The Evolution of Official Drinking Practices, 1880-2007
Once the Water as a Tactical Weapon Doctrine had been accepted by the U.S. military and received the backing of the influential USARIEM, the challenge for those who saw a commercial advantage in this information was to ensure that the theory became the globally accepted norm, in the guise of the Zero-Percent Dehydration Doctrine.
This would require that these novel doctrines be immunized from the scientific scrutiny and criticism that normally accompany any new theory in the course of “normal” science. Such protection was successfully achieved by having influential organizations like the ACSM and National Athletic Trainers Association (NATA), among others, produce Position Stands that entrenched this paradigm shift as an infallible “truth.” Who would dare challenge the consensus view of the brightest minds in the discipline, all backed by such noble and righteous organizations? Anyone who wished to question those truths clearly was practicing quackery and would be exposed as such.
The result would be that anyone who questioned these novel doctrines was no longer attacking just a scientific theory. Instead, he or she was attacking the dignity and credibility of organizations such as USARIEM, NATA, and the Gatorade Sports Sciences Institute (GSSI)—or even the ACSM, which Gatorade had itself labeled as “the premier organization in sports medicine and exercise science” when it announced its first “gift” of $250,000 to that organization in 1992 (1).
The analogy in modern medicine is the lipid hypothesis, which holds that elevated blood cholesterol concentrations are the major direct cause of heart disease and lowering those concentrations with the prescription of a cholesterol-lowering (statin) drug is the single most important technique in preventing heart disease. This idea is patently false—that is, it is not supported by rigorous, unambiguous scientific findings. But the hypothesis enjoys support from all the major cardiological societies and organizations around the world. Predictably, those entities are heavily funded by the pharmaceutical companies that produce the very drugs that lower blood cholesterol concentrations. Their interest in sustaining the lipid hypothesis is not purely altruistic.
In a similar fashion, benevolent altruism was not the factor driving the adoption of the Zero-Percent Dehydration Doctrine.
Sadly, some highly influential scientists took the easy route and chose to abandon “normal” science during this period. Instead of debating the science, they took to attacking the messenger and may have used their positions as editors or associate editors of major scientific publications to prevent the publication of findings that either challenged or disproved these novel doctrines (2).
These scientists would not necessarily have done this at the direct request of industry. They would do it because, through their scientific publications and public lectures that supported and advanced these novel doctrines, their careers and their egos required that these ideas be correct.
Over the years, I developed Figure 1 to explain how I believe the Position Stands of the ACSM and NATA were initially immunized from criticism, as well as how, in the end, the truth finally broke through, as it usually does (if one gives it enough time).
As British physician and author James le Fanu has written, “[B]iology does not readjust to accommodate the false theories of scientists” (3). If our understanding of the biology is incorrect, and we produce interventions and rigid advice based on our misunderstanding, then ultimately someone is going to suffer.
There always will be consequences.
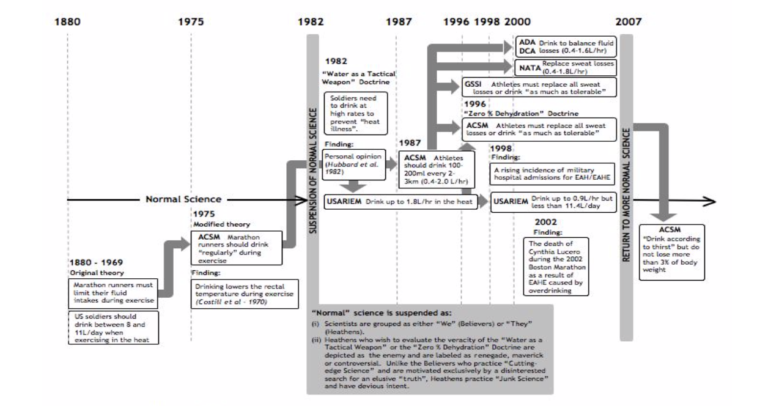
Figure 1: One method that derails “normal” science is having influential organizations incorporate a novel theory into their Positions Stands. This method establishes the unproven theory as “truth” and helps discourage its proper scientific evaluation by disinterested researchers. It establishes a “we” and “they” mentality. Scientists who wish to challenge the novel theory are portrayed as enemies of these organizations, not as disinterested judges. Thus, the adoption of the Water as a Tactical Weapon Doctrine by USARIEM placed USARIEM in a blocking position between the new doctrine and “normal” science. USARIEM was joined soon after 1996 by the ACSM, GSSI, NATA, the American Dietetics Association (ADA), and Dietitians of Canada (DCA), all of whom formed the “we” scientists when the ACSM adopted the Zero-Percent Dehydration Doctrine. As a result, scientists wishing to conduct “normal” science to evaluate the truth of these twin doctrines after 1996 could be dismissed as “they” who were motivated by ambitions other than the search for “truth.” Only after the death of Dr. Cynthia Lucero in the 2002 Boston Marathon and the failure, after 2007, of the Gatorade brand to continue the spectacular growth it experienced in the 1980s and 1990s was there some semblance of a return to “normal” science.
The bottom left corner of Figure 1 shows the period between about 1880 and 1975. I chose 1880 because that is when athletic competitions became organized for the first time. Until 1975, there was little real interest in what athletes should drink during exercise and competition, and it seems that the general advice would have been something like: Do whatever pleases you. For example, at the unique 1976 conference on the New York City (NYC) Marathon (which for the first time traversed the five NYC boroughs), there was very little mention of fluid ingestion during exercise (4, p. 211-213) apart from a presentation by Professor Cyril Wyndham, who warned of the dangers of not drinking during marathon running (5). The idea that drinking during marathon races could provide a performance advantage was still far from anyone’s mind, other than, of course, that of Dr. Robert Cade (6).
The U.S. military, which had fought wars in every possible environment, had its own specific guidelines. These advised that soldiers who were active during the day should drink between 8 and 11 L/day (7). Since inactive humans usually need about 2-3 L/day to remain in fluid balance, this would allow an extra 5-8 L for daily activity. Given an 8-hour working day, this recommendation would result in a maximum of about 1 L/hr during physical activity.
Interestingly, Douglas Lee commented from his own experience that:
Many experienced tropical dwellers, on the other hand, feel better able to cope with the situation if they delay replenishment for an hour or two after activity in the heat is commenced. Subjects compelled by the author to maintain body weight in hot room studies by water or saline drinking complained of discomfort and sometimes vomited. There is some evidence that man can learn to adjust to relative dehydration of the order of 2-5% of his normal body weight with the degree of functional disturbance that accompanies his first experience. (7, p. 564-565)
This was an early warning that it might be possible to drink fluid at faster rates than the small intestine is able to absorb. As a result, unabsorbed fluid will accumulate in the small bowel, leading to vomiting. No one ever considered this possibility. Instead, accepting the unproven USARIEM Water as a Tactical Weapon Doctrine, the ACSM would subsequently promote just such high rates of fluid intake during exercise. And vomiting would be the least of the problems it would cause.
In 1975, the first ACSM Position Statement on the prevention of heat injuries during distance running (8), written by David Costill, was released. His advice was that athletes “should be encouraged to frequently ingest fluids during exercise.” Importantly, there were no mentions of rates of fluid intake or threats that if such rates were not equalled, there would be dire health consequences, especially heatstroke.
In 1982, an event happened that breached the conduct of normal science. This occurred when Roger Hubbard, Ph.D., plucked the Water as a Tactical Weapon Doctrine (9) seemingly out of thin air. The sole “evidence” he could have had to develop this hypothesis at the time would have been the studies by Wyndham and Nic Strydom (10), and those of Costill et al. (11) and Carl Gisolfi and J.R. Copping (12). Yet, as I detailed in a previous column, none of those studies could possibly be used as evidence that fluid ingestion during exercise could, as he claimed, ensure that soldiers “in battle during hot weather operations” could “operate at optimal efficiency yet remain free from the serious consequences of dehydration and heat illness” (9).
But Hubbard’s persuasive powers (and the desires of other USARIEM scientists to believe him) were such that within a short time, the U.S. military revised the drinking guidelines it had used successfully for perhaps at least a century. As of 1988 (13, 14), it introduced radical change to its historic drinking guidelines. The new guidelines advised that military personnel who are active in extreme environmental conditions follow an exercise-rest ratio of 20 minutes of exercise to 40 minutes of rest and drink at a rate of 1.9 L/hr.
This is a classic example of what Thomas Sowell describes as The Vision of the Anointed (15): That which has worked in the field for hundreds of years and is based on the practical experiences of millions of humans (including those U.S. soldiers who fought in the First and Second World Wars and other major conflicts) is suddenly no longer valid. Instead, it must be thrown out because someone—a member of The Anointed—has a better, more radical idea that will immediately solve a non-existent problem. It is quickly forgotten that there is absolutely no scientific basis for this hypothesis.
When the hypothesis finally was tested (16), the data absolutely failed, as I showed in a previous column, to support it. Yet the data was interpreted as if it had. The Anointed are very good at ensuring that ugly facts do not ever prevent the adoption of their favorite theories.
So with the support of USARIEM, the way was open for this new drinking theory to become the global norm.
In Figure 1, I suggest that when the Water as a Tactical Weapon Doctrine was accepted as the definitive truth by USARIEM and the U.S. military, it signaled the end of “normal” science. From that moment on, scientists researching the role of fluid ingestion during exercise became categorized as either believers or heathens (an early example of identity politics entering science). Heathens who wished to do what we are meant to do as scientists — conduct experiments that might disprove accepted dogmas like the Water as a Tactical Weapon Doctrine or the Zero-Percent Dehydration Doctrine — were exiled and labeled as renegade, maverick, or controversial; terms which, of course, exactly describe how good scientists should be identified.
But as we are beginning to learn, when commerce becomes involved in science, the rules of proper scientific conduct soon change.
The influence of this new USARIEM dogma was apparent in the anonymously authored ACSM Position Stand on the prevention of thermal injuries during distance running (17), which, for the first time, prescribed specific goals for the amount of fluid that needed to be consumed during exercise.
The experts now had concluded that it was no longer safe or appropriate for humans to use natural signals such as thirst — a signal based on hugely complex biological pathways that have evolved over millions and millions of years—to direct our behaviors. As of 1987, only the experts knew how much we should drink during exercise.
The experts’ ideas spread rapidly. In 1996, the ACSM produced the Zero-Percent Dehydration Doctrine, which advised athletes to replace all their weight losses during exercise or “drink as much as tolerable.” No one warned that when drinking “as much as tolerable,” some athletes, especially recreational female marathon runners/joggers taking more than five hours to complete their 26-mile marathons, might be able to “tolerate” unsafe levels of fluid consumption during exercise. We had established the dangers of this practice already in 1991 (18-21); yet our evidence was simply ignored.
But for Robert Murray, Ph.D., and the GSSI, these guidelines were a commercial gift from heaven. Under Murray’s leadership, the GSSI soon began to trumpet this advice, quoting directly from the 1996 ACSM Position Stand:
During exercise, athletes should start drinking at regular intervals in an attempt to consume fluids at rates sufficient to replace all the water lost through sweating or consume the maximal amount that can be tolerated. (22, p. 250)
Interestingly, Murray cites the study by Drs. Scott Montain and Edward Coyle (23), which the GSSI had funded (under his direction), as the definitive evidence supporting the 1996 ACSM Position Stand.
By 2000, NATA (24), the American Dietetic Association (ADA), and the Dietitians of Canada (DCA) (25) were all parroting the same ideas and encouraging athletes to drink between 0.4 and 1.8 L/hr during all forms of exercise. The ADA and DCA Position Stand was conveniently released as a joint statement with the ACSM and published in the ACSM’s official journal, Medicine and Science in Sports and Exercise.
Murray and the GSSI could be well pleased that they had achieved a global monopoly on the advice athletes around the world would receive regarding their fluid requirements during exercise, advice that would favor the use of sports drinks over all else. Meanwhile, the opinions of Gatorade skeptics like myself had been well and truly silenced.
But there were already signs of trouble brewing. Ironically, the first official organization to recognize the danger, other than ourselves (18, 19), would be the very group that had initiated this slide into non-science: USARIEM and those of its scientists who had inherited the Water as a Tactical Weapon Doctrine.
In 1998, the U.S. military detected a rising incidence of exercise-associated hyponatremia (EAH) (26, Figure 2) and correctly concluded that it was the result of the advice in the 1988 guidelines promoting forced overdrinking. Accordingly (and bravely and correctly), it revised its guidelines to limit fluid intake to 0.9 L/hr and less than 11.4 L/24 hours (13, 14).
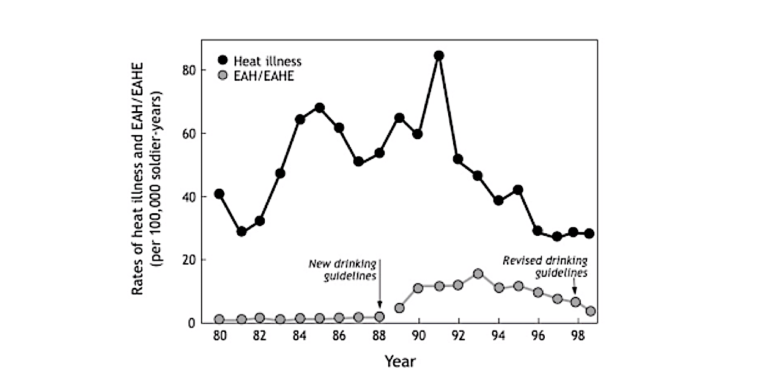
Figure 2: The rate of cases of “heat illness” and EAH/EAHE admitted to U.S. military hospitals between 1980 and 1999. Note that the rate of admissions for EAH/EAHE began to rise in 1989 following the adoption of new drinking guidelines based on the Water as a Tactical Weapon Doctrine in 1988. The rate of admissions for EAH/EAHE peaked in 1993 but in 1999 was still elevated above the 1988 rate. This trend would continue until the present. By 2016, the U.S. military acknowledged that there had been 1,519 cases of EAH in its soldiers between 2001 and 2016, with 85 in 2016 alone (27). Revised drinking guidelines would be introduced to the U.S. military in April 1988. The rate of admissions for “heat illness” was unaffected by the introduction of the new drinking guidelines in 1988 and was lowest after the adoption of the revised drinking guidelines in 1999. These guidelines advised drinking at lower rates. The spike in cases of “heat illness” in 1992 was a result of the first Iraq War.
I discovered that USARIEM was becoming concerned about the consequences of its advice that same year in a most unusual way.
In 1997, I had spoken at a conference in Nottingham, U.K., and had presented my argument that dehydration is not a disease, that it has minimal effects on athletic performance, and that, in contrast, drinking to excess is dangerous because it can produce fatal EAHE.
In the Q&A period after my lecture, Michael Sawka, Ph.D., from USARIEM (who was also a key author of the 1996 ACSM Position Stand on exercise and fluid replacement (28) that promoted the Zero-Percent Dehydration Doctrine) thoroughly reprimanded me for my arguments. My lecture had clearly not impressed him and he was not shy to warn the audience that there was no science supporting my opinions.
Less than a year later, we both attended a conference in France, funded and organized, as I recall, by one of the bottlers of mineral waters. There, I gave a lecture essentially similar to the one I had delivered in Nottingham. Although Sawka was again in the audience, this time he made no comments at the conclusion of my talk.
In the lunch break immediately after my talk, I went out for a run. I crossed paths with Sawka, who was also out running. He stopped me and complimented me on my “great” talk.
Naturally, I was taken aback by this surprising change in his opinion. I asked what had interested him in the talk (when one year before he had been contemptuous of the same information).
His answer was that in the time since USARIEM had introduced its new drinking guidelines to the U.S. military in 1988, there had been an immediate increase in the number of soldiers hospitalized for EAH/EAHE (Figure 2). This was not immediately appreciated, however.
Then, in one month alone (July 1997), five trainees in Fort Benning, Georgia, were hospitalized with EAHE, one with a fatal outcome. Eleven more cases of EAHE at Fort Benning in the previous 12 months then were reviewed (13). It was clear that the cause was forced overdrinking; the result of sticking too rigidly to the novel U.S. military drinking guidelines. Thus, Sawka and his colleagues wrote:
The U.S. Army’s fluid replacement guidelines emphasize fluid replacement during hot weather training to prevent degradation of performance and minimize the risk of heat injury. Little consideration has been given, however, to possible overhydration and development of water intoxication. Sufficient epidemiological evidence is available to demonstrate an increasing incidence of water intoxication during military training. (13)
Even though Sawka finally acknowledged that I had correctly discovered the cause of EAH/EAHE, we never really became close friends. Our differences were well captured in an excellent exchange of ideas we had in 2007 (29).
What I found so difficult to understand about Sawka’s position was that, while he would encourage the U.S. military to change its drinking guidelines because they were the direct cause of an outbreak of EAH/EAHE in the military, he remained silent on the issue that the 1996 ACSM Position Stand on exercise and fluid replacement (28) also promoted forced overdrinking among non-military exercisers.
Surely he must at some time have realized that the 1996 ACSM Position Stand must produce exactly the same outcomes among the general public as the USARIEM-directed guidelines had caused in the military.
The Return of Normal Science
The cause of the outbreak of EAH/EAHE in the U.S. military could not be ignored forever, but it would still be some years before the dangers of the forced overdrinking policy promoted by the 1996 ACSM Position Stand on exercise and fluid replacement (28) would be admitted.
Change would be driven largely by the result of a single tragedy: the death of Cynthia Lucero in the 2002 Boston Marathon. Her entirely avoidable death finally would force reality to strike. The consequences of her tragic and unnecessary death are fully described in Waterlogged (4), and I will return to discuss this in a future column.
The key point is that because she died of unnatural causes, an autopsy had to be performed. As reported in the Boston Globe, the autopsy concluded that she died because she had drunk too much fluid (30), including, according to her friends, too much Gatorade (31). No longer could a developing truth be hidden from public scrutiny.
One outcome was that in 2002, I was invited by the International Marathon Medical Directors Association (IMMDA) to develop new drinking guidelines for competitors in marathon races under its jurisdiction, based on my experience and understanding of the biology of EAH and post-exercise collapse. These were first published in 2003 (32) and updated in 2006 (33). The key points I developed in the original guidelines were as follows:
- Dehydration does not cause heatstroke.
- Heatstroke is not prevented by fluid ingestion during exercise.
- Athletes should be encouraged to drink to thirst during exercise.
- The majority of athletes who collapse after prolonged exercise do so because they develop exercise-associated postural hypotension (EAPH) (34), a benign condition that is treated quite simply by having the athlete lie down with his or her legs elevated above the level of the heart (35, 36).
- In contrast, athletes who collapse before the finish of a race have significant, sometimes life-threatening conditions and require expert medical attention. The two most common causes in persons without pre-existing medical conditions are EAH/EAHE and heatstroke.
Since the message about the cause of EAH and EAHE still was not being taken sufficiently seriously, in 2005 we organized the 1st International Exercise-Associated Hyponatremia Consensus Development Conference in Cape Town, South Africa. The conclusions of the conference were published in 2006 (37). The consensus was that all the evidence that had accumulated since our original work (18, 19) confirmed our original conclusion that forced overdrinking is the single most important factor causing EAH and EAHE.
An important outcome of the 1st Conference was that a number of the participants were able to pool their data from studies in which changes in body weight and blood sodium concentrations in competitors in marathons and longer events had been studied (38). The combined data identified the three biological changes necessary to cause EAH and EAHE, further confirming that our ideas were correct—and that the Zero-Percent Dehydration Doctrine was the ultimate cause.
The ACSM 2007 Position Stand on Exercise and Fluid Replacement
Faced with this incontrovertible evidence, the ACSM issued its revised 2007 Position Stand on Exercise and Fluid Replacement (39). All six authors of the revised guidelines had very strong and “cozy” relationships with Gatorade (2); four received research funding from the GSSI; the fifth, Dr. Randy Eichner, could best be described as a traveling medical spokesperson for Gatorade and the GSSI; and the sixth, Sawka, was employed by USARIEM, the organization that had created the Zero-Percent Dehydration Doctrine. Since the U.S. military is one of the biggest consumers of Gatorade, it seems highly improbable that the work of USARIEM is completely free of any influence from either Gatorade or the GSSI.
These guidelines continue to promote the false Science of Hydration.
They promote the need to pre-hydrate at least “several hours before the activity to enable fluid absorption and allow urine output to return to normal levels.” There is zero evidence that this recommendation is necessary, helpful, desirable, or even safe.
The guidelines also propose, “The goal of drinking during exercise is to prevent excessive (>2% body weight loss from water deficit) dehydration and excessive changes in electrolyte balance to avert compromised performance.” Again, there is zero evidence that a loss of >2% of body weight compromises performance. Instead, the authors should explain to athletes that weight loss during exercise is normally distributed (as we showed in Figure 3 in a previous column (40)) and the athletes who win marathons and longer races are usually the most “dehydrated” (4).
Next, the guidelines suggest, “Because there is considerable variability in sweating rates and sweat electrolyte content between individuals, customized fluid replacement programs are recommended. Individual sweat rates can be estimated by measuring body weight before and after exercise.” Again, this advice has never ever been tested in a controlled trial. There is absolutely no evidence that this is necessary. Instead, the evidence suggests that athletes will optimize their health and performance during exercise provided they drink only to thirst (41).
The guidelines continue with the statement, “During exercise, consuming beverages containing electrolytes and carbohydrates can provide benefits over water alone under certain circumstances.” While there may be some evidence that glucose-containing beverages may have some benefits—as well as some harms, accelerated tooth decay being the obvious (42, 43)—the evidence that there is any benefit to ingesting electrolytes during exercise is slim. There is zero evidence that electrolyte ingestion plays any part in the prevention of EAH and EAHE, a point to which we will return in great detail in future columns.
Finally, they propose, “After exercise, the goal is to replace any fluid electrolyte deficit. The speed with which rehydration is needed and the magnitude of fluid electrolyte deficits will determine if an aggressive replacement program is merited.” Again, there is zero evidence that this is necessary or desirable. It has simply not been studied appropriately.
Once again, the needs of the sports drink industry to oversell its product won over the scientific requirement to present facts that are evidence-based (44, 45).
But that is what happens, as we have seen repeatedly, when Position Stands are written by those who enjoy the largesse of the very industries that stand to benefit the most from industry-favorable guidelines.
The next columns will detail how we proved that EAH and EAHE are indeed caused by forced overdrinking in persons who followed the experts’ drinking guidelines to the letter.
We will also show how industry tried further to confuse the public by developing alternate explanations for these conditions, such as the “salty-sweater” myth and the myth that sodium deficiency treated by ingesting a sports drink during exercise can prevent EAH and EAHE.
Additional Reading
- The Hyponatremia of Exercise, Part 1
- The Hyponatremia of Exercise, Part 2
- The Hyponatremia of Exercise, Part 3
- The Hyponatremia of Exercise, Part 4
- The Hyponatremia of Exercise, Part 5
- The Hyponatremia of Exercise, Part 6
- The Hyponatremia of Exercise, Part 8
- The Hyponatremia of Exercise, Part 9
- The Hyponatremia of Exercise, Part 10
- The Hyponatremia of Exercise, Part 11
- The Hyponatremia of Exercise, Part 12
Professor T.D. Noakes (OMS, MBChB, MD, D.Sc., Ph.D.[hc], FACSM, [hon] FFSEM UK, [hon] FFSEM Ire) studied at the University of Cape Town (UCT), obtaining a MBChB degree and an MD and DSc (Med) in Exercise Science. He is now an Emeritus Professor at UCT, following his retirement from the Research Unit of Exercise Science and Sports Medicine. In 1995, he was a co-founder of the now-prestigious Sports Science Institute of South Africa (SSISA). He has been rated an A1 scientist by the National Research Foundation of SA (NRF) for a second five-year term. In 2008, he received the Order of Mapungubwe, Silver, from the President of South Africa for his “excellent contribution in the field of sports and the science of physical exercise.”
Noakes has published more than 750 scientific books and articles. He has been cited more than 16,000 times in scientific literature and has an H-index of 71. He has won numerous awards over the years and made himself available on many editorial boards. He has authored many books, including Lore of Running (4th Edition), considered to be the “bible” for runners; his autobiography, Challenging Beliefs: Memoirs of a Career; Waterlogged: The Serious Problem of Overhydration in Endurance Sports (in 2012); and The Real Meal Revolution (in 2013).
Following the publication of the best-selling The Real Meal Revolution, he founded The Noakes Foundation, the focus of which is to support high quality research of the low-carbohydrate, high-fat diet, especially for those with insulin resistance.
He is highly acclaimed in his field and, at age 67, still is physically active, taking part in races up to 21 km as well as regular CrossFit training.
REFERENCES
- Berryman JW. 50 Years of progress and service, 1954-2004. Med. Sci. Sports Exerc. Special Edition, 1-9.
- Cohen D. The truth about sports drinks. Br. Med. J. 345(2012).
- Le Fanu J. The Rise and Fall of Modern Medicine. New York, NY: Basic Books, 2012.
- Noakes TD. Waterlogged: The serious problem of overhydration in endurance sports. Champaign, IL: Human Kinetics, 2012.
- Wyndham CH. Heatstroke and hyperthermia in marathon runners. Annals N.Y. Acad. Sci. 301(1977).
- Noakes TD. The Hyponatremia of Exercise, Part 2. CrossFit.com. 11 March 2019. Available here.
- Lee DHK. Terrestrial animals in dry heat: Man in the desert. In Handbook of Physiology: Adaptation to the Environment. Dill DB, Adolph EF, and Wilber CG Eds. Washington, D.C.: American Physiological Society, 1964, pp. 551-582.
- American College of Sports Medicine. The American College of Sports Medicine Position Statement on Prevention of Heat Injuries During Distance Running. Med. Sci. Sports 7(1975): VII-VIX.
- Hubbard RW, Mager M, Kerstein M. Water as a tactical weapon: A doctrine for preventing heat casualties. Defense Technical Information Center OAI-PMH Repository 1982, pp. 1-19.
- Wyndham CH, Strydom NB. The danger of an inadequate water intake during marathon running. S. Afr. Med. J. 43(1969): 893-896.
- Costill DL, Kammer WF, and Fisher A. Fluid ingestion during distance running. Arch. Environ. Health 21(1970): 520-525.
- Gisolfi CV, and Copping JR. Thermal effects of prolonged treadmill exercise in the heat. Med. Sci. Sports 6(1974): 108-113.
- Montain SJ, Latzka WA, Sawka MN. Fluid replacement recommendations for training in hot weather. Mil. Med. 164(1999): 502-508.
- Kolka MA, Latzka WA, Montain SJ, et al. Effectiveness of revised fluid replacement guidelines for military training in hot weather. Aviat. Space Environ. Med. 74(2003): 242-246.
- Sowell, T. The Vision of the Anointed: Self-Congratulation as a Basis for Social Policy. New York, NY: Basic Books, 1996.
- Kerstein M, Mager M, Hubbard R, et al. Heat-related problems in the desert: The environment can be an enemy. Mil. Med. 149, (1984): 650-656.
- American College of Sports Medicine. Position Stand on the Prevention of Thermal Injuries During Distance Running. Med. Sci. Sports Exerc. 19(1987): 529-533.
- Noakes TD, Goodwin N, Rayner BL, et al. Water intoxication: A possible complication during endurance exercise. Med. Sci. Sports Exerc. 17(1985): 370-375.
- Irving RA, Noakes TD, Buck R, et al. Evaluation of renal function and fluid homeostasis during recovery from exercise-induced hyponatremia. J. Appl. Physiol. 70(1991): 342-348.
- Noakes TD. The hyponatremia of exercise. Int. J. Sports Med. 2, (1992): 205-208.
- Noakes TD. Fluid replacement during exercise. Exerc. Sports Sci. Rev. 21(1993): 297-330.
- Murray RJ. Dehydration, hyperthermia, and athletes: Science and practice. J. Athl. Train. 31(1996): 248-252.
- Montain SJ, and Coyle EF. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J. Appl. Physiol. 73(1992): 1340-1350.
- Casa DJ, Armstrong LE, and Hillman SK. National Athletic Trainers Association Position Statement. Fluid replacement for athletes. J. Athl. Train. 35(2000): 212-224.
- American College of Sports Medicine, American Dietetic Association, Dietitians of Canada. Joint Position Statement: Nutrition and athletic performance. Med. Sci. Sports Exerc. 32(2000): 2130-2145.
- Montain SJ, Latzka WA, Hoyt RW, et al. Sustaining hydration in hot weather. RTO-MP-076 25(2002): 1-8.
- Anonymous. Update: Exertional Hyponatremia. U.S. Armed Forces 2001-2016. Health Mil. Available here.
- Convertino VA, Armstrong LE, Coyle EF, et al. American College of Sports Medicine Position Stand: Exercise and fluid replacement. Med. Sci. Sports Exerc. 28(1996): i-vii.
- Sawka MN, and Noakes TD. Does dehydration impair exercise performance? Med. Sci. Sports Exerc. 39(2007): 1209-1217.
- Smith S. Marathon runner’s death linked to excessive fluid intake. Boston Globe. 13 August 2002.
- Associated Press. Runner dies due to too much fluid. Deseret News U.S. & World. 13 August 2002.
- Noakes TD. Fluid replacement during marathon running. Clin. J. Sport Med. 13(2003): 309-318.
- Hew-Butler T, Verbalis JG, and Noakes TD. Updated Fluid Recommendation: Position Statement From the International Marathon Medical Directors Association (IMMDA). Clin. J. Sport Med. 16(2006): 283–292.
- Holtzhausen LM, and Noakes TD. The prevalence and significance of post-exercise collapse in ultramarathon runners. Med. Sci. Sports Exerc. 27(1995): 1095-1101.
- Holtzhausen LM, and Noakes TD. Collapsed ultraendurance athlete: proposed mechanisms and an approach to management. Clin. J. Sports Med. 7(1997): 292-301.
- Asplund CA, O’Connor FG, and Noakes TD. Exercise-associated collapse: an evidence-based review and primer for clinicians. Br. J. Sports Med. 45(2011): 1157-1162.
- Hew-Butler TD, Almond CS, Ayus JC, et al. Consensus Statement of the 1st International Exercise-Associated Hyponatremia Consensus Development Conference, Cape Town, South Africa 2005. Clin. J. Sport Med. 15(2005): 208–13.
- Noakes TD, Sharwood K, Speedy D, et al. Three independent biological mechanisms cause exercise-associated hyponatremia: Evidence from 2,135 weighed competitive athletic performances. PNAS 102(2005): 18550-18555.
- Sawka MN, Burke LM, Eichner ER, et al. American College of Sports Medicine Position Stand. Exercise and fluid replacement. Med. Sci. Sports Exerc. 39(2007): 377-390.
- Noakes, TD. The hyponatremia of exercise, part 5. CrossFit.com. 6 April 2019. Available here.
- Hoffman MD, Cotter JD, Goulet ED, et al. VIEW: Is Drinking to Thirst Adequate to Appropriately Maintain Hydration Status During Prolonged Endurance Exercise? Yes. Wilderness Environ. Med. 27(2016): 192-202.
- Needleman I, Ashley P, Petrie A, et al. Oral health and impact on performance of athletes participating in the London 2012 Olympic Games: a cross-sectional study. Br. J. Sports Med. 47(2013): 1054–1058.
- Needleman I, Ashley P, Fine P, et al. Oral health and elite sport performance. Br. J. Sports Med. 49(2015): 3–6.
- Noakes TD, and Speedy DB. Case proven: Exercise associated hyponatraemia is due to overdrinking. So why did it take 20 years before the original evidence was accepted? Br. J. Sports Med. 40(2006), 567–572.
- Noakes TD, and Speedy DB. Lobbyists for the sports drink industry: an example of the rise of ‘‘contrarianism’’ in modern scientific debate. Br. J. Sports Med. 41(2007): 107-109.
Comments on The Hyponatremia of Exercise, Part 7
These article about hyponatremia of exercise are somewhat disturbing to me. It makes me want to go double check all the recommandation that we receive. And it is a good thing because we should understand by now that it is our own responsibility to go get the truth and to stay up to date with it.
I find it interesting that we would allow the abandonment of biological thirst for a water-intake prescription. Humans just keep letting themselves be outsmarted under the guise of science but for the benefit of commerce.
Too true, Katina. The longer I have been in medicine and in science, the more disturbed I have become by the prevailing attitude in health care. The primary desired professional outcome seems to be a beneficial financial outcome. In this series I have tried to show how the sports drink industry is a prime example of this approach.
The Hyponatremia of Exercise, Part 7
3