It often happens that the opinions of a single person can turn an interesting but unproven idea or hypothesis into a hallowed, globally accepted dogma for which there is no hard evidence.
The success of Dr. Ancel Keys, Ph.D., in promoting the diet-heart hypothesis is one such example, well known to readers of this website. Perhaps the closest analogy in the Science of Hydration is Dr. Roger W. Hubbard, Ph.D.
Water as a Tactical Weapon: A Doctrine for Preventing Heat Casualties
In the early 1980s, Hubbard, then working for the highly respected and influential United States Army Research Institute for Environmental Medicine (USARIEM), developed a personal vision. He came up with the notion that the U.S. military could use water as a “tactical weapon”: that simply by drinking more water than the forces against whom they were fighting, the U.S. military could achieve greater battle successes whenever they were forced to fight in the heat.
Hubbard wrote:
In order to fulfil mission requirements, individuals must operate at optimal efficiency yet remain free from the serious consequences of dehydration and heat illness (my added emphasis) … The potential for rapid deployment of large numbers of US Forces to either hot-wet or hot-dry regions of Southwest Asia represents, in itself, a substantial medical threat from endemic disease. A failure to prevent unnecessary heat casualties could result in an unacceptable level of non-battle losses and jeopardize the entire operation. Our advocacy of using water as a tactical weapon is based on historical, logistical, physiological and psychological evidence, in addition to personal observations of Army, Marine and Navy Units manoeuvring at 29 Palms, Ft. Irwin, Camp Lejeune and experiences at a variety of southern Army posts, the Philippine Islands, Vietnam, and Israel. (1)
As a result, Hubbard and USARIEM proposed a novel model of exercising and drinking for military personnel, dependant on the prevailing environmental conditions. In brief, as conditions became hotter, military personnel would drink more and exercise less. In the hottest conditions, soldiers would be allowed to exercise for only 20 minutes per hour and forced to rest for the remaining 40 minutes. Each hour, they would need to drink 2.0 quarts of fluid (1.9 L/hr).
These guidelines would be adopted by the U.S. military in 1988 (2, 3), five years after the Gatorade brand had been purchased by the Quaker Oats company.
Hubbard’s guidelines indicate that at that time the key scientists at USARIEM, the most influential such organization in the world, believed the following:
- Heat illness is due to inadequate fluid ingestion during activity.
- As a consequence, all forms of heat illness can be prevented by increasing fluid intake.
- Reducing the amount of exercise and allowing sufficient time for recovery also will reduce the risk of heat illness. Since exercise raises the body temperature in proportion to the metabolic rate (VO2 – previous column), it is logical to assume that reducing the amount of time soldiers are allowed to exercise from 50 to 20 minutes each hour must prevent heat illness, because however much activity soldiers performed in any 10- to 20-minute exercise bout in the heat, their body temperatures would return to near normal values in the 40- to 50-minute rest interval between bouts. As a result, it is difficult to imagine why such a favorable work-rest ratio would not, by itself, prevent “heat illness” in anyone exercising intermittently in the heat.
Why, then, would the resting soldiers also need to ingest copious amounts of fluid “ahead of thirst” to produce an equally favorable outcome? And what evidence did these authors produce to prove that their novel intervention was highly effective?
The study that evaluated the efficacy of this novel doctrine involved 6,010 U.S. Navy and Army reservists, who participated in a 15-day exercise in the Californian desert in temperatures that ranged between 49 and 54 degrees Celsius, or 120 and 129 degrees Fahrenheit (4). The exercise was known as the Combined Arms Exercise (CAX 8-80). The goal of the study was to determine whether these novel guidelines for fluid intake and activity regulation would optimize performance and minimize the risk of “heat illness” under these severe environmental conditions.
The experiment involved two groups of reservists, the control and experimental groups. The study, however, broke the first rule of a randomized controlled trial (RCT) since subjects were not randomized to either of these two groups at the start. Instead, the two groups came from different military units, so they had been identified (and separated) long before the trial had even been planned.
As a result, the two experimental groups were not properly matched, since the experimental group comprised elite soldiers and the control group was made up of more usual soldiers.
It is highly likely that even before the trial began, the two groups differed in the likelihood that they would either develop or, more importantly, seek medical care for any symptoms they might develop during the experiment. Logically, one would expect the more elite soldiers to be more reluctant to seek medical care for the minor symptoms that the authors had categorized as “heat illness” (as discussed subsequently).
Prior to the beginning of the trial, members of the experimental group were given a brief lecture in which they were informed of “six physiological laws governing work in the heat.” The control group did not receive this lecture This, too, is contrary to a good experimental protocol since both groups should have received a lecture in which they were told what was expected of them.
In the brief lecture, the experimental group was told that soldiers, like all humans, are unaware when they are “dangerously dehydrated,” and that it was “therefore, forbidden to have the administration of fluids be dependent upon his (the soldier’s) thirst and desire to drink. Thus, the regular and timely administration and intake of fluids is the responsibility of the commander.”
Here we see, for the first time (of which I am aware), the promotion of the idea that thirst is an inadequate guide to how much we should be drinking.
From where did this novel insight into our human biology suddenly arise? The authors give no explanation. One can only assume that this was Hubbard’s understanding of the human biology necessary to explain his theory.
It is clearly impossible to drink 1.9 L/hr on the basis of thirst. The logic then becomes: To prevent heat illness, soldiers need to drink 1.9 L/hr. Since thirst will not drive anyone to drink at such high rates for prolonged periods, thirst is no longer serving the function we scientists have decided it must, and the only solution is to tell the soldiers that they must drink “ahead of thirst.” As a result, from this day forth, we decree that “thirst is no longer an adequate indication of one’s level of dehydration.” As a result, “all must drink ahead of thirst.”
The problem is that if the vision of this new biology is not real, then any novel guidelines based on that falsehood likely will produce unexpected, perhaps nasty outcomes. As I will show, those nasty outcomes were happening already, though not yet in the United States, and not yet in the military. They were happening in ultramarathon runners in my own country, South Africa.
The six laws that the experimental group were taught in their brief lecture were presumably provided by the two physiologists who co-authored the article, Hubbard and Dr. Milton Mager, Ph.D. Those laws give us insight into the intellectual biases that each had acquired as part of their training and experience at USARIEM.
Importantly, it is unclear where those six laws originated, since there is nothing in the publication record of either Mager or Hubbard that suggests these laws were the result of a progressive accumulation of carefully conducted research findings leading to the unavoidable conclusion that those novel guidelines would produce the desired outcomes.
At the time of this experiment, neither Mager nor Hubbard had published a single study in which they evaluated the effects of fluid ingestion on the performance and health of exercising humans. Instead, their major research interest was the development of an animal model of heatstroke using rats as their experimental subjects (5).
In addition, the first author of the article, Dr. Morris Kerstein, MD, was at the time a professor of surgery at the University of Tulane. Although he had published widely on surgical conditions in humans, he had no previous publications dealing with exercise and fluid ingestion.
Moreover, it seems that none of the authors had previously conducted a field trial involving a large number of subjects.
For the purposes of this experiment, the control group of soldiers did not receive the novel information recently conceived by the USARIEM scientists. Instead, they were provided with the standard U.S. military information about how soldiers are to conduct themselves when exercising in the heat. Nor was the fluid intake of the control subject regulated as might have been expected in a study purporting to determine whether fluid ingestion alters the risk of developing “heat illness”; fluid was provided “generously” to these soldiers at the “usual stopping sites.” I was unable to find a record of exactly how many soldiers were included in the experimental and control groups.
It is beginning to seem that, like Professors Cyril Wyndham and Nic Strydom’s study (6), which I dissected in my previous column, this study was poorly designed and lacked any possibility of actually testing the authors’ hypothesis. Instead, it is as if the authors had concluded what they wanted to find even before the study began.
During the experiment, 1,387 soldiers (23% of the total) reported for medical care. Of these, 286 were considered to have “heat-related” symptoms, and these included 110 cases of heat exhaustion, 53 cases of headache, 31 cases of cramps/nausea, 46 cases of nosebleed, and 46 cases of eye irritations. If each case removed the soldier from the battlefield for 4 hours, the authors concluded that these various “heat illnesses” caused 1,144 man-hours of lost duty.
The authors remarkably did not provide a detailed breakdown of the distribution of cases of “heat illness” in the experimental and control groups. They instead simply concluded that since there were no cases of “heat illness” in the experimental group, their experiment proved:
- Water should be considered a tactical weapon.
- Commanders, who modify the activity levels of their units as the heat stress level increases and, additionally, enforce drinking in the absence of thirst, can maintain a viable and efficient fighting force under any environmental condition encountered in the desert.
They further suggested, “The purpose of publishing these data from a military exercise is to provide other investigators, who treat full-time athletes, part-time athletes (my added emphasis), and individuals with heat-related problems with the information that there are methods for preventing heat-related illnesses.”
“Ammunition,” they wrote, “can be defined as any material used to attack or defend a position. Should that position include a battle against the heat and arid climate, the primary ammunition will be water (my emphasis).”
On the basis of this study, the authors believed they had solved the problem of heat illness, not just in the military but in all exercisers doing any form of activity in the heat. The solution was simple: Drink ahead of thirst and at rates of up to 1.9 L/hr if environmental conditions are severe.
I contend that the papers by these authors (1, 4) are the two most important historical documents in the published literature relating to fluid ingestion during exercise. They are even more important than the study of Wyndham and Strydom (6). As I will show, they introduced a revolutionary concept to the U.S. military, and from there — via the American College of Sports Medicine, the Gatorade Sports Science Institute, and the National Athletic Trainers Association — to all English-speaking athletes and recreationally active persons around the globe. They are revolutionary documents.
Yet it is also clear that the experiment they reported never could have proved what they claimed. Instead, the authors fell into the trap of believing their own vision, regardless of the facts.
First, the experimental study they describe is designed to test the hypothesis that in soldiers who have unlimited access to fluid during exercise, only the subjects who drank at rates beyond those dictated by their thirst would avoid developing serious health consequences, particularly “heat illness” resulting from dehydration.
But the assumption that “dehydration” causes “heat illness” such that all those with “heat illness” must be dehydrated and conversely those without “heat illness” are properly hydrated cannot be assumed since it has never been proven. In my previous columns, I detailed how these false ideas arose from the incorrect interpretations applied to the study of Wyndham and Strydom (6).
Instead of directly evaluating that hypothesis, the design of this experimental trial merely assumed that a lower incidence of heat illness must have been due to more appropriate fluid replacement and an avoidance of “dehydration” in the experimental group — the group that had been taught in one “brief lecture” that they must drink “ahead of thirst.” A scientific experiment cannot make that assumption, however, because the soldiers were told they must drink “ahead of thirst” and at a rate of 1.9 L/hr, they actually did that in the experiment.
So proving rather than assuming there was a difference in drinking behaviors in the two groups — and that this produced different levels of dehydration which then explained differences in the rates of “heat illness” between the experimental and control groups — requires at the very least that all participants in the experimental and control groups must be weighed before and after the exercise bouts in which some developed “heat illness.” This would have established whether the reportedly lower incidence of heat illness in the experimental group was indeed because its members were less “dehydrated” because they had drunk more. This also would have established whether the experimental group drank at rates as high as 1.9 L/hr.
The authors did not measure weight changes in either group, so they were unable to prove that the prevention of “dehydration” by drinking ahead of thirst at rates of up to 1.9 L/hr explained their findings.
Instead, they assumed that the lower rates of “heat illness” in the experimental group proved that they had drunk more and were less dehydrated.
I often say that what you believe determines what you believe. The authors of this study used a circular argument to “prove” what they already believed before the experiment began (Figure 1).
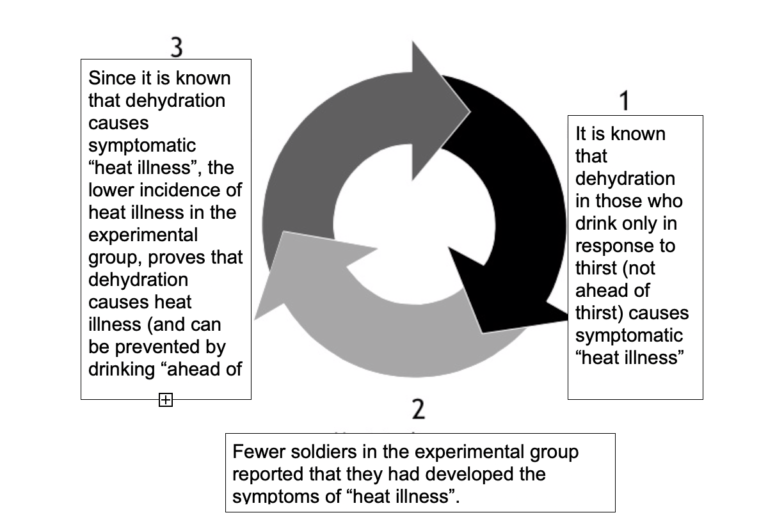
Figure 1: The circular argument present in the study of Kerstein, et al. (4), that launched the “drink ahead of thirst” doctrine for a global audience
Second, as already argued, the basis for any intervention RCT is that subjects in both groups must essentially be identical, since they were randomized from a general population to either the experimental or control groups. But this was certainly not the case in this study, as the experimental group comprised four companies that led the attack and were classified in military terms as “high risk.”
It is probable that “high risk” soldiers who graduate to lead companies are selected because they have valuable and unusual personal and physical characteristics. Indeed, the authors acknowledged that the experimental subjects “were selected for special treatment because they were considered highly motivated and could be expected to put forth maximal effort in the forthcoming exercise.” In contrast, the control group came from the other units that were not involved in “high risk” military activities. This at least raises the question of which group would be more likely to complain of vaguely defined “heat illness” from specific but varied psychological contexts.
Which brings us to our third point: the definition of what constitutes a “heat illness” for this study was even vaguer than usual. It included complaints of headache, cramps/nausea, nosebleeds, and eye irritations. It is difficult to understand how these later categories, which comprised 176 cases (62% of the total of 286 cases), could ever seriously be categorized as “heat illnesses.” Their inclusion suggests that the authors chose to dilute the diagnostic criteria for “heat illness,” perhaps because this dilution would produce more cases of “heat illness” in the control group and so favor their preconception that fluid ingestion during physical activity reduces the incidence of “heat illness.”
Fourth, there is no table in the text showing exactly how many subjects were in each group or the precise number who developed “heat illness” in the different categories. It is not possible to determine whether the apparent absence of cases of heat illness in the experimental group is a real finding.
Fifth, in discussing their results, the authors pay almost no attention to the role of fluid ingestion in the outcome of their studies. This is understandable, since they had not measured the body mass of any subjects during the exercises, so they could not determine the levels of “dehydration” present in soldiers in the experimental and control groups. Nor had they recorded their rates of fluid ingestion. They could have no idea of how much or how little fluid subjects with or without “heat illness” had drunk during exercise, or whether the apparent absence of cases of “heat illness” in the experimental group was because subjects in that group had drunk more and were therefore less “dehydrated.”
If there truly were no cases of heat illness in the experimental group, this could have been because (i) they were superior athletes with better motivation and therefore at low risk of seeking medical care for a “heat illness”; (ii) they exercised more carefully in the heat and rested more; (iii) they drank more and therefore became less dehydrated during the trial; or (iv) a combination of (i), (ii), and (iii).
Thus, perhaps as in the case of Wyndham and Strydom (6), the authors of this study had concluded exactly what they were bound to conclude, even before the experiment began. They had no need to undertake the study except to convince others by publishing as a “scientific article” that which they believed to be the “truth” but which was completely independent of the facts.
The tragedy of this study was that it failed to establish whether drinking at such high rates (up to 1.9 L/hr in more severe heat) is beneficial—or, even more important, whether it is safe.
Instead, this novel doctrine was accepted without proper scrutiny, first by the USARIEM and then by the American College of Sports Medicine/Gatorade Sports Science Institute alliance. It was as if a religious dogma, immune to scientific scrutiny, had been handed down to man from a higher authority. Sadly, those who used this information for the development of future drinking guidelines were guilty of believing the religion and ignoring the science.
So the question may be asked: Is the science of fluid replacement during exercise — the Science of Hydration — actually based on science?
Or had it become a religion?
Additional Reading
- The Hyponatremia of Exercise, Part 1
- The Hyponatremia of Exercise, Part 2
- The Hyponatremia of Exercise, Part 3
- The Hyponatremia of Exercise, Part 5
- The Hyponatremia of Exercise, Part 6
- The Hyponatremia of Exercise, Part 7
- The Hyponatremia of Exercise, Part 8
- The Hyponatremia of Exercise, Part 9
- The Hyponatremia of Exercise, Part 10
- The Hyponatremia of Exercise, Part 11
- The Hyponatremia of Exercise, Part 12
Professor T.D. Noakes (OMS, MBChB, MD, D.Sc., Ph.D.[hc], FACSM, [hon] FFSEM UK, [hon] FFSEM Ire) studied at the University of Cape Town (UCT), obtaining a MBChB degree and an MD and DSc (Med) in Exercise Science. He is now an Emeritus Professor at UCT, following his retirement from the Research Unit of Exercise Science and Sports Medicine. In 1995, he was a co-founder of the now-prestigious Sports Science Institute of South Africa (SSISA). He has been rated an A1 scientist by the National Research Foundation of SA (NRF) for a second five-year term. In 2008, he received the Order of Mapungubwe, Silver, from the President of South Africa for his “excellent contribution in the field of sports and the science of physical exercise.”
Noakes has published more than 750 scientific books and articles. He has been cited more than 16,000 times in scientific literature and has an H-index of 71. He has won numerous awards over the years and made himself available on many editorial boards. He has authored many books, including Lore of Running (4th Edition), considered to be the “bible” for runners; his autobiography, Challenging Beliefs: Memoirs of a Career; Waterlogged: The Serious Problem of Overhydration in Endurance Sports (in 2012); and The Real Meal Revolution (in 2013).
Following the publication of the best-selling The Real Meal Revolution, he founded The Noakes Foundation, the focus of which is to support high quality research of the low-carbohydrate, high-fat diet, especially for those with insulin resistance.
He is highly acclaimed in his field and, at age 67, still is physically active, taking part in races up to 21 km as well as regular CrossFit training.
References
- Hubbard RW, Mager M, Kerstein M. Water as a tactical weapon: A doctrine for preventing heat casualties. Defense Technical Information Center OAI-PMH Repository. 1982: 1-19.
- Montain SJ, Latzka WA, Sawka MN. Fluid replacement recommendations for training in hot weather. Mil. Med. 164(1999): 502-508.
- Kolka MA, Latzka WA, Montain SJ, et al. Effectiveness of revised fluid replacement guidelines for military training in hot weather. Aviat. Space Environ. Med. 74(2003): 242-246.
- Kerstein M, Mager M, Hubbard R, et al. Heat-related problems in the desert: The environment can be an enemy. Mil. Med. 149(1984): 650-656.
- Hubbard RW, Bowers WD, Matthew WT, et al. Rat model of acute heatstroke mortality. J. Appl. Physiol. 42(1977): 809-816.
- Wyndham CH, Strydom NB. The danger of an inadequate water intake during marathon running. S. Afr. Med. J. 43(1969): 893-896.