In this 2019 review, Thomas Seyfried et al. assess the potential of ketogenic metabolic therapy (KMT) to challenge or supplant the current standard of care (SOC) for glioblastoma multiforme (GBM). In keeping with evidence presented in his previous work, Seyfried advocates for KMT as a viable approach because of its potential effectiveness and the ineffectiveness of the current SOC.
GBM SOC treatment generally involves surgical resection of the tumor and radiotherapy alongside temozolomide and dexamethasone. This treatment causes damage to healthy brain cells, which, through multiple mechanisms, may increase tumor growth, resistance to future therapies, and tumor invasiveness. Figure 4 summarizes these arguments. Seyfried notes median life expectancy following a GBM diagnosis has not changed from estimates a century ago.

Figure 4
Ketogenic metabolic therapy (KMT) consists primarily of following a calorie-restricted ketogenic diet to simultaneously lower blood glucose levels and elevate ketone bodies. Ketone bodies cannot be used as fuel by GBM cells, and so this state leads to specific cancer cell death without harming healthy cells. Preclinical mouse data (shown in Figure 5) demonstrated reduced tumor invasiveness while also leading to clearer tumor margins (which should improve the effectiveness of surgical resection). These effects may be further enhanced by co-therapies including hyperbaric oxygen and period glutamine suppression.
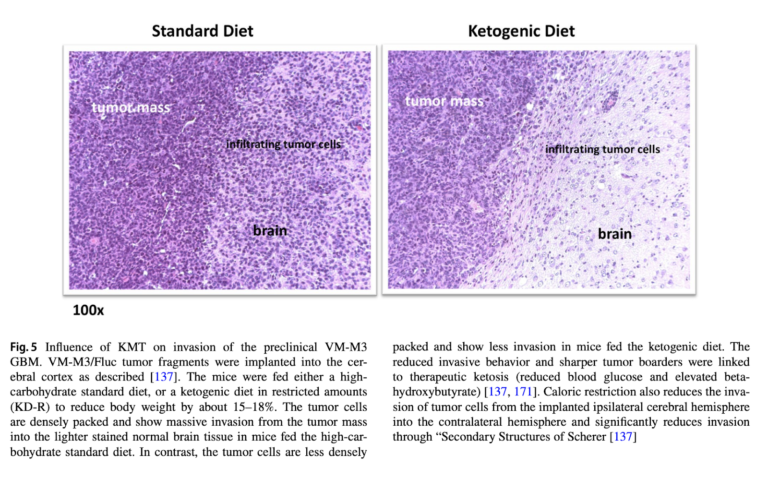
Figure 5
KMT, particularly when delivered as part of a “press-pulse” therapeutic strategy, is designed to specifically deprive cancer cells of energy without harming normal cells. Preliminary anecdotal evidence suggests a KMT in the absence of standard-of-care treatment may be able to extend lifespan (including the case of a single long-term survivor). The authors suggest future research comparing SOC to SOC + KMT and KMT alone would begin to substantiate KMT’s therapeutic value.