As previously noted in Part 1 of this series, my life changed at the end of June 1981 when I received a letter from a 46-year-old female runner of 108 lb. who had experienced never-before-described symptoms during the 56-mile Comrades Marathon.
She told me that late on the afternoon of June 1, 1981, she fell into a coma and was admitted to a hospital following her participation in that year’s marathon. Twelve miles from the finish, she failed to recognize her husband, who had come to assist her. He convinced her to stop running and drove her to the medical facility at the race finish. There, she received 2 liters of fluid, administered intravenously for treatment of “dehydration” that was then—and continues to be now—the expected cause of all complications that occur during prolonged exercise (1).
Her husband, noting that her condition worsened after she received the intravenous fluids, decided to take action. He wanted her to be admitted to a hospital in Durban, South Africa, where the race had started. But on the drive back to Durban, the runner suffered a grand mal epileptic seizure and lapsed into a coma. She was admitted to the hospital, where blood testing found her serum sodium concentration to be reduced to 115 mmol/L; a chest X-ray indicated the presence of “water in the lungs” (pulmonary oedema), confirming a diagnosis of exercise-associated hyponatremic encephalopathy (EAHE), the first such known case. Treated very conservatively, her serum sodium concentration returned to the normal range, and she regained consciousness on the fourth day in hospital. She was discharged from the hospital, fully recovered, a further two days later, six days after she had begun the Comrades Marathon in perfect health.
When this runner wrote to me, she asked, “What happened?” I answered that I had no idea but would investigate.
By 1985 we had made some progress in the investigation. We reported her story and another three similar cases in a paper entitled ‘‘Water intoxication: a possible complication of endurance exercise” (2). Even then, we observed (without direct measurement), “the etiology of the hyponatremia in these runners was due to overhydration.” We concluded with the admonition that “the intake of hypotonic fluids in excess of that required to balance sweat and urine losses may be hazardous in some individuals” (2).
The following year, two doctors who had developed EAHE during the Chicago 80/100-km ultramarathon described their experiences (3). Notably, these doctors had been advised to drink 300–360 mL at each aid station placed 1.6 km apart on the 10-km lap course on which the race was held. They also noted, “In addition, athletes are instructed to drink more than their thirst dictates, since thirst may be an unreliable index of fluid needs during exercise. Runners, as a group, are taught to ‘push fluids.’” As a result, each drank in excess of 20 liters of fluid during the eight to 10 hours they ran. The authors became aware of our earlier study only after their original manuscript had been accepted for publication. Their identical conclusions were developed independently of our own: “The two runners consumed such large quantities of free water during the race that apparent water intoxication developed. … It seems likely that the hyponatremia was caused primarily by increased intake and retention of water and contributed to the sodium loss.”
In a historic coincidence, the senior physician in that report received intravenous hypertonic (3%) saline for the treatment of his EAHE. His serum sodium concentration increased from 118 mmol/L to the normal range (135 mmol/L) within eight hours of hospital admission. He returned to his home in Atlanta the following morning, resuming his medical practice that same afternoon. But his junior colleague was less fortunate. Treated with the less concentrated, normal (0.9%) saline solution intravenously, he remained semi-comatose for 36 hours while his serum sodium concentration remained low. He was discharged from the hospital only on the fifth hospital day, four days later than his senior colleague.
Hence, the first “controlled” clinical trial comparing the effects of isotonic and hypertonic saline in the management of EAHE was completed, by chance, already in 1983 and reported in 1986, antedating by 22 years the conclusion that hypertonic (3-5%) saline solutions are the most appropriate therapy for this condition (4) and the use of less-concentrated saline solutions is absolutely contraindicated (5).
Thus, by 1986 a body of evidence showed:
(a) EAHE is caused by excessive fluid consumption during exercise;
(b) athletes who drink to excess during exercise usually do so on the well-meaning advice of others, including race organizers; and
(c) the condition responds hardly at all to treatment with 0.9% normal saline, whereas recovery is rapid when hypertonic (3–5%) saline solutions are used. It would take almost another 20 years before this wisdom would be universally applied (5).
After 1985, it became apparent to us that EAHE was becoming increasingly common in 56-mile Comrades Marathon runners. Sixteen athletes were admitted to the hospital with EAHE after the 1987 race. Accordingly, we decided to follow the fluid and sodium balance during recovery of all runners admitted to the hospital for the treatment of EAHE after the 1988 Comrades Marathon. We specifically hoped to determine whether the initial conclusions from the first case reports were correct.
The report of that study, published in 1991 (6), came to the following unambiguous conclusion:
This study conclusively resolves this issue (of what causes EAHE). It shows that each of eight athletes who collapsed with hyponatremia of exercise (mean plasma sodium concentration of 122.4 mmol/L) was fluid overloaded by an amount ranging from 1.22 to 5.92 liters. These fluid volumes are conservative because no allowance was made for insensible water losses during recovery. The subjects conservatively estimated that their fluid intakes during exercise ranged from 0.8 to 1.3 L/h, compared with maximum values of 0.6 L/h in normonatremic runners. We also found that the subjects’ sodium losses (153 mmol) were not larger than those of runners who maintained normonatremia during exercise.
Thus, it was concluded that “the hyponatremia of exercise results from fluid retention in subjects who ingest abnormally large fluid volumes during prolonged exercise.”
In our youthful naivety, we assumed this would be the end of the matter—that these definitive findings would be universally embraced and preventive actions based on our conclusions would be enacted immediately around the world, with the result that EAHE would disappear as quickly as it had emerged.
With minimum resources and little direct funding, including none from the sports drink industry, my colleague Dr. Dale (Benjamin) Speedy took up the challenge of testing our findings in a series of studies of New Zealand Ironman triathletes. Whereas we had been able to study just tens of athletes in competition, his team chose to study many hundreds. By applying simple but relevant measurements to large numbers of subjects in a series of groundbreaking studies, Dr. Speedy’s team confirmed that EAH and EAHE had become common in Ironman finishers; that female athletes are especially at risk; and that the cause is fluid retention from excessive fluid consumption during events lasting more than four hours (7-11).
What is more, his team was able to show that simply by (a) advising the athletes not to overdrink during competition and (b) restricting fluid availability during the cycling and running legs of the race, the number of cases of EAHE requiring hospital admission was reduced from 14 in the 1997 New Zealand Ironman to three the following year. There also was no evidence that this advice increased the number of athletes requiring medical care because they drank too little during exercise and had become “dangerously dehydrated.” Instead, as is usually found, the most “dehydrated” triathletes usually won these races.
Discovering the Cause of EAH and EAHE Did not Prevent an Increase in These Conditions in the U.S. Military in the 1990s
Just as these successes were occurring, the incidence of EAH and EAHE was increasing dramatically in the U.S. military, with 125 cases of EAHE requiring hospital admission between 1989 and 1996 (12). In addition, there were at least six recorded deaths (13-15).
Of these 125 cases, 40 occurred at a single training facility: Fort Benning in Georgia. Evaluation of these 40 cases showed, “(1) all were associated with excessive water intake; (2) the training cadre often mistook hyponatremia for dehydration, and; (3) afflicted trainees were not given (appropriate) medical care in a timely manner” (13).
Suitably alarmed, the U.S.military correctly concluded that the introduction of their novel drinking guidelines, as I described earlier (16), were at fault. As a result, revised guidelines were introduced in April 1998. These new guidelines set upper limits of fluid consumption at 1–1.5 quarts per hour (909–1364 mL/h) and 12 quarts (10.9 liters) per day. The impact was immediate. The incidence of hyponatremia in the U.S. Army fell in 1998 and 1999, with most of the reduction occurring as a result of the immediate adoption of these new guidelines at Fort Benning.
However, a report published in March 2018 (17) shows that cases of EAH and EAHE still are happening at Fort Benning. In the words of Maj. (Dr.) Meghan Galer:
In an effort to prevent heat stroke, we have this culture of drink water, drink water, drink water. But if you drink too much water, you basically dilute the electrolytes in your body, specifically the sodium. When that happens, fluid shifts in your body, specifically in your brain, and your brain swells, and because of your skull, it has nowhere to go. This condition is known has hyponatremia and can be caused by someone over-hydrating.
To prevent Emergency Medical Service (EMS) personnel from giving potentially life-threatening intravenous fluids to collapsed soldiers with EAH or EAHE, Galer added the crucial first step that we had proposed as the standard of care in 2005 (5): Specifically, before anyone who collapses during prolonged exercise (more than three hours) is given intravenous fluids, it is essential that their blood sodium concentration be measured to rule out EAH or EAHE. Galer insisted: “Our medics, or anyone at the scene, are not allowed to give more than one liter of ice-cold fluid until they know what the patient’s sodium is.” As a result, Fort Benning EMS personnel must now carry with them an iStat machine, which provides a real-time measurement of the patient’s blood-sodium concentration. It is worth noting that these Fort Benning changes also occurred in response to CrossFit’s hydration conference and its proposed strategies for avoiding EAH and EAHE.
Of course, a simpler precaution would be simply to prevent the condition from happening in the first place by telling the soldiers to “drink to thirst.” There has never been any evidence that drinking any amount of fluid—either too little or too much or just the right amount—prevents or causes heatstroke. In fact, we have reported the only known case in the world in which a soldier died from the combined effects of heatstroke and EAHE (18). Tragically, the overdrinking that caused this soldier’s EAHE did not prevent his fatal heatstroke.
The evidence that excessive fluid replacement cannot prevent heatstroke is reviewed fully in Waterlogged (19), first published in 2012.
The American College of Sports Medicine Ignores These Findings, With Predictable Outcomes
In 1996, the American College of Sports Medicine (ACSM), an organization whose only two “platinum” sponsors at the time were Gatorade and the Gatorade Sports Science Institute (GSSI), produced its modified Position Stands, which promoted the concept that subjects should drink “as much as tolerable” during exercise (20, 21). This was linked to an extensive marketing campaign, directed by the sports drink industry through the GSSI (22), to promote this new advice.
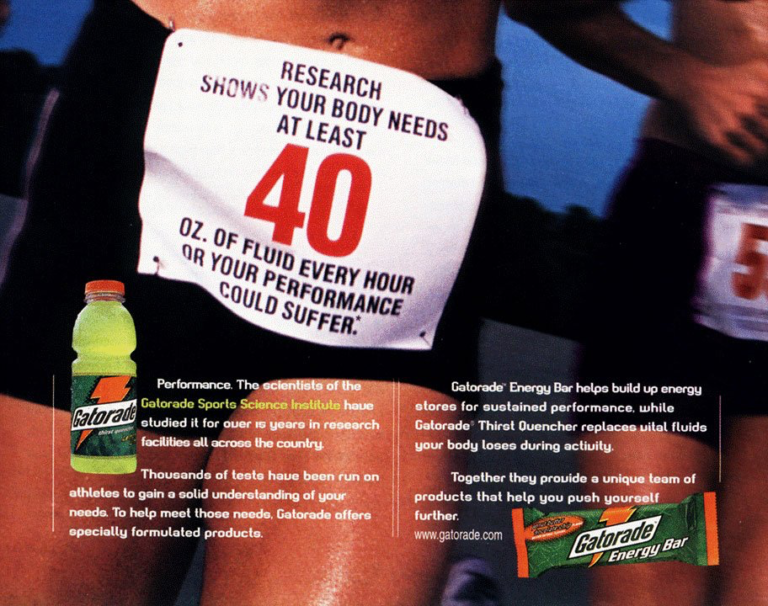
d
The focus of this advice was to prevent heatstroke during exercise. This, in turn, was based on the false idea that dehydration causes heatstroke by reducing the human capacity to lose heat during exercise. According to that theory, dehydration impairs heart function, reducing blood flow to the skin and thus impairing the sweat function. Neither of these outcomes has ever been proven, however. Instead, it is established that typical levels of exercise-induced dehydration do not reduce sweat rates (23-28), meaning that this (false) model cannot explain why heatstroke develops during exercise. The model is equally insufficient for explaining why drinking to excess as promoted by the Water as a Tactical Weapon Doctrine (16) will not prevent heatstroke (18).
An alternative explanation is that humans developed the capacity to sweat copiously during exercise specifically to protect from the development of heatstroke during exercise in the heat. As Bernd Heinrich describes:
The fact that we, as savanna-adapted animals have such hypertrophied sweating responses implies that, if we are naturally so profligate (wasteful – my addition) with water, it can only be because of some very big advantage. The most likely advantage was that it permitted us to perform prolonged exercise in the heat. We do not need a sweating response to outrun predators, because that requires relatively short, fast sprinting, where accumulating a heat load is, like a lactic acid load, acceptable. What we do need sweating for is to sustain running in the heat of the day—the time when most predators retire into the shade. (29)
Heinrich also notes that modern hunter-gatherers, like the !Kung San Bushmen of Southern Africa, “carry no food or water with them (on 30-km hunts in the heat) because that hinders their ability to travel.”
In retrospect, the scientists who drew up the 1996 ACSM Position Stands disrupted our understanding of normal physiology in order to promote the Zero-Percent Dehydration Doctrine (30). They ignored the known physiological principle that all the body’s responses during exercise, including body temperature and blood sodium concentrations, are homeostatically regulated, and that weight loss as a result of sweating is an essential component of that homeostatic regulation. Instead, as a consequence of this industry-driven subversion, subsequent generations of exercise scientists have been taught that body weight is the critical variable that must be defended at all costs during exercise (31, 32).
But attempting to maintain the body weight during exercise by drinking “as much as tolerable” prevents homeostatic control of blood sodium concentration, leading to EAH and EAHE.
Unfortunately, the paradigm shift occasioned by the ACSM Position Stands and as championed by the GSSI happened at the very time that marathon running, particularly in the U.S., underwent its most fundamental change since 1976. Before 1976, there were few runners in marathon races, and most were usually well-trained and able to finish the 42 km in less than 3.5 hours.
Since 1996, this has changed so that most current marathon runners in the U.S. require four or five or more hours to complete these distances (33). In publishing its Position Stands, the ACSM promoted the concept that it was a good idea for less well-conditioned athletes traveling at slow speeds (8–9 km/h) for prolonged periods (4.5 hours) to drink “as much as tolerable” to prevent a condition (heatstroke) that occurs rarely in such slow runners and is not caused by dehydration (18). The result was predictable.
The first reported death from EAHE occurred in a female runner, as I had predicted, in the Valley of the Giants marathon in California in 1993 (34). Besides the deaths in the U.S. military, this was followed by three additional deaths reported in female runners in U.S. marathons: Dr. Kelly Barrett in the 1998 Chicago Marathon (35), Dr. Cynthia Lucero in the 2002 Boston Marathon (36), and six months later under essentially identical conditions, Hilary Bellamy in the 2002 Marine Corps Marathon (37). Each of these women reportedly (34, 37) received intravenous isotonic saline solutions for treatment of EAHE, a treatment established to be ineffective already in 1985 (2, 3). The correct treatment of EAH is either to do nothing if the condition is mild and the patient does not have EAHE, or to infuse hypertonic saline solutions (3–5%) in modest amounts (4, 5), with or without the use of diuretics.
How long these preventable catastrophes might have continued to occur is anyone’s guess. But fortunately, at the same race in which Lucero participated, a group of enthusiastic hospital residents from the Harvard Medical School decided to perform what would become the definitive study (38). They chose a large sample size of runners and included questions that could be analyzed retrospectively to determine predictors of post-race serum-sodium concentrations.
The crucial difference between this and all previous studies of EAH was that the Harvard Medical School study leapt across the gargantuan divide between sports science and clinical medicine and was published in arguably the most influential medical journal in the world, the New England Journal of Medicine. The authors’ conclusions were the following:
(1) EAH occurred in a substantial fraction of the diverse athletic population studied.
The authors calculated that, if their sample was representative of all 15,000 finishers in the 2002 Boston Marathon, approximately 1,900 of those runners would have developed EAH and about 90 would have developed “critical” EAHE (serum-sodium concentration of 120 mmol/L or less). This contrasts with the commercially driven conclusion that EAH is uncommon and much less prevalent than conditions caused by “dehydration.”
For example, in a press release published on the GSSI website on the day that my peer-reviewed editorial was published in the British Medical Journal (39), the GSSI proposed that “Dr Noake’s (sic) editorial is not representative of the comprehensive research that is available on the topic of hydration during exercise. Nor does it factor in the very real dangers associated with the more common condition of dehydration” (40).
This is perhaps understandable, as the editorial dealt with the proven dangers of overhydration and not the commercially driven and scientifically unsound claims for the dangers of dehydration (18).
The GSSI press release concluded: “In summary, there is no doubt that hyponatremia is a rare but dangerous condition that affects a very, very small subset of the population. However, dehydration and heat illness occur more frequently and represent the greater threat to anyone who is physically active in a warm environment.”
It is perhaps stretching the truth to suggest that a preventable condition that affects 13% of runners and might possibly have involved 1,900 runners, 90 seriously (38), in a single race, is “rare.” Whereas it might appear “rare” to a sports drink company, whose product was the official race drink for that particular event, the doctors treating such an unnecessary case load might indeed be of a different opinion.
(2) “Substantial weight gain appeared to be the most important predictor of hyponatremia and correlated with increased fluid intake.”
(3) The nature of the fluid ingested did not influence the risk of EAH.
(4) Race time in excess of four hours increased the risk of EAH. As a result, the authors concluded that EAH may be a preventable condition through “efforts to monitor and regulate fluid intake.”
These conclusions mirrored those of our original studies and the content of my editorial in the British Medical Journal (39), published 21 months earlier, which stated:
[T]he athlete most likely to develop hyponatremic encephalopathy is a female marathon runner who runs these 42 km races at speeds slower than 8–9 km/h (about 5 mph). She gains weight during exercise because she drinks excessively both before and during exercise, sometimes in excess of 100 cups of fluid during the race (about 15 liters of fluid during five to six hours of exercise) … since the cause of the condition is now known, prevention is possible.
An Unexplained Puzzle
It is puzzling that while the U.S. military was becoming increasingly aware of the dangers of overdrinking as the sole cause of EAH and EAHE after 1993, the ACSM was encouraging distance runners to (a) drink more according to the Zero-Percent Dehydration Doctrine (30) and (b) ingest more sodium chloride during exercise in order to prevent EAH and EAHE. The question then becomes: From whom were these two different organizations receiving this contradictory scientific advice?
Interestingly, the first (senior) authors of the ACSM’s 1996 Position Stands (20, 21) were either employed by the U.S. military (Dr. Victor Convertino) or had worked at the U.S. Army Research Institute for Environmental Medicine (USARIEM) (Dr. Lawrence Armstrong). The senior author of one of the 2007 Position Stands (42) was once again Armstrong, who was joined by Dr. Michael Sawka, a USARIEM employee. Of the 12 authors of the 2007 Position Stands (42, 43), four were employees of USARIEM (and another seven had declared links to the U.S. sports drink industry). Furthermore, between 2004 and 2009, Drs. Pandolf and Young of USARIEM were the senior editors of the journal Medicine and Science in Sports and Exercise in which these guidelines were published.
During this period Gatorade was producing special prepacked “care” packs for “troops in battle fields or boot camps requiring on-the-go hydration to replace nutrients and carbohydrates loss [sic] during exercise and battle” (44). What is more: “Record heat and sales to the military overseas led to a shortage of Gatorade in 2005” (45).
Since the U.S. military provides a captive market for Gatorade products, it would only be sensible for that company to develop a special relationship with relevant groups in the U.S. military, as it has with the ACSM and related organizations. Perhaps this explains why these tight relationships came into being and were sustained during the writing of these different Position Stands.
It seems fair to conclude that after 1987, USARIEM scientists — either current employees or past students or other employees of the U.S. military — became increasingly influential in the development of the ACSM Position Stands on fluids and exercise. To their credit, by 2007 they were able to convince the ACSM that athletes should not be encouraged to drink “as much as tolerable” but only according to the dictates of thirst (provided that a weight loss greater than 2% was not incurred).
But the question remains: Why did Armstrong and Convertino, both with links to either USARIEM or the U.S. military, allow the adoption of the ACSM’s “Zero-Percent Dehydration Doctrine” in 1996 when both must have had some inkling of the damage the 1988 drinking guidelines had caused in the U.S. Army? And why did USARIEM promote a model claiming prolonged exercise in the heat could cause EAH as a result of dehydration and large sodium chloride losses in sweat (Figure 9.12 in reference 19) even though two of the authors of that model, Sawka and Dr. Scott Montain, did not advise the U.S. military to increase the sodium intakes of soldiers during exercise to prevent EAH and EAHE?
Instead, both scientists had written that cases of EAH and EAHE in the U.S. military were due to “water intoxication (hyposmolality/hyponatremia) … suggesting that fluid replacement guidelines might need adjustment to prevent overdrinking” (46). The cited article contains no single mention of sodium losses as a cause of EAH and EAHE. Drs. Montain, Latzka, and Sawka had also written in 1999, “Calculations indicate that total body water must have increased by 3 to 5 liters to achieve such low serum-sodium values (in U.S. military personnel with EAH – my addition)” (12).
This raises a further interesting question: If Sawka believed that water intoxication alone causes EAH and EAHE in soldiers, why did he allow the 2007 ACSM Position Stand to include the advice that runners should increase sodium intake during exercise to prevent both conditions?
It is as if he and Montain believe that soldiers and runners belong to a different species of Homo sapiens who develop EAH and EAHE for different reasons when they exercise for prolonged periods in the heat.
Conclusions
History is replete with examples of correct ideas that were not accepted until subsequent generations confirmed their validity. Usually, there is a logical reason for this delayed acceptance; often the fault lies with the researchers themselves.
Typically, this is a matter of timing. New ideas are not accepted immediately simply because they are correct. It is said instead, “Science progresses one funeral at a time.” The proponents of the old ideas must first die before that which they taught their students can be replaced.
An editorial essentially identical to that ultimately published in the British Medical Journal (39) was submitted to the New England Journal of Medicine about two years earlier, following the death of Barrett in the 1998 Chicago Marathon (35). But this article antedated the death of Lucero at the 2002 Boston Marathon (36) and hence was too early, too improbable, and advanced by scientists who were geographically too distant from the perceived center of global medical science.
What we have learned is that in the face of such a message, and pitted against the power of modern marketing (40), an opposing scientific message will not be heard.
In this case, only the death of Lucero in very public circumstances produced the tipping point that exposed the concealed truth. We will consider this tragic occurrence further at a later date.
Additional Reading
- The Hyponatremia of Exercise, Part 1
- The Hyponatremia of Exercise, Part 2
- The Hyponatremia of Exercise, Part 3
- The Hyponatremia of Exercise, Part 4
- The Hyponatremia of Exercise, Part 5
- The Hyponatremia of Exercise, Part 6
- The Hyponatremia of Exercise, Part 7
- The Hyponatremia of Exercise, Part 9
- The Hyponatremia of Exercise, Part 10
- The Hyponatremia of Exercise, Part 11
- The Hyponatremia of Exercise, Part 12
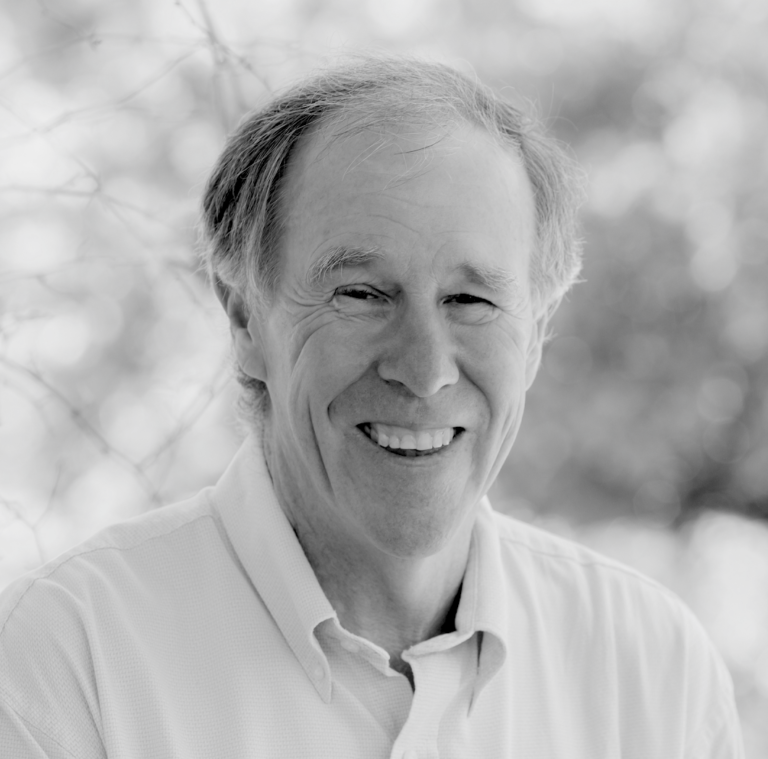
Professor T.D. Noakes (OMS, MBChB, MD, D.Sc., Ph.D.[hc], FACSM, [hon] FFSEM UK, [hon] FFSEM Ire) studied at the University of Cape Town (UCT), obtaining a MBChB degree and an MD and DSc (Med) in Exercise Science. He is now an Emeritus Professor at UCT, following his retirement from the Research Unit of Exercise Science and Sports Medicine. In 1995, he was a co-founder of the now-prestigious Sports Science Institute of South Africa (SSISA). He has been rated an A1 scientist by the National Research Foundation of SA (NRF) for a second five-year term. In 2008, he received the Order of Mapungubwe, Silver, from the President of South Africa for his “excellent contribution in the field of sports and the science of physical exercise.”
Noakes has published more than 750 scientific books and articles. He has been cited more than 16,000 times in scientific literature and has an H-index of 71. He has won numerous awards over the years and made himself available on many editorial boards. He has authored many books, including Lore of Running (4th Edition), considered to be the “bible” for runners; his autobiography, Challenging Beliefs: Memoirs of a Career; Waterlogged: The Serious Problem of Overhydration in Endurance Sports (in 2012); and The Real Meal Revolution (in 2013).
Following the publication of the best-selling The Real Meal Revolution, he founded The Noakes Foundation, the focus of which is to support high quality research of the low-carbohydrate, high-fat diet, especially for those with insulin resistance.
He is highly acclaimed in his field and, at age 67, still is physically active, taking part in races up to 21 km as well as regular CrossFit training.
References
- Noakes TD. Comrades makes medical history – again. S A Runner 4(1981): 8–10.
- Noakes TD, Goodwin N, Rayner BL, et al. Water intoxication: A possible complication during endurance exercise. Med. Sci. Sports Exerc. 17(1985): 370-375.
- Frizzell RT, Lang GH, Lowance DC, et al. Hyponatremia and ultramarathon running. JAMA 255(1986): 772–774.
- Ayus JC, Arieff A, Moritz ML Hyponatremia in marathon runners. N Engl J Med 353(2005): 427–428.
- Hew-Butler TD, Almond CS, Ayus JC, et al. Consensus document of the 1st International Exercise-Associated Hyponatremia (EAH) Consensus Symposium, Cape Town, South Africa 2005. Clin J Sport Med 15(2005):207–213.
- Irving RA, Noakes TD, Buck R, et al. Evaluation of renal function and fluid homeostasis during recovery from exercise-induced hyponatremia. J Appl Physiol 70(1991): 342–348.
- Speedy DB, Noakes TD, Rogers IR, et al. Hyponatremia in ultradistance triathletes. Med Sci Sports Exerc 31(1999): 809–815.
- Speedy DB, Noakes TD, Rogers IR, et al. A prospective study of exercise-associated hyponatremia in two ultradistance triathletes. Clin J Sport Med 10(2000): 136–141.
- Speedy DB, Rogers IR, Noakes TD, et al. Exercise-induced hyponatremia in ultradistance triathletes is caused by inappropriate fluid retention. Clin J Sport Med 10(2000): 272–278.
- Speedy DB, Rogers IR, Noakes TD, et al. Diagnosis and prevention of hyponatremia at an ultradistance triathlon. Clin J Sport Med 10(2000): 52–58.
- Speedy DB, Noakes TD, Boswell T, et al. Response to a fluid load in athletes with a history of exercise induced hyponatremia. Med Sci Sports Exerc 33(2001): 1434–1342.
- Montain SJ, Latzka WA, Sawka MN. Fluid replacement recommendations for training in hot weather. Mil Med 164(1999): 502–508.
- Gardner JW. Death by water intoxication. Mil Med 167(2002): 432–434.
- O’Brien KK, Montain SJ, Corr WP, et al. Hyponatremia associated with overhydration in U.S. Army trainees. Mil Med 166(2001): 405–410.
- Garigan TP, Ristedt DE. Death from hyponatremia as a result of acute water intoxication in an Army basic trainee. Mil Med 164(1999): 234–238.
- Noakes TD. The hyponatremia of exercise, part 5. CrossFit.com. Feb. 28, 2019. Available here.
- Garcia M. Fort Benning team determined to end heat-related deaths across. March 20, 2018. Available here.
- Nolte HW, Hew-Butler T, Noakes TD, et al. Exercise-associated hyponatremic encephalopathy and exertional heatstroke in a soldier: high rates of fluid intake during exercise caused rather than prevented a fatal outcome. Phys Sportsmed (2015): 1–6.
- Noakes TD. Waterlogged: The serious problem of overhydration in endurance sports. Champaign, IL: Human Kinetics, 2012.
- Armstrong LE, Epstein Y, Greenleaf JE, et al. American College of Sports Medicine position stand. Heat and cold illnesses during distance running. Med Sci Sports Exerc 28(1996): i–x.
- Convertino VA, Armstrong LE, Coyle EF, et al. American College of Sports Medicine position stand. Exercise and fluid replacement. Med Sci Sports Exerc 28(1996): i–vii.
- Murray B. Fluid replacement: The American College of Sports Medicine position stand. Sports Science Exchange 9(1996): 1–5.
- Ladell WS. The effects of water and salt intake upon the performance of men working in hot and humid environments. J Physiol 127(1955): 11–46.
- Shibasaki M, Kondo N, Crandall CG. Non-thermoregulatory modulation of sweating in humans. Exerc Sport Sci Rev 31(2003): 34–39.
- Costill DL, Kammer WF, Fisher A. Fluid ingestion during distance running. Arch Environ Health 21(1970): 520–525.
- Adolph EF. Water metabolism. Annu Rev Physiol 9(1947): 381–408.
- Eichna LW, Bean WB, Ashe WF, et al. Performance in relation to environmental temperature. Bull Johns Hopkins Hospital 76(1945): 25–58.
- Montain SJ, Coyle EF. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J Appl Physiol 73(1992): 1340–1350.
- Heinrich B. Racing the antelope. New York: Harper Collins, 2001:1–292.
- Noakes TD. The hyponatremia of exercise, part 3. CrossFit.com. Feb. 28, 2019. Available here.
- Baker LB, Munce TA, Kenney WL. Sex differences in voluntary fluid intake by older adults during exercise. Med Sci Sports Exerc 37(2005): 789–796.
- Noakes TD. Sports drinks, the prevention of “voluntary dehydration,” and the development of exercise-associated hyponatremia (EAH). Med Sci Sports Exerc 38(2006): 193.
- Dugas JP. Sodium ingestion and hyponatraemia: sports drinks do not prevent a fall in serum sodium concentration during exercise. Br J Sports Med 40(2006): 372.
- Ayus JC, Varon J, Arieff AI. Hyponatremia, cerebral edema, and noncardiogenic pulmonary edema in marathon runners. Ann Intern Med 132(2000): 711–14.
- Zorn E. Runner’s demise sheds light on deadly myth. Chicago: Chicago Tribune, 1999.
- Smith S. Marathon runner’s death linked to excessive fluid intake. New York Times 13 Aug, 2002.
- Thompson J-A, Wolff AJ. Hyponatremic encephalopathy in a marathon runner. Chest 124(suppl)(2003): 313S.
- Almond CS, Shin AY, Fortescue EB, et al. Hyponatremia among runners in the Boston Marathon. N Engl J Med 352(2005): 1550–1556.
- Noakes TD. Overconsumption of fluids by athletes. BMJ 327(2003): 113–114.
- Gatorade Sports Science Institute. Gatorade Sports Science Institute refutes hydration guidelines in British Journal of Medicine (sic) report. 2003. Originally available at http:// www.pepsico.com/news/gatorade/2003/20030718g.shtml.
- American College of Sports Medicine. Position stand on the prevention of thermal injuries during distance running. Med. Sci. Sports Exerc 19(1987): 529-533.
- Armstrong LE, Casa DJ, Millard-Stafford M, et al. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc 39(2007): 556–572.
- Sawka MN, Burke LM, Eichner ER, et al. American College of Sports Medicine position stand. Exercise and fluid replacement. Med Sci Sports Exerc 39(2007): 377–90.
- Gatorade. Gatorade Orange Military Powder packets—Military Gatorade Sticks. http://www.hydrationdepot.com/Gatorade-Orange-Military-Powder-Packets-Military-Gatorade-Sticks.html, 2010. Accessed March 2019.
- Ingram FC. Company history: The Gatorade Company. http://www.answers.com/topic/the-gatorade-company, 2010. Accessed September 2010.
- Kolka MA, Latzka WA, Montain SJ, et al. Effectiveness of revised fluid replacement guidelines for military training in hot weather. Aviat Space Environ Med 74(2003): 242-246.
The Hyponatremia of Exercise, Part 8