China, consuming roughly 14 grams a day — had a median blood pressure of 119/70 mmHg, while the one with the lowest salt intake — a Chicago African-American population at 6 grams a day — had a median blood pressure of 119/76 mmHg. Only body mass and alcohol intake correlated with blood pressure in this comparison.
The Intersalt researchers did derive two positive correlations between salt and blood pressure. One weak association appeared when they treated the 10,000-plus subjects as a single large population rather than 52 distinct populations. It implied that cutting salt intake from 10 grams a day to four would reduce blood pressure by 2.2/0.1 mmHg. The more potent association was between salt intake and the rise in blood pressure with age: Populations that ate less salt experienced a smaller rise than did populations that ate more salt. If this relationship was causal, Intersalt estimated, then cutting salt intake by 6 grams a day would reduce the average rise in blood pressure between the ages of 25 and 55 by 9/4.5 mmHg.
These findings made Intersalt Rorschach-like in its ability to generate conflicting interpretations. John Swales wrote off the results in an accompanying BMJ editorial, saying the potential benefit, if any, was so small it “would hardly seem likely to take nutritionists to the barricades (except perhaps the ones already there).” Today, the majority of the researchers interviewed by Science, including Intersalt members such as Daan Kromhout and Lennart Hansson, see it as a negative study. Says Hansson, “It did not show blood pressure increases if you eat a lot of salt.”
Stamler and other Intersalt leaders vehemently disagree. When the results were published, Stamler described them as “abundant, rich, and precise confirmation” of the sodium-blood pressure association and used them to advocate a 6-gram “reduction in salt intake for everyone.” In this view, the definitive positive finding was the correlation between salt consumption and rising blood pressure with age. Intersalt’s Hugo Kesteloot, for instance, an epidemiologist at the Catholic University of Leuven in Belgium, says this was “the most interesting finding” and “confirmatory.” Officials at the NHBPEP and NHLBI sided with this interpretation. In 1993, the NHBPEP report on primary prevention of hypertension cited Intersalt for confirming the “strong positive relationship” between sodium intake and blood pressure reported by Dahl in 1972, which was precisely what it did not do. NHLBI’s Cutler still describes the results as “overwhelmingly positive.”
“The most slender piece of evidence in favor of [a salt-blood pressure link] is welcomed as further proof of the link, while failure to find such evidence is explained away.”
—Olaf Simpson
Critics, however, noted that the association Stamler and his colleagues found so telling — between salt intake and blood pressure rise with age — was not included among the hypotheses that Intersalt had clearly delineated in prestudy publications describing its methodology. This made the finding appear to be a post hoc analysis, a practice known pejoratively as “data dredging.” In such situations, the researchers are no longer testing hypotheses, as the scientific method requires, but are finding hypotheses that fit data already accumulated. Although this doesn’t mean the new hypotheses are not true, it does mean they have not been properly tested.
Because Intersalt wasn’t designed to test a link between salt and a rise in blood pressure with age, explains NIH’s Bill Harlan, the association reported later could be treated as no more than an inference: “If you [were going] in with that as a specific hypothesis, you would have set the study up differently,” for example, by including a wider range of ages and a larger sample of each population. David Freedman, a UC Berkeley statistician, puts it more bluntly, saying that the conclusion about salt and rising blood pressure with age looked like “something they dragged in when the primary analyses didn’t go their way.”
Although Intersalt members agree that testing a hypothesized link between salt and rising blood pressure with age was not in their proposals, they insist it was always part of the plan. “It just wasn’t in by omission. Stupidly,” says Intersalt’s Paul Elliot, an epidemiologist at London’s Imperial College School of Medicine. Alan Dyer of Northwestern University, the collaboration’s biostatistician, says, “It just was one of those things that didn’t get written down.” Stamler insists it was recorded in the minutes of a meeting and in an early publication, and that the accusations of “retrospective data-dredging” are “factually wrong” and should be retracted.
Far from delivering the last word on salt, Intersalt had dissolved in ambiguous data and contradictory interpretations. And that was just round one.
Intersalt tries again
In 1993, after the NHBPEP cited Intersalt as supporting a recommendation of universal sodium reduction, the Salt Institute, a Washington-based trade organization of salt producers, began a concerted effort to obtain Intersalt’s raw data. The institute’s director, Richard Hanneman, says he wanted to examine the reported association between salt intake and rise in blood pressure with age. He and some of the researchers who consult for the institute for $3000 a year — McCarron; University of Alabama, Birmingham, cardiologist Suzanne Oparil; University of Toronto epidemiologist Alexander Logan; and UC Davis nutritionist Judy Stern — were puzzled by what they saw as a contradiction in the data. If higher salt intake resulted in a greater increase in blood pressure as the population aged, they reasoned, the centers with high salt intakes should have had higher median blood pressures, which wasn’t the case. Only if the Intersalt centers with high salt intake had lower blood pressure to start with could their median blood pressures have come out roughly equal, as Intersalt reported. While this seemed counterintuitive, Intersalt had not published the data — the blood pressure of the 20- to 29-year-olds — that would allow the hypothesis to be checked independently.
Hanneman failed to get Intersalt’s raw data, but he did obtain enough secondary data to publish a paper in May 1996, in an issue of the BMJ dedicated to Intersalt. Hanneman claimed to confirm that Intersalt centers with higher salt intake did indeed have lower systolic blood pressures in their youngest cohorts. Accompanying editorials, all written by outspoken advocates of salt reduction, harshly rejected the analysis. Malcolm Law, for instance, dismissed Hanneman’s ideas as a “bizarre hypothesis” and an example of “the lengths to which a commercial group will go to protect its market when presented with clear evidence detrimental to its interests.” But none of these commentators addressed the apparent contradiction in Intersalt’s claims. Other researchers who read the paper — Intersalt collaborator Friedrich Luft, for instance, a nephrologist at Berlin’s Humboldt University, and Freedman, who read it at Science’s request — noted flaws in Hanneman’s reanalysis but also agreed that the Intersalt findings seemed inexplicable.
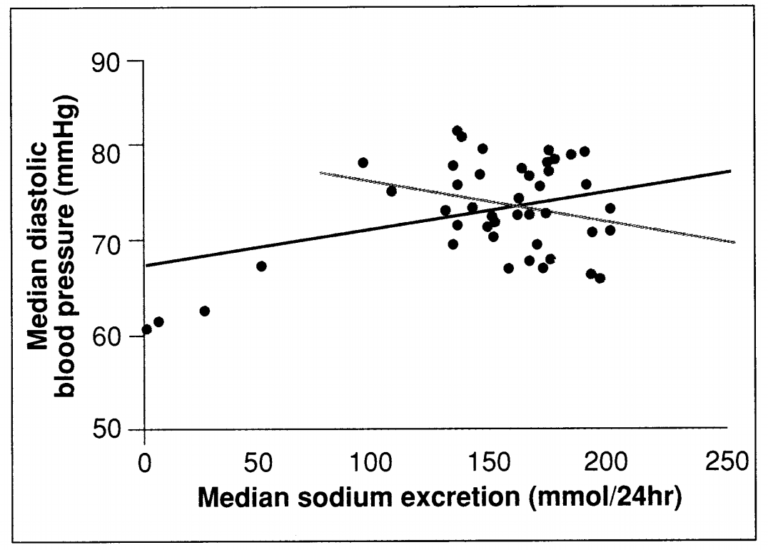
Figure 1: Dueling trends. The relation of salt and blood pressure for all 52 Intersalt populations (red) and for the 48 industrialized populations without very low salt consumption (brown). (Source: Intersalt, 1988)
This particular dispute turned out to be moot, however, given the controversy ignited by another paper in the same issue: Intersalt’s own reanalysis of its data. Under the title Intersalt Revisited, Stamler and his colleagues addressed what they considered a problem in their original publication: that they may have underestimated the true association between salt and blood pressure.
Their reanalysis stepped into one of the most controversial areas in epidemiology, known as regression dilution bias. The gist is that if an association between two variables — such as salt and blood pressure — is real, any errors in measuring exposure to either variable will only serve to “dilute” the apparent cause and effect. In this case, because both 24-hour urine samples and single blood pressure readings are likely to stray from the long-term averages, Intersalt’s analysis would have underestimated the true strength of the effect of salt on blood pressure. “If [the association] is real,” says Elliot, “it is biased toward the null, and so you have to accept the reality that it must be larger than measured.” Statistical techniques could then be used to correct it upward to its proper size. The catch, of course, is that such corrections would inflate a spurious association as well.
Stamler and colleagues, certain of the reality of the salt-blood pressure link, now corrected their 1988 estimates for regression dilution bias. With a few other corrections, the net effect was to enhance the apparent benefits of salt reduction from something ambiguous in 1988 to consistent, “strong, positive” associations in 1996. Cutting daily salt intake by 6 grams, they now concluded, would drop blood pressure by 4.3/1.8 mmHg, a benefit three times larger than originally estimated. “Now the position has been clarified,” wrote Law. “All the Intersalt analyses confirm salt as an important determinant of blood pressure.”
But the position had not been clarified. The BMJ editors had initially commissioned a commentary to run with Intersalt’s reanalysis from epidemiologists George Davey Smith of the University of Bristol in the United Kingdom and Andrew Phillips of the Royal Free Hospital School of Medicine in London. The critique they submitted was so damning of Intersalt Revisited, however, that the BMJ editors felt compelled to reveal it to the Intersalt authors before publication. According to BMJ editor Richard Smith, Stamler and his colleagues objected so strongly to the commentary that the BMJ agreed to run it 6 weeks later, disassociated, at least in time, from the work it called into question.
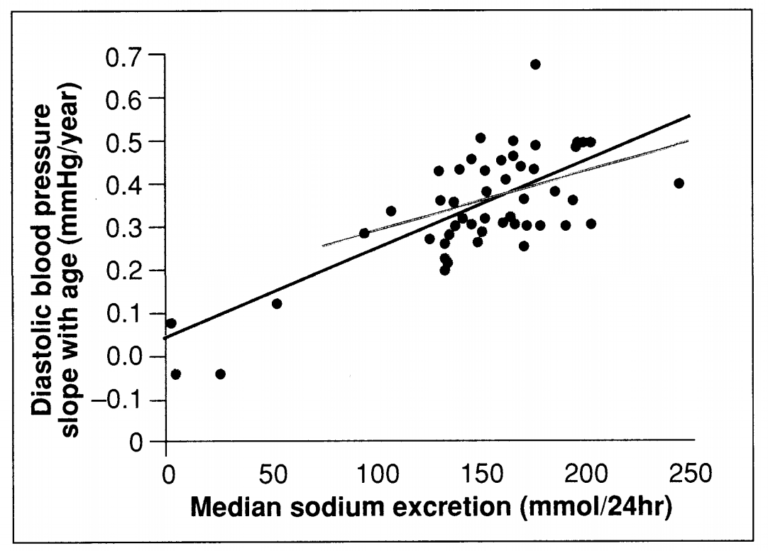
Figure 2: Positive finding? Intersalt data show a correlation between salt consumption and the rise in blood pressure with age.
As Davey Smith explained to Science, their commentary identified a litany of problems with Intersalt Revisited, from “O-level mathematical mistakes” to basing their statistical corrections on assumptions unsupported by data. For instance, in order to correct for regression dilution bias, Stamler and his colleagues assumed that changes in sodium intake and blood pressure in any individual were independent of each other over periods of a few weeks. But if blood pressure and salt intake did fluctuate together, Davey Smith and Phillips noted, then the Intersalt corrections would result in “an inappropriately inflated estimate.” The two epidemiologists cited studies concluding that blood pressure and salt intake are related in the short term and pointed out that “the very hypothesis under test — that sodium intake … is related to blood pressure — would predict [these] associations.”
In their response, published in the same issue, Stamler and his colleagues insisted that their corrections were legitimate because the “totality of the evidence — the only sound basis for judgment on this matter — supports the conclusion that this association is causal.” They cited the “independent expert groups, national and international,” that had concluded habitual high salt intake was a causal factor of high blood pressure, although they neglected to mention that those groups had all relied on Intersalt circa 1988 to reach their conclusions. Intersalt also listed seven reasons why their original estimate was “probably underestimated” but seemed to make no attempt to find reasons why it might have been overestimated. “It was embarrassing to read,” Harvard School of Public Health epidemiologist Jamie Robins told Science, while describing Intersalt’s arguments as “arcane, bizarre, and special pleading.”
The commentary and response led to yet more letters in the BMJ the following August. Now Davey Smith and Phillips were joined by a half-dozen other researchers criticizing Intersalt Revisited, such as Nick Day, head of the biostatistics unit of the British Medical Research Council (MRC) in Oxford. “As soon as you start making big corrections [to your original findings],” says Day, “people begin to get suspicious.”
Day describes the problem with Intersalt Revisited as one of “garbage in, garbage out” and believed it had implications well beyond the salt controversy: Stamler and his colleagues, like many epidemiologists, assumed they could correct for underlying uncertainties in their data with statistical methods. “It doesn’t work,” he says. “There will always be uncertainty surrounding what you’ve done, and if what you’ve done makes quite a serious difference to the crude observed relationships, then it puts a great haze of doubt over the whole thing. If you have an underlying uncertainty — that is, ‘garbage in’ — it is never going to be refined into gold.”
This assessment is rejected by Stamler and most of his Intersalt Revisited co-authors, although not all of them. Michael Marmot, for instance, an epidemiologist at the University College London Medical School and a signatory of Intersalt Revisited, told Science that, in retrospect, the reanalysis was not compelling. “Somebody looking at this from the outside,” he says, “could well take the view that [the corrections] were done for one reason alone, which was to increase the size of the associations. They would not be crazy for taking such a view just based on reading the paper.”
Trials and tribulations
In the grand scheme of the salt controversy, a study such as Intersalt, revisited or not, should have been irrelevant. After all, as researchers on both sides agree, Intersalt was an observational study showing at best weak associations in a field of research where randomized, controlled clinical trials — the “gold standard” of epidemiology — should be able to establish a cause and effect, if any exists. “You kind of can’t believe it’s an issue,” says Robins, for instance. “They can actually run randomized experiments [on salt reduction], and they’ve run lots of them.” All a researcher needs is to randomize subjects into two groups, one reducing salt intake, one eating normally, and then see what happens.
But the results were as ambiguous as anything else in the salt dispute. Doing the trials correctly turned out to be surprisingly difficult. Choosing low-salt foods, for instance, inevitably leads to changing other nutrients, as well, such as potassium, fiber, and calories. Placebo effects and subtle medical intervention effects have to be avoided carefully. “If you just study people for 10 weeks, you will detect some changes over time which have nothing to do with the experiment you’re carrying out,” says Graham Watt, who in the mid-1980s ran three of the first double-blind, placebo-controlled trials on salt reduction.
A technique known as meta-analysis has lately become the route to clarity in such situations. The idea is that if a host of clinical trials gives ambiguous results, the true size of the effect might be assessed by pooling the data from all the studies in such a way as to gain statistical power. But meta-analysis is controversial in its own right. It might have been the ideal solution to the salt controversy had not the salt controversy turned out to be the ideal situation to demonstrate the questionable nature of meta-analysis. As Harvard School of Public Health epidemiologist Charles Hennekens puts it: “It’s all so arbitrary, and you’d like to believe it’s arbitrary in a random way, but it turns out to be arbitrary in the way the investigators want it to be.”
In 1991, Cutler, Elliot, and collaborators generated the first meta-analysis of randomized clinical trials on the salt question. They found 21 trials in hypertensive subjects, although only six were placebo-controlled, and six in normotensives, of which only those done by Watt were double-blind and placebo-controlled, and those showed zero benefit from salt reduction. By amassing these trials together, however, the controlled with the uncontrolled, Cutler and Elliot deduced that a 3- to 6-gram reduction in daily salt consumption would drop blood pressure by 5/3 mmHg in hypertensives and 2/1 mmHg in normotensives. This relationship was “likely to be causal,” they then concluded, because “the results are consistent with a large body of epidemiological, physiological, and animal experimental evidence.” This, of course, was exactly the point of contention.
Cutler’s meta-analysis was promptly overshadowed by the three-part extravaganza published in the BMJ in April 1991 by Malcolm Law and his colleagues. Their conclusions were unprecedented: They deduced that salt reduction has an effect on blood pressure nearly double that found by Cutler and Elliot. Law and his colleagues predicted that “moderate” universal salt reduction — cutting daily intake by only 3 grams — would benefit the population more than treating all hypertensives with drugs, while cutting intake by 6 grams a day would prevent 75,000 deaths a year in Britain alone.
They derived these conclusions in three steps. First, they analyzed the ecologic studies to estimate the average apparent effect of salt on blood pressure. They then “quantitatively reconciled” this estimate with the numbers derived from the intrapopulation studies after suitably correcting those upward for regression dilution bias. Having demonstrated that the ecologic and intrapopulation studies were not in fact contradictory, as had been believed for 20 years, they then proceeded to determine whether this reconciled estimate was consistent with all the relevant clinical trials. These, says Law, turned out to be dead on, thus demonstrating that all studies were in agreement about the considerable benefits of salt reduction.
Although this “quantitative review,” as Law calls it, has its supporters, they are in a minority. Its critics — including epidemiologists and statisticians who read the paper at the request of Science — insist the work is so flawed as to be effectively meaningless. Take the selection of which studies to include and which to discard: In the analysis of the ecologic studies, Law and his colleagues chose 23 studies done between 1960 and 1984, and one from Szechuan, China, published in 1937. They then excluded Intersalt, the mother of all ecologic studies, from the analysis because its well-calibrated, standardized blood pressure measurements often yielded numbers 15 mmHg lower than those made in comparable communities by the older, uncalibrated, nonstandardized studies. Critics likened this decision to tossing the baby and keeping the bath water. Law told Science that they excluded Intersalt because the original results were “inadequate” and “too low,” but that this was not the case with “Intersalt Revisited,” a study he would have included had it been available.
As for the analysis of clinical trials, noted Swales, Law and his colleagues synthesized the results of 78 trials, of which only 10 were actually randomized. One study even predated the era of modern clinical research. The fall in blood pressure that Law and his colleagues attributed to sodium, says Swales, was likely due to the “impact of poor controls.” Even Richard Smith, the BMJ editor who published the research, described it to Science as “not the best we’ve ever done.”
Intersalt “did not show blood pressure increases if you eat a lot of salt.”
—Lennart Hansson
“The position has been clarified; all the Intersalt analyses confirm salt as an important determinant of blood pressure.”
—Malcolm Law
Law, however, says the study has stood up well, noting that its findings agree with those of Intersalt Revisited. And despite the critiques, Law’s meta-analysis is still one of the most highly cited papers in the salt literature and was one of the bedrocks — along with Intersalt, the study Law considered inadequate — of the 1993 NHBPEP primary prevention report.
Poles apart
Over the past 5 years, two conspicuous trends have characterized the salt dispute: On the one hand, the data are becoming increasingly consistent suggesting at most a small benefit from salt reduction — while on the other, the interpretations of the data, and the field itself, have remained polarized. This was vividly demonstrated by two more salt-blood pressure meta-analyses. In 1993, with the appearance of the NHBPEP primary prevention report, the Campbell’s Soup Co. enlisted the University of Toronto’s Logan to do the first of them. Logan had studied salt reduction in the early 1980s and found it to be of “very little” use. With funding from Campbell’s, he now identified 28 randomized trials in normotensives and 28 in hypertensives. Meanwhile, Cutler learned of Logan’s new analysis and countered by updating his own.
The results of the two studies were virtually identical — or at least, “more similar than they are different,” says Cutler, who based his new meta-analysis on 32 relevant studies. For a reduction of roughly 6 grams of salt, Cutler claimed the trials demonstrated a blood pressure benefit of 5.8/2.5 mmHg in hypertensives and 2.0/1.4 mmHg in normotensives. Logan claimed a benefit of 3.7/0.9 mmHg in hypertensives and 1.0/0.1 in normotensives. Considering the possible errors, says Robins, “those are the same data. The rest is smoke and mirrors.”
Logan and Cutler then went about interpreting the data in opposite ways that happened to coincide with their established opinions. Logan and his collaborators noted that these estimates were probably biased upward by negative publication bias — in which studies finding no effect are not published — and by a placebo effect. They said there was some evidence suggesting that sodium restriction might be harmful and concluded that “dietary sodium restriction for older hypertensive individuals might be considered, but the evidence in the normotensive population does not support current recommendations for universal dietary sodium restriction.” Cutler and his colleagues claimed that the numbers did not appear to be biased upward by either a placebo effect or a negative publication bias. They said there was no evidence suggesting that salt reduction can be harmful and concluded that the data supported a recommendation of sodium restriction for both normotensives and hypertensives.
Logan’s paper got the better press, because it contradicted the established wisdom and was published in JAMA in 1996, a year before Cutler’s paper appeared in the American Journal of Clinical Nutrition. But advocates of salt reduction — notably Graham MacGregor of St. George’s Hospital Medical School in London, author of two popular cookbooks on low-salt and no-salt diets — suggested to reporters that Logan’s meta-analysis could not be trusted because of a conflict of interest from the Campbell’s funding. In a JAMA editorial accompanying Logan’s meta-analysis, NHLBI director Claude Lenfant recommended that the study be ignored, in any case, on the familiar grounds that “the preponderance of evidence continues to indicate that modest reduction of sodium … would improve public health.”
Despite Lenfant’s assessment, the latest salt studies seem to agree with the negligible benefit of salt reduction suggested by Logan’s interpretation. That was the bottom line of the University of Copenhagen meta-analysis, published in JAMA in May, and also of the NHLBI-funded Trials of Hypertension Prevention Phase II (TOHP II) published in March 1997. TOHP II, a 3-year clinical trial of 2400 people with “high normal” blood pressure, coordinated by Hennekens at Harvard Medical School, found that a 4-gram reduction in daily salt intake correlated with a 2.9/1.6-mmHg drop in blood pressure after 6 months. That benefit, however, had mostly vanished by 36 months, and Hennekens agrees that it could have been due to a medical intervention effect.
Of all these studies, the one that may finally change the tenor of the salt debate was not actually about salt. Called DASH, for Dietary Approaches to Stop Hypertension, it was published in April 1997 in The New England Journal of Medicine. DASH suggested that although diet can strongly influence blood pressure, salt may not be a player. In DASH, individuals were fed a diet rich in fruits, vegetables, and low-fat dairy products. In 3 weeks, the diet reduced blood pressure by 5.5/3.0 mmHg in subjects with mild hypertension and 11.4/5.5 mmHg in hypertensives — a benefit surpassing what could be achieved by medication. Yet salt content was kept constant in the DASH diets, which meant salt had nothing to do with the blood pressure reductions.
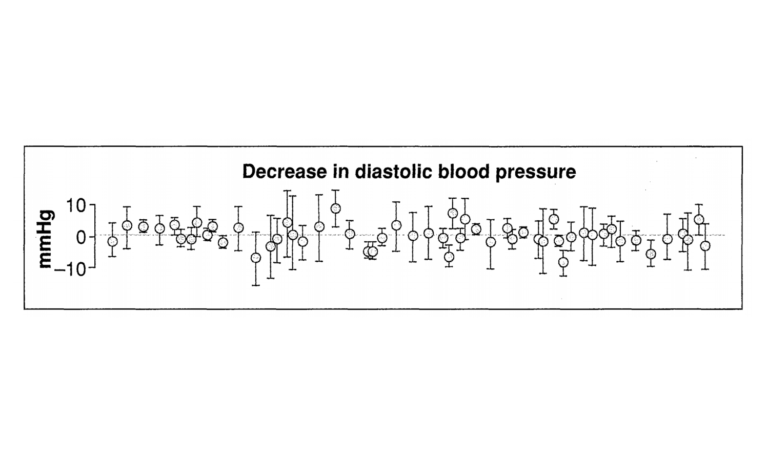
Figure 3: Adding up the evidence. In a meta-analysis of 56 clinical trials done since 1980 in people with normal blood pressure, extreme salt reduction offered little benefit. (Source: Graudal et al., JAMA)
Indeed, if the DASH results stand up, says Day, they suggest that fruits and vegetables may be the true cause of the effects attributed to salt in the old ecologic studies. Societies that have high salt intakes tend to consume highly salted preserved foods simply because they do not have year-round access to fruits and vegetables. Now the DASH collaboration has embarked on a follow-up to differentiate the effects of salt from those of the DASH diet. The researchers are working with 400 subjects, randomized to either a control diet or the DASH diet and to three different levels of salt intake — 3, 6, or 9 grams daily. Results are expected in 2 years.
“We’re all being pushed by people who say, ‘Give me the simple answer. Is it or isn’t it?’ “
—Bill Harlan
Picking your battles
In 1976, when the salt controversy was new, Jean Mayer, then president of Tufts University, called salt “the most dangerous food additive of all.” Today the debate has devolved into an argument over whether extreme reductions in salt intake, perhaps impossible to achieve in the general population, can drop blood pressure by as much as 1 or 2 millimeters of mercury, and if so, whether anyone should do anything about it. For people with normal blood pressure, such a benefit is meaningless; for hypertensives, clinicians say that medications have a much greater effect at a cost of a few cents a day. But what works for the individual and what works for public health are still two different things. To Stamler, for instance, or Cutler, there is no question that a population that avoids salt will have less heart disease and strokes. And salt intake, they argue, is far easier to change than, say, smoking or inactivity, because much can be accomplished by convincing industry to put less salt in processed foods.
“As long as there are things in the media that say the salt controversy continues, the [salt interests] win.”
—Jeff Cutler
Whether it’s worth it is the question. For the agencies involved to induce the public to avoid salt, they must convince individuals that it’s bad for their individual health, which, for those with normal blood pressure, it almost assuredly isn’t. Although this explains the single-mindedness of the promotional message out of the NHLBI and NHBPEP, it can also make the agencies and administrators look disingenuous. Moreover, public health experts firmly believe that the public can only be sold so many health recommendations. “How much of the government’s moral weight do you expend on this particular issue?” says University of Toronto epidemiologist David Naylor. “You have to pick your battles. Is this a battle worth fighting?” Hammering on the benefits of salt reduction, say Naylor, Hennekens, and others, may come at the expense of advocating weight loss, healthy diets in general, and other steps that are significantly more beneficial.
The argument that salt reduction is a painless route to lower blood pressure also assumes that there is no downside to this kind of social engineering. Social interventions can have unintended consequences, notes NIH’s Harlan, which seemed to be the case, for instance, with the recommendation that the public consume less dietary fat. “It was a startling change to a lot of us,” Harlan says, “to see the proportion of fat in the diet go down and weight go up. Obviously it’s not as simple as it once seemed.”
The last 5 years have also seen two studies published — the latest this past March in The Lancet — suggesting that low-salt diets can increase mortality. Both studies were done by Michael Alderman, a hypertension specialist at New York City’s Albert Einstein College of Medicine and president of the American Society of Hypertension. Epidemiologists — and Alderman himself — caution against putting too much stock in the studies. “They are yet more association studies,” says Swales. “Any insult you make of Intersalt you can make of those as well.” But Alderman also notes that only a handful of such studies comparing salt intake to mortality have ever been done, and none have come out definitively negative. “People just rely upon statements that [salt reduction] can’t really do any harm,” says Swales. “It may or may not be true. Individual harmful effects can be as small as beneficial effects, and you can’t detect those in clinical trials either.”
After publication of his second study, Alderman recruited past and present presidents of hypertension societies and the American Heart Association and wrote to Lenfant at the NHLBI “urging prompt appointment of an independent panel of qualified medical and public health scientists to review existing recommendations [on salt consumption] in light of all available data.” In April Lenfant told Science that he had agreed to proceed with the review. If such a panel should convene, Hennekens has one observation worth keeping in mind: “The problem with this field is that people have chosen sides,” he says. “What we ought to do is let the science drive the system rather than the opinions.”
Touchstones of the Salt Debate
- Dahl et al., 1972. Clinical, ecological, and rat studies supporting salt-blood pressure link.
- Gleibermann et al., 1973. Review of 27 ecologic studies suggests a direct linear relationship between salt and blood pressure.
- Cooper et al., 1979. Intrapopulation study of several hundred schoolchildren suggests “not wholly negative” relationship between salt and blood pressure.
- McCarron et al., 1984. Analysis of the National Health and Nutrition Examination Survey database suggests that salt is harmless and that calcium and potassium protect against hypertension.
- Smith et al., 1988 (Scottish Heart Health Study). Study of 7300 Scottish men finds no relationship between salt intake and blood pressure.
- Intersalt, 1988. Study of 52 200-person populations shows weak or no relationship between salt and blood pressure but infers a relationship between salt and the rise in blood pressure with age.
- Intersalt Revisited, 1996. Statistical reanalysis of the original Intersalt data now finds strong, consistent positive association between salt and blood pressure.
- Cutler et al., 1991. Meta-analysis of 27 clinical trials finds that salt reduction lowers blood pressure in both hypertensives and normotensives.
- Law et al., 1991. Review of 24 ecologic studies, 14 intrapopulation studies, and 78 clinical trials finds that salt-blood pressure link is “substantially larger” than generally appreciated and increases with age.
- Midgley et al., 1996. Meta-analysis of 56 clinical trials concludes that benefit from salt reduction is small and does not support current dietary recommendations.
- Cutler et al., 1997. Meta-analysis of 32 clinical trials concludes that benefit of salt reduction is larger and does support current dietary recommendations.
- Trials of Hypertension Prevention Collaborative Research Group, 1997 (TOHP II). Clinical trial in 2400 subjects indicates that long-term reductions in salt intake are hard to maintain and result in little or no reduction in blood pressure.
- Appel et al., 1997 (DASH). Clinical trial of 459 people shows that dietary factors other than sodium have a much greater effect on blood pressure.
- Graudal et al., 1998. Meta-analysis of 114 clinical trials does not support a general recommendation to reduce salt intake.
Click here to view the original PDF of the article.
Click here to see the original discussion of the article from Aug. 23, 2003, on CrossFit.com.