This 2015 review summarizes multiple mechanisms by which statins may increase heart disease and heart failure risk.
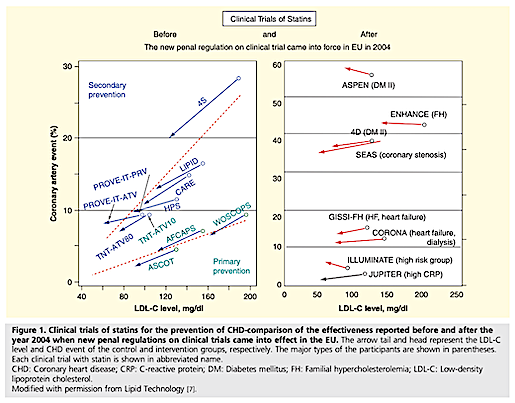
First, the authors argue the most trustworthy existing evidence does not show that statin-induced reductions in LDL cholesterol decrease heart disease risk. The widespread belief that statins reduce heart disease event rates is primarily based on studies and meta-analyses of studies performed in the 1990s. More recent trials, specifically those published after clinical trial regulations were increased in the EU (2004), have consistently failed to show that statins significantly reduce CHD risk, despite consistently reducing LDL cholesterol levels (Figure 1).
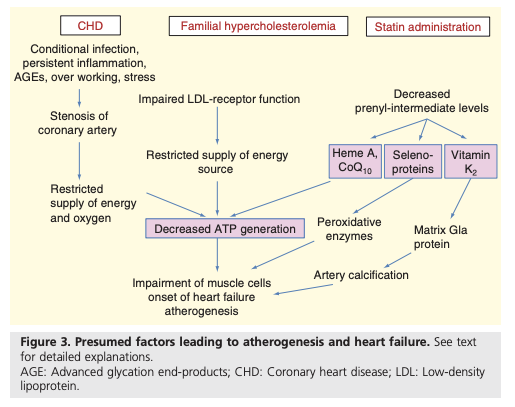
The authors argue statins may increase heart disease and heart failure risk through multiple mechanisms (Figure 3). Statins, by inhibiting cholesterol biosynthetic pathways, inhibit the synthesis of coenzyme Q10 (CoQ10) and heme A, both critical components of the electron transport chain. As a result, statins may impair mitochondrial function and reduce ATP generation (1).
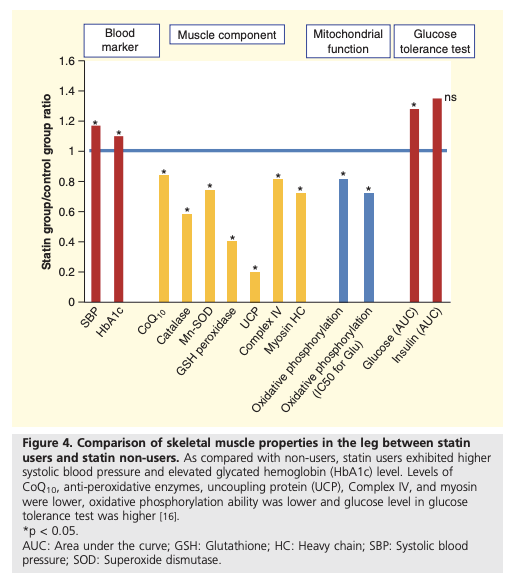
This may explain multiple abnormalities in muscular and mitochondrial function observed in statin users, including reduced mitochondrial oxidative capacity, as is summarized in Figure 4.
Statins have also been shown to inhibit synthesis of selenoproteins. Selenoproteins reduce peroxidative stress. Statin use may increase levels of this stress and thus induce cardiomyopathy, similar to that known to occur due to selenium deficiency.
Additionally, statins inhibit synthesis of vitamin K2 (VK2), which participates in reactions that prevent blood vessel calcification. This inhibition provides a potential explanation for trials showing accelerated coronary artery calcification when comparing high-frequency to low-frequency statin use among diabetics.
Finally, statins may increase the risk of heart failure. Muscle weakness and pain are well-recognized statin side effects, and these detrimental effects may extend to heart muscle. Two trials found diastolic dysfunction and/or evidence of congestive heart failure to be common in patients taking statins; in one of the two trials, statin discontinuation alongside CoQ10 supplementation improved heart muscle function. The authors note statin-induced cardiomyopathy may be an underreported issue, as the requisite mitochondrial damage may take years to develop and so may not be clearly linked to statin introduction.
In sum, the authors argue statins may increase risk of atherosclerosis by increasing artery calcification, and heart failure by inducing mitochondrial dysfunction and ATP insufficiency. In light of more recent trials that bring into question whether statins reduce CHD risk (despite lowering cholesterol levels), the authors suggest statins may increase overall mortality and morbidity.
Notes
- This may be similar to familial hypercholesterolemia (FH). While FH is often characterized as a condition of excess blood cholesterol, it is directly caused by a deficiency in LDL receptor availability or function. In other words, while blood cholesterol levels are high in FH, cells are unable to take up cholesterol, which could lead to ATP deficiency through similar mechanisms.