The publication of the Hubbard-inspired USARIEM paper “Water as a Tactical Weapon” (1) establishes that by the early 1980s, the U.S. military was convinced that Cyril Wyndham and Nic Strydom’s idea that dehydration causes heatstroke—which can be prevented by copious fluid ingestion during exercise as a result of drinking “ahead of thirst”—was proven fact. With the support of USARIEM, it would not take much for this belief to spread rapidly around the world. The Gatorade Sports Science Institute (GSSI) soon would be formed to drive the marketing of the Gatorade brand and the global acceptance of this “truth.”
Thereafter, a number of important events happened in quick succession.
In 1983, Quaker Oats bought the Gatorade brand for US$220 million. The clear intent of the new owners was to make Gatorade the global leader in sports drinks.
In 1985, Gatorade began to fund the National Athletic Trainers Association (NATA).
Later that same year, Quaker Oats opened the GSSI in Barrington, Illinois, and installed Dr. Bob Murray, Ph.D., as its founding director. He soon became an aspirational figure in the sports sciences. He served until July 2008, when he was removed as PepsiCo, the new owners of the Gatorade brand, began to grapple with falling Gatorade sales.
In 1987, the U.S. military introduced new drinking guidelines (2, 3), updating those that had been in use since at least World War II. These new guidelines mandated that soldiers must drink up to 1.8 L/hr whenever they exercised in temperatures in excess of 30 degrees Celsius. The guidelines clearly were based on the unproven assumptions promoted by the 1984 Water as a Tactical Weapon Doctrine (4).
In the same year, the American College of Sports Medicine (ACSM) produced its second Position Stand on the Prevention of Thermal Injuries During Distance Running (5). For the first time, these guidelines promoted specific rates of fluid ingestion during exercise, in keeping with the Water as a Tactical Weapon Doctrine. Since the guidelines promoted overdrinking during exercise, they set the scene for a global tragedy that was already developing even as the guidelines were adopted.
In 1988, the first of 12 Quaker Oats-funded closed scientific conferences held in exotic locations around the world kicked off in Bermuda. Attendance was by invitation only. An invitation to these conferences soon became a status symbol among exercise scientists.
In 1990, Gatorade signed NBA Chicago Bulls superstar Michael Jordan to a $13.5-million contract. This denied Coca-Cola the option to have Jordan endorse its new sports drink, Powerade. The contract was so successful that it lasted until 2007.
In 1992, Gatorade announced a $250,000 gift to the ACSM, an organization that it described as “the premier organization in sports medicine and exercise science.”
In 1992, Drs. Scott Montain and Edward Coyle published a Gatorade-funded study (6), to be described in a future column. This study was used to justify the 1996 ACSM Position Stand On Exercise and Fluid Replacement (7).
In 1996, the ACSM updated its 1987 Position Stand with the publication of two companion Position Stands: On Exercise and Fluid Replacement (7) and On Heat and Cold Illnesses During Distance Running (8). The Position Stand on Exercise and Fluid Replacement advised all athletes, regardless of ability, the intensity at which they exercise, or the duration for which they exercise, to drink up to 1.2 L/hr during any and all forms of exercise. This Position Stand introduced another novel biological “truth,” which I have termed the Zero-Percent Dehydration Doctrine, to be discussed in a subsequent post in this series.
The damage that these Position Stands eventually caused was already predictable, even as they were promulgated.
The 1987 ACSM Position Stand on the Prevention of Thermal Injuries During Distance Running
In 1987, the ACSM updated its drinking guidelines for exercise under the new heading, “ACSM Position Stand on the Prevention of Thermal Injuries During Distance Running” (5). The document included, for the first time, what USARIEM already had turned into a scientific certainty based on the flawed study by Dr. Morris Kerstein and colleagues (4): that fluid ingestion during exercise can prevent all forms of heat illness. Thus, it stated, “Fluid consumption before and during the race will reduce the risk of heat injury, particularly in longer runs such as the marathon.”
The two key references supporting this new scientific certainty were the articles by Wyndham and Strydom (9), and Gisolfi and Copping (10), neither of which actually supported this conclusion. None of those authors could possibly draw that conclusion, since none had studied whether fluid ingestion during marathon running can prevent heat illness.
For the moment, let’s ignore the clear evidence that heatstroke occurs infrequently in marathon runners but is much more common in elite runners racing distances from 5 to 12 kilometers (11), usually in hot, humid conditions in which the runners’ metabolic rates and hence rates of heat production are much greater than in marathon runners who typically run more slowly. We remember, also, that races of 5 to 12 kilometers take tens of minutes rather than hours to complete, so it is not possible for athletes in these races to become “dangerously dehydrated.” Accordingly, if athletes are developing heatstroke and other heat illnesses in races of these distances, dehydration clearly cannot be the cause.
And let’s remember that the only measurements any of these authors performed pertained to the effect ingesting or avoiding fluid has on body temperature during exercise lasting between 90 and 150 minutes. Importantly, no athlete in any study developed any form of heat illness, regardless of whether they ingested fluids. Since no one in the control group of non-drinkers developed heat illness, the intervention of drinking fluids never could “prove” that fluid ingestion prevents heat illness. Surely, that is common sense.
We also must remember that the temperature-lowering effect of fluid ingestion only occurred after 60 minutes of exercise. Nor should we forget that the higher body temperatures in mammals who do not ingest fluid when living in the desert with limited access to water is likely an example of an advantageous mammalian biological response known as adaptive heterothermy (12) (advantageous because the higher body temperature increases heat loss from the body without the need to lose additional water in the form of sweat).
The authors also claimed, “Such dehydration will subsequently reduce sweating and predispose the runner to hyperthermia, heat stroke, heat exhaustion and muscle cramps.” Once again, the paper by Wyndham and Strydom is quoted as proof for this definitive conclusion. But Wyndham and Strydom studied none of those complications, since none of the athletes they studied developed any of these conditions. Even if they had, there is still today no evidence to support any of these claims.
So how could these experts, apparently the most knowledgeable in the world, concoct such a litany of factual distortions, which I first questioned in 1988 (13) and subsequently labeled “The Dehydration Myth” (14-16)? What if they were responding to someone else’s script?
The 1987 Position Stand introduced the concept of having specific targets for drinking. Specifically, it stated, “An adequate supply of water should be available before the race and every 2-3km during the race. Runners should be encouraged to drink 100-200 mL at each station.”
Whoever drew up this advice failed to understand that not all marathon runners race at the same pace or are of the same size or gender—or are exposed to exactly the same environmental conditions during the race. An athlete running a marathon in 2:04, who drinks 200 milliliters every 2 kilometers will be drinking at a rate of 2 L/hr, whereas a 6-hour marathon runner will drink about 700 mL/hr. However, these guidelines advise that all athletes, regardless of the speed at which they run, or their size, or gender, or the environmental conditions in which they exercise, should be drinking between 0.7 and 2.0 L/hr to ensure that they do not develop “dehydration-induced heatstroke.”
Why did no one ask: What about the type of exercise; its intensity and duration; the age, gender, and body mass of the exercisers; and the environmental conditions in which the exercise is performed? Surely these factors also could influence how much exercisers need to drink? By this time, however, my colleagues and I were the only group of scientists asking these sorts of difficult questions (17-20), and the questions usually were not well received by the scientific community responsible for providing answers.
Does the Body Contain a Reserve of Fluid That Does not Need to be Replaced During Exercise in Order to Prevent Heat Illness or Enhance Performance?
Even Wyndham and Strydom, whose (absence of) data was the key pillar propping up “The Dehydration Myth,” argued that it was safe to lose up to 3% of body weight during exercise without any risk that the body temperature would be abnormally elevated. They wrote:
[U]p to a water deficit of about 3%, body temperature varied between about 101 and 102°F (38.3 – 38.9°C) but with an increase in water deficit above 3%, rectal temperature increased in proportion to the extent of the water deficit, resulting in all runners with water deficits more than 4% having had rectal temperatures above 103°F (39.4°C). (9)
[As a result:] It is clear that if the water deficit exceed[s] 3% of the man’s body-weight, then, even in cool conditions, rectal temperature rises. If the deficit exceeds 4% it may rise to excessive levels, especially if the man is heavy. [A rectal temperature of 39.4°C is of course well below values at which damage can be expected—addition mine.]
Nor were Wyndham and Strydom the first to question whether humans need to replace all the fluids they lose during exercise. E.H. Hunt, who served with the British Army prior to the First World War, wrote in 1913, “A healthy man carries in his body a large reserve of water, this reserve being mainly stored in muscle and being so readily available that the percentage of water in the blood is not appreciably diminished even when several litres of water have been lost by sweating” (21). This finding that the blood volume does not decrease in athletes even when they lose quite substantial amounts of weight when drinking ad libitum (i.e., as much as desired) during prolonged exercise has been confirmed in a number of modern studies (12-29).
During World War II, British physician W.S.S. Ladell was the first to actively research this question. On behalf of the Committee for the Care of Shipwrecked Personnel, he was tasked to “discover means of mitigating thirst, to determine the minimum water requirements of the body, and to see how these requirements could be reduced” in shipwrecked sailors. From his research he developed the concept that the human body has a “free circulating water of 2L” (30, 31).
For his studies, consenting research subjects, including Ladell himself, were placed on a restricted water intake for up to 12 days in moderate environmental conditions; in some experiments, subjects did not receive any fluid for nearly three days. The main findings were the following:
- A water intake of between 0.8 and 0.9 liters per day was required to maintain water balance.
- Urine production on this fluid intake was reduced to 0.3 to 0.5 liters per day.
- A 5% weight loss occurred over the first 24 hours in those who did not drink. This degree of weight loss was tolerable. A 10% loss over 60 hours, however, produced gross physical and mental deterioration with generalized fatigue. Even after 72 hours without water, subjects still could rally themselves to perform “an exercise-tolerance test efficiently.”
- The rate of salivation fell only on the third day without water.
- The rate of weight loss during the first 24 hours was greater than the subsequent rates of loss. More important, “Water that was given during the first 24 hours never saved body-water, but swelled the urine-volume by the amount taken.”
Ladell’s inability to find any deleterious physiological effects with weight losses of up to 2.5 liters during exercise (32) further convinced him of the presence of this 2-liter free-circulating volume of fluid that does not need to be replaced during exercise.
As a result of this finding, Ladell concluded:
There is in the body what could be called free circulating water, normally used for such things as intestinal secretions, which are only temporarily lost to the body during digestion and then reabsorbed. Until this water has been utilized it is un-economical to start taking the limited water-ration. We therefore recommend that for the first 24 hours adrift no water should be taken.
He also postulated that humans may exist normally in a state of relative fluid overload:
It may be, however, that man has evolved drinking habits by which he maintains himself in a perpetually overhydrated state; in contrast to all other terrestrial mammals, he rarely produces a highly concentrated urine and to do that he has severely to control his fluid intake. (33)
He added, “In young adults the free circulating water amounts to at least 2 L, but whether it is as much as this at all ages and in both sexes it is not possible to say” (33).
There are two possible locations of this water store. The first is a volume of water stored with glycogen, the form in which sugar is stored in muscle and liver. In 1906, Nathan Zuntz and colleagues proposed that each gram of glycogen so formed might store as much as 3 grams of water (34). Since a 70-kilogram male might store at least 600 grams of glycogen in his liver and muscles, by the time that glycogen had been burned — for example after 3 or more hours of exercise — it would have released a total of 1.8 liters (1.8 kilograms) of water. This water would be replaced only after exercise, when the athlete again begins to replenish his glycogen stores.
The most impressive support for this theory comes from a 1970 study (35) that showed athletes increased their body weights by 2.4 kilograms during a period of increased carbohydrate intake, so-called “carbohydrate-loading.” Measured total body water content increased by 2.2 liters, accounting for most of this change in body weight. These changes could be explained by an increase in body glycogen content of about 500 grams with 1,500 milliliters of associated water. The authors concluded that “a change in the muscle glycogen content of the body causes the body weight to increase significantly more than the amount of stored glycogen” so that “it may be of importance to take the glycogen content of the body into consideration when total body water is determined.”
The second obvious site for this free water storage would be within the intestines. For example, the intestinal water contents of mammals with a rumen — including camels, sheep, and African antelope like the eland — may comprise up to 12-18% of body weight (36); in the camel it is estimated that 120 g/kg of water is stored in the gut (37). In a 700-kilogram camel, water stored in the gut could therefore account for an additional 84 liters of fluid. If the same ratio applies in humans, then the intestine of a 50- to 80-kilogram human conceivably could contain 2 to 4 liters of free fluid.
Perhaps the best recent evidence for the presence of this ~2-liter volume of free water that does not require replacement comes from a more modern study by Susan Barr, et al. (38). In this study, subjects cycled for up to 6 hours when they drank either nothing or enough water or a sodium-containing drink to balance their rates of sweat loss.
This was an early study to determine whether a fall in blood sodium concentrations during exercise is caused by unreplaced sodium losses in sweat. That is why the control condition was exercise without any fluid replacement, whereas the interventions involved drinking either water or a sodium-containing drink to prevent any dehydration. The authors did not consider that the full replacement of fluids lost during exercise, even with fluids containing sodium, is the real cause of falling blood sodium concentrations during prolonged exercise. This was one step too far in their thinking at the time.
Their key finding was that when subjects did not drink during exercise, they passed almost no urine (3rd column from the left in Figure 1). But when they drank enough to match their sweat rates, they passed more than 2 liters of urine (7th and 11th columns from left in Figure 1), indicating that their rate of fluid intake was superfluous by perhaps as much as 2 liters; exactly in keeping with Ladell’s conclusions from his studies, which reproduced the effects of being shipwrecked.
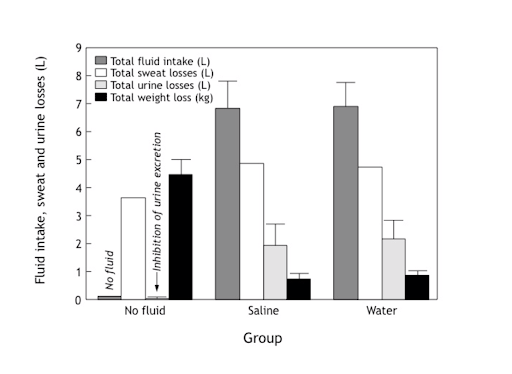
Figure 1: When subjects in the study of Barr and colleagues (38) did not drink at all (no fluid group) during 6 hours of exercise, they passed essentially no urine. But when they drank to prevent any weight loss during exercise (saline and water groups) they passed ~2 liters of urine. Sweat losses were largely unchanged by fluid ingestion during exercise. Reproduced from source 11 (p. 281).
The authors were, I think, a little surprised by the finding that when subjects drank enough to match their sweat rates (saline and water groups), their blood sodium concentrations fell progressively, even when they ingested a sodium-containing drink (Figure 2). Indeed, at the end of the trial, blood sodium concentrations were approaching 135 mmol/L, the level at which we begin to diagnose exercise-associated hyponatremia (EAH). But the authors failed to understand the relevance of their finding.
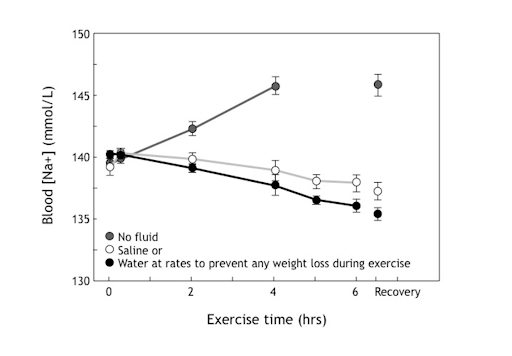
Figure 2: Blood sodium concentrations (mmol/L) in subjects who drank either nothing, saline, or water during 6 hours of exercise. Note that blood sodium concentrations rose when subjects did not drink during exercise, becoming “dehydrated,” but fell when they drank in excess so that they did not lose any weight. Note, also, that sodium ingestion during exercise failed to prevent the fall. The authors were essentially the first to show how EAH develops but failed to interpret this finding correctly.
A year before the publication of this paper, we already had established how EAH and its potentially fatal complication, exercise-associated hyponatremic encephalopathy (EAHE), develop (39). I thus felt compelled to explain (in a nice way, of course), what their findings really meant (40). I wrote that these findings indicate:
[F]luid ingestion during exercise plays a critical role in development of this condition (EAH), for the reason that serum sodium concentrations rose in the subjects who ingested fluid regardless of whether or not the fluid contained sodium. (40)
I concluded:
[Thus] far from preventing a fall in serum sodium concentrations during exercise, it was fluid (and sodium) ingestion that actually caused serum sodium concentrations to fall during exercise. In addition, despite a less negative sodium balance, serum sodium concentrations in subjects who ingested saline were not higher than were those who ingested water. (40)
Figure 3 provides the evidence to support this interpretation.
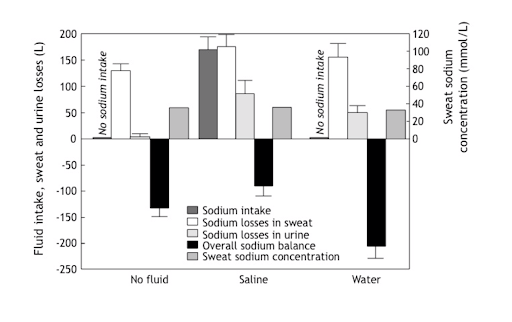
Figure 3: Sodium balance studies in subjects in the study of Barr et al. (38) who ingested either no fluid, saline, or water during 6 hours of exercise. Saline intake during exercise did not influence sweat-sodium concentrations but did increase sodium losses in urine and sweat. Despite this, overall sodium losses were least in those who ingested saline and greatest in those who ingested water. Despite a less negative sodium balance in subjects ingesting saline during exercise (compared to no fluid), blood sodium concentrations fell during exercise in this (saline group) but rose in the no fluid group (Figure 1).
Accordingly, water balance has a greater impact on the development of EAH than does saline ingestion, a finding that the sports drink industry tried to hide for almost two decades.
Everyone also should have noticed that urine production is turned on when subjects are forced to drink enough fluid to prevent any weight loss during exercise — the Zero-Percent Dehydration Doctrine.
That finding alone tells us that the Zero-Percent Dehydration Doctrine is not compatible with our normal human physiology. If there is no weight loss during exercise, the blood sodium concentration must fall, as it did in this experiment (Figure 2). That was the key piece of information that would lead to our discovery of how and why EAH and EAHE occur (39, 41).
Conclusion
The anonymous experts who drew up the 1987 ACSM Position Stand on the Prevention of Thermal Injuries During Distance Running (5) produced two novel dictums for how humans must conduct themselves during exercise.
The first was the decree that, should they wish to avoid “heat illness” during exercise, all athletes must drink according to a pre-arranged schedule. In other words, this committee of experts had decided that humans could no longer trust their own thirst mechanisms to ensure that they drink enough during exercise. In effect, they were claiming that the biological controls driving the thirst mechanism, which have been evolving in land-based mammals for more than 300 million years, are a failure because they don’t work in humans during exercise.
As I will describe in the next column, the second novel dictum that the experts were about to force on us is what I have termed the Zero-Percent Dehydration Doctrine.
The experts’ next push was to ensure that all athletes around the world properly understood these two novel physiological doctrines. They soon would add (false) dictums three, four, and five:
- EAH is caused by excessive body sodium losses during exercise.
- Persons who develop EAH lose large amounts of sodium in their sweat and therefore can be classified as “salty sweaters.”
- EAH can be prevented by the ingestion of an electrolyte-containing sports drink during exercise.
The tragedy, as I will relate, is that they convinced so many to believe their falsehoods.
Additional Reading
- The Hyponatremia of Exercise, Part 1
- The Hyponatremia of Exercise, Part 2
- The Hyponatremia of Exercise, Part 3
- The Hyponatremia of Exercise, Part 4
- The Hyponatremia of Exercise, Part 6
- The Hyponatremia of Exercise, Part 7
- The Hyponatremia of Exercise, Part 8
- The Hyponatremia of Exercise, Part 9
- The Hyponatremia of Exercise, Part 10
- The Hyponatremia of Exercise, Part 11
- The Hyponatremia of Exercise, Part 12
Professor T.D. Noakes (OMS, MBChB, MD, D.Sc., Ph.D.[hc], FACSM, [hon] FFSEM UK, [hon] FFSEM Ire) studied at the University of Cape Town (UCT), obtaining a MBChB degree and an MD and DSc (Med) in Exercise Science. He is now an Emeritus Professor at UCT, following his retirement from the Research Unit of Exercise Science and Sports Medicine. In 1995, he was a co-founder of the now-prestigious Sports Science Institute of South Africa (SSISA). He has been rated an A1 scientist by the National Research Foundation of SA (NRF) for a second five-year term. In 2008, he received the Order of Mapungubwe, Silver, from the President of South Africa for his “excellent contribution in the field of sports and the science of physical exercise.”
Noakes has published more than 750 scientific books and articles. He has been cited more than 16,000 times in scientific literature and has an H-index of 71. He has won numerous awards over the years and made himself available on many editorial boards. He has authored many books, including Lore of Running (4th Edition), considered to be the “bible” for runners; his autobiography, Challenging Beliefs: Memoirs of a Career; Waterlogged: The Serious Problem of Overhydration in Endurance Sports (in 2012); and The Real Meal Revolution (in 2013).
Following the publication of the best-selling The Real Meal Revolution, he founded The Noakes Foundation, the focus of which is to support high quality research of the low-carbohydrate, high-fat diet, especially for those with insulin resistance.
He is highly acclaimed in his field and, at age 67, still is physically active, taking part in races up to 21 km as well as regular CrossFit training.
References
- Hubbard RW, Mager M, Kerstein M. Water as a tactical weapon: A doctrine for preventing heat casualties. Defense Technical Information Center OAI-PMH Repository, 1982, 1-19.
- Montain SJ, Latzka WA, Sawka MN. Fluid replacement recommendations for training in hot weather. Mil. Med. 164(1999): 502-508.
- Kolka MA, Latzka WA, Montain SJ, et al. Effectiveness of revised fluid replacement guidelines for military training in hot weather. Aviat. Space Environ. Med. 74(2003): 242-246.
- Kerstein M, Mager M, Hubbard R, et al. Heat-related problems in the desert: The environment can be an enemy. Mil. Med. 149(1984): 650-656.
- American College of Sports Medicine. Position stand on the prevention of thermal injuries during distance running. Med. Sci. Sports Exerc. 19(1987): 529-533.
- Montain SJ, Coyle EF. Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J. Appl. Physiol. 73(1992): 1340-1350.
- Convertino VA, Armstrong LE, Coyle EF, et al. American College of Sports Medicine position stand: Exercise and fluid replacement. Med. Sci. Sports Exerc. 28(1996): i-vii.
- Armstrong LE, Epstein Y, Greenleaf JE, et al. American College of Sports Medicine position stand: Heat and cold illnesses during distance running. Med. Sci. Sports Exerc. 28(1996): i-x.
- Wyndham CH, Strydom NB. The danger of an inadequate water intake during marathon running. S. Afr. Med. J. 43(1969): 893-896.
- Gisolfi CV, Copping JR. Thermal effects of prolonged treadmill exercise in the heat. Med. Sci. Sports 6(1974): 108-113.
- Noakes TD. Waterlogged: The serious problem of overhydration in endurance sports. Champaign, Illinois: Human Kinetics, 2012,
- Fuller A, Hetem RS, Maloney SK, et al. Adaptation to Heat and Water Shortage in Large, Arid-Zone Mammals. Physiology 29(2014): 159-167.P
- Noakes TD, Adams BA, Myburgh KH, et al. The danger of an inadequate water intake during prolonged exercise: A novel concept re-visited. Eur. J. Appl. Physiol. Occup. Physiol. 57(1988): 210-219.
- Noakes TD. The dehydration myth and carbohydrate replacement during prolonged exercise. Cycling Sci. (June 1990): 23-29.
- Noakes TD. Dehydration during exercise: what are the real dangers? Clin. J. Sports Med. 5(1995): 123-128.
- Noakes TD. Hyponatremia in distance athletes. Pulling the IV on the dehydration myth. Physcn. SportsMed. 28(2000): 71-76
- Noakes TD. Fluid replacement during marathon running. Clin. J. Sports Med. 13(2003): 309-318.
- Noakes TD. Drinking guidelines for exercise: What evidence is there that athletes should drink “as much as tolerable,” “to replace the weight lost during exercise” or “ad libitum”? J. Sports Sci. 25(2007): 781-796.
- Noakes TD. Current drinking guidelines are not evidence-based. In: Physiological bases of human performance during work and exercise. Taylor NAS, Groeller H, Eds. Edinburgh: Elsevier, 2008, 585-592.
- Noakes TD. Is drinking to thirst optimum? Ann. Nutr. Metab. 57(2010): 9-17.
- Hunt EH. The regulation of body temperature in extremes of dry heat. J. Hyg. 12(1913): 479-488.
- Hew-Butler T, Collins M, Bosch A, et al. Maintenance of plasma volume and serum sodium concentration despite body weight loss in Ironman Triathletes. Clin. J. Sports Med. 17(2007): 116-122.
- Knechtle B, Wirth A, Knechtle P, et al. Increase in total body water with decrease of body mass while running 100km nonstop – formation or oedema? Res. Q. Exerc. Sport 80(2009): 593-603.
- Knechtle B, Senn O, Imoberdorf R, et al. Maintained total body water content and serum sodium concentrations despite body mass loss in female ultra-runners drinking ad libitum during a 100km race. Asia Pac. J. Clin. Nutr. 19(2010): 83-90.
- Nolte HW, Noakes TD, van Vuuren B. Ad libitum fluid replacement in military personnel during a 4 hour route march. Med. Sci. Sports Exerc. 42(2010): 1675-1689.
- Nolte HW, Noakes TD, van Vuuren B. Trained humans can exercise safely in extreme dry heat when drinking water ad libitum. J. Sports Sci. 29(2011): 1233-1241.
- Nolte HW, Noakes TD, van Vuuren B. Protection of total body water content and absence of hyperthermia despite 2% body mass loss (‘voluntary dehydration’) in soldiers drinking ad libitum during prolonged exercise in cool environmental conditions. Brit. J. Sports Med. 45(2011) 1106-1112.
- Tam N, Nolte HW, Noakes TD. Changes in total body water content during running races of 21.1 and 56km in athletes drinking ad libitum. Clin. J. Sports Med. 21(2011): 218-225.
- Tam N, Noakes TD. The quantification of body fluid allostasis during exercise. Sports Med. 43(2013): 1289-1299.
- Ladell WS. Effects of drinking small amounts of sea-water. Lancet 242(1943): 441-444.
- Ladell WS. Effect on man of restricted water supply. Br. Med. Bull. 5(1947): 9-13.
- Ladell WS. The effects of water and salt intake upon the performance of men workin