Type 2 diabetes is generally thought to be chronic and progressive, marked by an inevitable decline in beta cell function and increase in plasma glucose levels. Current pharmaceutical treatments are fundamentally unable to alter the course of the disease. Bariatric surgery has been shown to rapidly normalize glucose levels, even prior to weight loss. This study tested whether severe caloric restriction — similar to that seen alongside bariatric surgery — could lead to similar glycemic benefits. The study results indicated a very low-calorie diet rapidly improves liver insulin sensitivity and gradually improves pancreatic function in the process reversing Type 2 diabetes.
During the study, 11 diabetics were fed a 600-calorie-per-day diet (VLCD), most of which came from Optifast shakes and the remainder of which came from vegetables. All subjects were overweight or obese and had been diabetic for four years or less. Nine controls were selected, matched for age, sex, and weight.
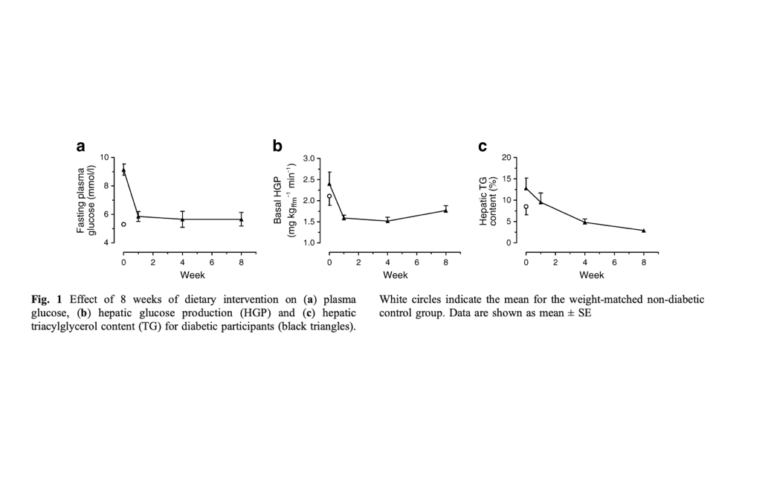
Within the first week on a VLCD, fasting glucose levels had normalized (from 9.2 to 5.9 mmol), as had fasting insulin levels (151 to 73 units). Hepatic insulin sensitivity (as measured by the extent to which glucose production is suppressed by insulin) was improved to a level better than controls, and hepatic glucose production decreased. These changes occurred alongside a 30% reduction in liver fat (from 12.8% to 8.5% of weight) within the first week. By week eight, liver fat was down 70% and similar to that of healthy-weight, nondiabetic controls.
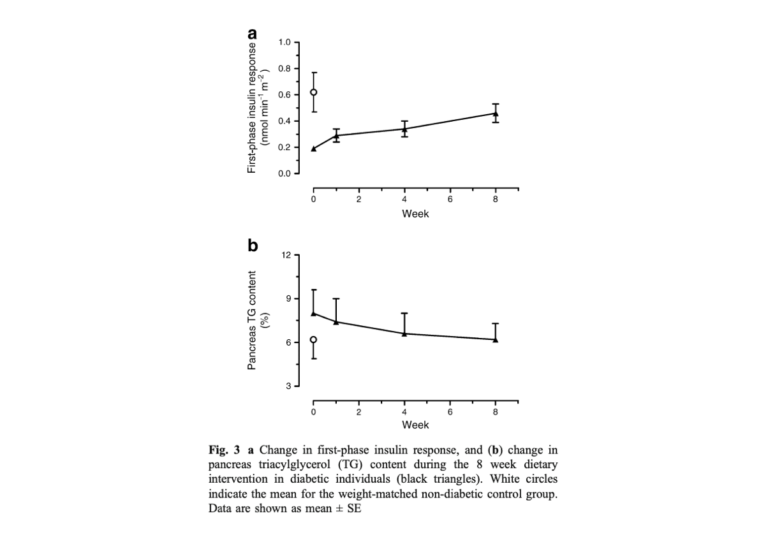
Pancreatic function improved more gradually. Pancreatic fat content decreased to match controls by the eighth week, and first-phase insulin response (i.e., the insulin dose produced in immediate response to a glucose load) increased similarly.
Notably, peripheral glucose disposal — i.e., the rate at which the muscles and other tissues cleared glucose from the blood, a measure correlated with peripheral insulin sensitivity — did not change significantly over the eight-week period.
Subjects’ mean plasma triglyceride, total cholesterol, and LDL cholesterol levels dropped, while HDL cholesterol levels remained steady.
Taken together, these results indicate:
- Diabetes is not necessarily a chronic, irreversible diseases. As has been shown with bariatric surgery and now with diet, diabetes can be reversed at a whole-body and an organ-specific level through a targeted, intensive intervention.
- Deterioration in liver and pancreas function were closely linked to increased fat content in those organs; as fat was cleared, function was restored. While this does not directly implicate fat as causal, it suggests organ fat accumulation may play an important role in diabetes progression.
- Dietary restriction improves glycemic control by driving improvements in the liver and pancreas, not muscle and fat (i.e., peripheral) tissue. Given the documented benefits of exercise on peripheral insulin sensitivity (outlined elsewhere on CrossFit.com), this suggests dietary interventions and exercise have complementary roles in controlling and reversing diabetes.
Note this is one of multiple studies indicating the benefits of gastric bypass surgery for diabetics can be explained, at least in large part, by the caloric restriction associated with the surgery rather than the surgery itself (1).
Notes
- Very low-calorie diet mimics the early beneficial effect of roux-en-Y gastric bypass on insulin sensitivity and β-cell function in Type 2 diabetic patients, The importance of caloric restriction in the early improvements in insulin sensitivity after roux-en-Y gastric bypass surgery, Calorie restriction is a major determinant of the short‐term metabolic effects of gastric bypass surgery in obese Type 2 diabetic patients, Rapid improvement in diabetes after gastric bypass surgery
Reversal of Type 2 Diabetes: Normalisation of Beta Cell Function in Association With Decreased Pancreas and Liver Triacylglycerol