In the previous column, I explained how Ancel Keys, once a cholesterol denialist, suddenly shifted his position on dietary factors related to heart disease and came to use weak epidemiological evidence to advance the diet-heart and lipid hypotheses. I also described how Keys became the leading researcher on this topic despite the fact that other researchers, such as Drs. Haqvin Malmros and John Gofman, had preceded him in developing the relevant research and were more qualified to conduct such scientific inquiry. In this column, I delve further into the details of Keys’ hypotheses and his strategic selection of data to support them.
Recall the 1953 graph for which Keys became famous:
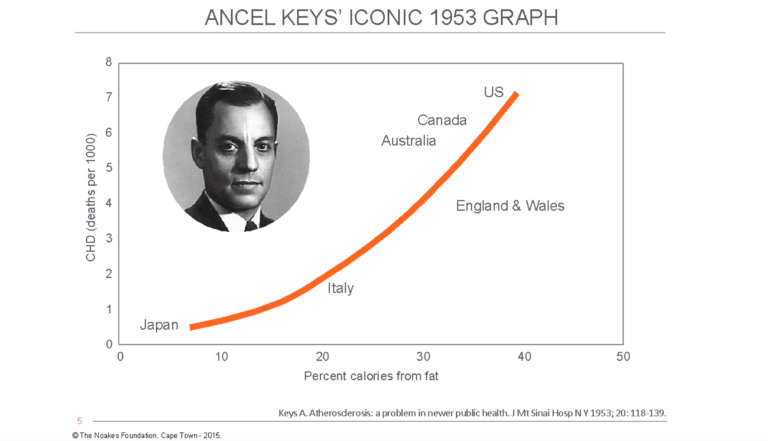
Figure 1: In his 1953 paper (8), Keys included data from six countries, apparently showing a close relationship between the increasing percentage of fat in the diet (as a percentage of total calories) and deaths per 1,000 persons from degenerative (atherosclerotic) heart disease. He hypothesized that this (associational) relationship could be explained by higher blood cholesterol concentrations in persons living in countries ingesting more dietary fat, as in the U.S., Canada, and Australia. Reproduced from reference 8.
Also recall Keys’ very strategic selection of data points from the World Health Organization’s (WHO) available data in order to create the appearance of a correlation between dietary fat intake and CHD (Figure 2).
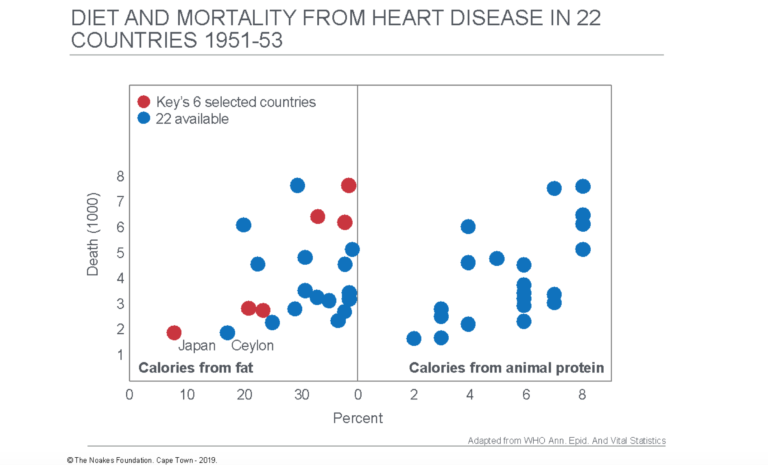
Figure 2: The data Keys sourced to draw up his famous 1953 figure came from an annual publication produced by the WHO. The left panel in this figure shows the data for annual death rates versus calories from dietary fat for 22 countries for which data were then available. Keys selected just six of those countries (red dots) and excluded the remainder (blue dots). Reproduced from references 34 (p. 6) and 35 (p. 923).
Below, I discuss several critiques of Keys’ methodology — both my own critiques and those published by his contemporaries — suggest alternative interpretations of the data available to him, and explain how he convinced the world his hypothesis was the singular truth, altering the trajectory of 70 years of medical practice and dietary guidelines.
Keys argues dietary fat consumption causes coronary heart disease (CHD) epidemic in U.S.
Keys’ wartime research on starvation showed a reduction in dietary fat consumption was associated with (or produced) a dramatic reduction in CHD mortality. Keys therefore needed to develop his hypotheses based on another, but opposite, natural experiment — one that showed increasing dietary fat intake in the U.S. since 1910 was associated with (or produced) the sudden rise in CHD.
Keys claimed that in the U.S., dietary fat consumption had risen from 32% of total daily calories in 1910 to 33% in 1920, 35% in 1930, 38% in 1940, and 40% in 1950 (8). Since coronary atherosclerosis requires decades to develop, Keys’ argument became that a 3-6% change in dietary fat intake from 1910 to 1940 was sufficient to initiate the coronary atherosclerosis “epidemic” of the 1950s.
This means that if male U.S. citizens were eating 2,500 calories per day during this period, then in 1910, 32% of those calories (800 calories) would be ingested as calories from fat. Since 1 gram of fat provides 9 calories, the average U.S. male citizen was eating 89 grams of fat per day in 1910. But in 1950, when the CHD epidemic was well established, that same average citizen was eating 1,000 calories of fat per day, or 111 grams a day.
Thus, according to this theory, a 22 grams/day (25%) increase in daily fat intake was sufficient to initiate the global heart disease epidemic of the 1950s.
To give this further context, a 22 grams/day increase in dietary fat would be the equivalent of adding any one of the following to one’s daily diet: either four eggs, 28 grams of fatty fish, 80 grams of cheese, three-quarters of an avocado, a quarter cup of cashew nuts, or a tablespoon and a half of extra-virgin olive oil.
So according to Keys’ 1953 explanation, the CHD epidemic of the mid-20th century happened because, at some moment after the 1930s, the citizens of the U.S. began inexplicably to make unwise and life-threatening dietary choices. This, in essence, is Keys’ diet-heart hypothesis: that increased dietary fat intake is the direct cause of CHD.
In his book first published in 1959, Keys described his hypothesis:
The most important point about the diet … is that the fats we eat have a major effect on the amount of cholesterol in the blood, and it is this cholesterol which is deposited in the walls of the arteries. The more common fats in our American diet – meat and dairy fat, margarine and hydrogenated shortenings – tend to raise the blood cholesterol. On the other hand, most common food oils (liquid fats) generally have no such effect or may even work in opposition. … Besides fats, other factors in the diet may influence the blood cholesterol level and the development of coronary heart disease. Most populations that have relatively little coronary disease live on diets that are rather high in leafy vegetables and fruits as well as low in sugar and in meat and dairy fats. (1, p. 14-15)
In a 1961 interview with Time magazine (36), Keys explained how elevated blood cholesterol concentrations directly cause coronary atherosclerosis, sometimes colloquially called “clogging of the arteries.” This is his second hypothesis, the lipid hypothesis.
“As the fatty protein molecules travel in the bloodstream, they are deposited in the intima, or inner wall of a coronary artery. The proteins and fats are burned off, and the cholesterol is left behind. As cholesterol piles up, it narrows, irritates and damages the artery, encouraging formation of calcium deposits and slowing circulation,” Keys told Time magazine (my emphasis). “Eventually, says Keys, one of two things happens. A clot forms at the site, seals off the flow of blood to the heart and provokes a heart attack. Or (more commonly, thinks Keys) the deposits themselves get so big that they choke off the artery’s flow to the point that an infarct occurs: the heart muscle is suffocated, cells supplied by the artery die, and the heart is permanently, perhaps fatally injured” (36).
Just for noting at this juncture of the argument: For Keys’ explanation to be correct, the initial damage in the development of atherosclerosis must occur directly under the surface of the arterial wall, in the upper layer of the intima. But V. M. Subbotin (37) provides modern evidence that this is not what happens. Instead, the initial lesion is exactly where Paul Dudley White had depicted it in his 1946 textbook (3, facing p. 480): deep in the intima, “just overlying the media (the muscular layer of the artery).” As W. E. Stehbens has argued, atherosclerosis is a “hemodynamic disease and … the disease develops irrespective of the blood cholesterol level” (38, p. 27).
In time, Keys recommended the following as part of the ideal diet for the prevention of coronary heart disease (1, p. 43):
- Restrict use of fats in dairy products and in ordinary meats.
- Use vegetable oils in cookery, not as medicine.
- Avoid hydrogenated products but if you insist on a spread, use the newer margarines.
- Avoid heavy use of salt and sugar.
- Favor fish, shellfish, poultry, fresh vegetables, fruits, non-fat milk products.
Ultimately, this would become known as the Mediterranean diet, although it is not clear which Mediterraneans actually follow it.
The 1955 Seminar of the World Health Organizations (WHO) Study Group on Atherosclerosis and Ischaemic Heart Disease
In the previous column, I explained how Keys strategically selected data from an annual WHO publication to demonstrate a correlation between fat consumption and heart disease. Keys first presented his interpretation of the highly selected data (8) at a 1955 conference organized by the WHO. At the symposium, he said, “There is a remarkable relationship between the death rate from degenerative heart disease and the proportion of fat in the national diet.” This was considered a reasonable statement of fact. But what was not acceptable was his speculative conclusion that “no other variable (than dietary fat) … shows anything like such a consistent relationship (with heart disease rates)” (39, p. 8). It was this statement that would ignite the debate.
Keys’ presentation was vigorously interrogated by Jacob Yerushalmy and Herman Hilleboe, who published their arguments two years later, in 1957 (33). They emphasized that Keys presented data that were purely associational. That is, his data points were related in time and place, but there was no proof that the two variables had a cause and effect relationship with each other. Yerushalmy and Hilleboe pointed out that “no matter how plausible such an association may appear, it is not in itself proof of a cause-effect relationship” (33, p. 2343). They continued by warning: “But quotation and repetition of the suggestive association soon creates the impression that the relationship is truly valid, and ultimately it acquires status as a supporting link in a chain of presumed proof” (p. 2343, my emphasis). In fact, quotation and repetition became the hallmark of the method by which Keys convinced the world his hypothesis was the singular truth.
Yerushalmy and Hilleboe’s next concern was that Keys had used data from only six countries, whereas data were available for 22.
To explain why this was an important weakness, they produced a figure showing that by considering data from only six countries, it was possible to show an inverse relationship between deaths from vascular lesions of the brain (strokes) and fat calories as a percentage of total calories (Figure 3). Those data would then support the conclusion that a high-fat diet protects against the development of atherosclerotic disease of the (cerebral) arteries in the brain while at the same time (according to the Keys’ hypothesis) causing atherosclerotic disease of the (coronary) arteries supplying the heart. Clearly this is implausible. It is more plausible, as I will argue in my next column, that an elevated blood cholesterol concentration is not the immediate cause of either of these conditions.
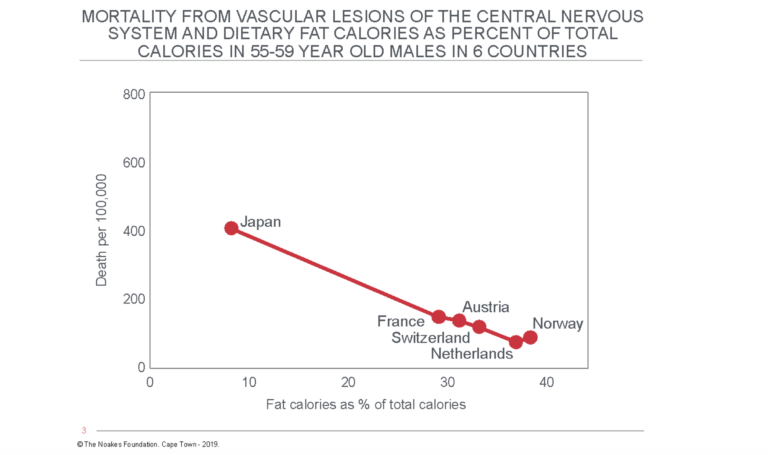
Figure 3: An apparently inverse relationship exists between mortality from cerebrovascular disease and the dietary fat intake as a percentage of total calories in six countries, cherry-picked for demonstration purposes by Yerushalmy and Hilleboe (33). This would imply (according to Keys’ logic) that a high-fat diet is healthy because it prevents strokes. For obvious reasons, this figure is never mentioned by those who believe Keys’ diet-heart hypothesis. Reproduced from reference 33.
Yerushalmy and Hilleboe wrote, “Of course it is obvious that no such conclusion should be inferred” (p. 2345). In passing, they drew attention to the paradox presented by the data from Japan: “It is interesting to note that Japan which has the lowest death rate from cardiovascular disease has the highest death rate from cerebrovascular disease” (p. 2345).
They then produced their own iconic graph, which included the data from all 22 countries (33, Figure 4). They noted adding more countries to the six Keys selected showed that “in the narrow band between 30 and 40 per cent dietary fat intake, [there is] the entire gamut of heart disease mortality ranging from less than 300 per 100,000 for Austria … [to] as much as 739 for the United States” (p. 2345). Furthermore, “In countries with approximately the same proportion of the diet available as fat, the heart disease mortality ranges from 220 to 739 per 100,000” (p. 2345-2346). Hence, “the selection of the original six countries, for whatever reason, greatly exaggerated the importance of the association,” they concluded.
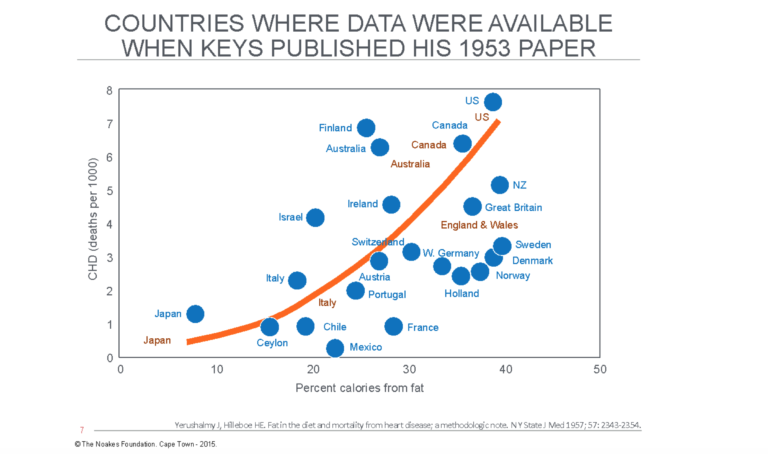
Figure 4: Yerushalmy and Hilleboe (33) included data from another 16 countries ignored by Keys when he drew up his iconic 1953 figure (Figure 1). These data show the truth is not as simple as Keys’ figure attempts to show. For example, the range of fat intakes between 30-40% produces a seven-fold difference in CHD rates ranging from ~100 per 100,000 persons in France to >700 per 100,000 in the United States. Thus, dietary fat intake cannot be the exclusive explanation for different heart disease rates in different countries. Reproduced from reference 33.
The authors then completed a detailed analysis of the association of 15 dietary factors with all-cause mortality and mortality from all causes other than diseases of the heart.
They found, “The association between dietary protein and heart disease … was at least as strong as that between dietary fat and heart disease … . This clearly suggests that the dietary fat-heart disease association (i.e., the diet-heart hypothesis – my addition) is not unique or specific since the association between fat and heart disease mortality is not as strong as that between animal protein and heart disease” (p. 2349).
Then, to further disprove Keys’ interpretation of the data, they found that higher intakes of fat and animal protein were negatively associated with death from all causes other than heart disease. In other words, if higher intakes of fat and animal protein were indeed causing death from heart disease, then they were also protecting against other important causes of death. But this is paradoxical, since heart disease was then the leading cause of death.
In their final damning conclusion, they wrote:
The evidence from 22 countries for which data are available indicates that the association between the percentage of fat calories available for consumption in the national diets and mortality from arteriosclerotic and degenerative heart disease is not valid; the association is specific neither for dietary fat nor for heart disease mortality. Clearly this tenuous association cannot serve as much support for the hypothesis which implicates fat as an etiologic factor in arteriosclerotic and degenerative heart disease. (p. 2350)
They continued by giving Keys an even more thorough lesson in the dangers of drawing definitive conclusions from associational, population-based, epidemiological studies:
But herein lies the pitfall. Because it is well understood that an “association” is at least only a small part of the etiologic story, there is a tendency to deal with the associations uncritically or superficially … . Evidence for an association must be carefully scrutinized and scientifically weighed … the primary data must be evaluated for relevance, accuracy, and internal consistency, and the results must be tested for validity … . If the association is not specifically related to the variables but rather reflects a relationship with extraneous or irrelevant factors, it is worse than useless. … In the proposition considered in this paper — the suggested association between fat in the diet and heart disease mortality — the examination of all available basic data and the tests for specificity show that the association lacks validity. Consequently the apparent association in itself cannot serve as supporting evidence for the theory that dietary fat plays a major role in heart disease mortality. (p. 2351)
History must judge why Keys’ weak hypothesis, and not its demolition by Yerushalmy and Hilleboe — not only survived but was embraced and promoted by the medical community for at least the next seven decades. How can we possibly explain this apparent scientific anomaly?
Keys’ response to the intellectual hammering he received from Yerushalmy and Hilleboe was two-fold. It was, according to his colleague Henry Blackburn, MD, “the pivotal moment in Keys life” (29, p. 36). “Keys got up from being knocked to the ground and said, ‘I’ll show these guys,’ and designed the Seven Countries Study.”
More immediately, he crafted a response which was also published in 1957 (41). In it, Keys adopted a novel argument based on circumlocution.
Keys’ rebuttal was that he was trying to prove a causal relationship that Yerushalmy and Hilleboe claimed did not exist: “It appears that Dr. Hilleboe’s extreme caution about drawing conclusions may be biased in favor of negative versus positive conclusions; surely the lack of causal relationship is no less difficult to prove than that a given effect is the result of a given cause. I doubt that Dr. Hilleboe really believes he has adequate evidence to state that there is not a causal relationship between dietary fat and the tendency to develop atherosclerosis in man” (p. 552).
In other words, Keys claimed the right to condemn fat on the basis of an unproven hypothesis, itself based on circumstantial, associational evidence. But its disproof — that is, the proof that it is safe to eat dietary fat — could only be provided by appropriately conducted scientific investigation that would, of course, take many years and much money to complete.
According to Keys’ logic, until such an investigation was done, his hypothesis must remain as the truth. And, one might add, it has done so until even today, so successful was Keys’ subterfuge.
As a result, “Keys not only launched the cholesterol/fat paradigm, he also biased the debate in its favour” (39, p. 14).
As investigative journalist Nina Teicholz has detailed in her definitive book (29):
In other words, Keys wanted his hypothesis to be presumed right until proven wrong. Yet — and this is an important point — science is not like the justice system. Whereas Americans are presumed to be innocent until proven guilty, scientific knowledge is just the opposite: a hypothesis must not be presumed right until a pile of significant evidence grows up behind it, and even then, you can never be entirely sure. All that one can ever really say is the preponderance of the evidence tends to support one idea over another. Keys’s unwavering belief in his own hypothesis, even in its formative stages and even in the face of conflicting evidence, however, suggests he was willing to stray from these scientific principles to defend it (his hypothesis). (29, p. 36)
Another Keys critic who also happened to be in attendance at the 1955 WHO seminar was Edward H. Ahrens, Ph.D. Ahrens began a rebuttal article of Keys (42) with the statement: “There is a serious lack of direct evidence that atherosclerosis is due to alterations in fat metabolism. Yet, the hypothesis is made attractive by various lines of reasoning — pathological, clinical, and epidemiologic” (42, p. 1905). He then described his own studies showing how blood cholesterol concentrations can be reduced by substituting “vegetable” oils (peanut, cottonseed, corn, and safflower) for saturated fats, or by eating a vegetarian diet.
Ahrens continued by warning that the “various lipid levels do not vary in a parallel manner and that a total cholesterol value may give little indication of the other lipid levels” (p. 1909). Here, he was referring to the problem of carbohydrate-sensitive hypertriglyceridemia, which he believed was the important predictor of heart attack risk and to the identification of which he had made a significant contribution (43).
He concluded, “In view of the fact that it has not been demonstrated in man that lowered levels of serum lipids will alter his susceptibility to atherosclerosis and in view of the many questions that remain unanswered in this year 1957, it seems inadvisable at this time to recommend that the general public eat more or less fat or avoid fat of any kind. We believe that much more basic information must be gathered before widespread changes in dietary habits are adopted” (p. 1911).
But then he condoned the prescription of a low-fat diet to lower blood cholesterol concentrations in those considered to be at the greatest risk. This seems illogical, especially since he concluded the article by restating, “The hypothesis that dietary fats affect atherogenesis however plausible and appealing, remains unproved … . Radical changes in dietary habits are not recommended to the general public at this time” (p. 1911).
In opinion pieces published over the next 30 years (44-46), Ahrens became only more outspoken in his criticisms of the use of the diet-heart hypothesis to promote population-based dietary changes: “The argument for such dietary changes is supported mainly by extrapolations from epidemiological data and from animal experimentation. Reasons are given for concluding that recommendations are unwise, impractical, and unlikely to lead to reduced incidence of atherosclerotic disease” (44, p. 1345).
Note that this statement was made in 1979, fully 22 years after Keys’ original battle with Yerushalmy and Hilleboe. One would have thought that by then, Keys and his comrades would have come up with some definitive evidence to support their (already enacted) population-wide dietary changes.
Ahrens also reviewed the 1979 Consensus Statement of the American Society of Clinical Nutrition (44), which had clearly described the problems that arise when one relies on associational studies to “prove” causal relationships:
In regard to dietary fats, cholesterol, and atherosclerotic disease, the panel concluded that the association of these two factors to arteriosclerotic disease among population groups was strong, but within population groups weak; that the strength and independence of the association were weakened by the confounding effects of a number of genetic, environmental, and socioeconomic factors; that proof from necropsy evidence was either lacking or confounded by other factors; that the effects of changing the intakes of saturated fats and cholesterol both in primary and in secondary prevention trials offered suggestive but not definitive proof of the association; that animal experimentation had succeeded in producing models of arteriosclerotic disease in some but not all species with wide differences in responsiveness to the intake of cholesterol and saturated fat even within species; and that the underlying biological explanations were not well understood. (44, p. 1346)
The report also noted:
The panel as a whole voted that the evidence relating the intake of saturated fat and dietary cholesterol to atherogenesis in man was convincing; further, they agreed that a reduction of saturated fat and cholesterol would lead to reduced levels of plasma cholesterol. On the other hand, the evidence of disease prevention by diet modification was considered unconvincing. Thus the panel could not guarantee that lipid-lowering by dietary means would necessarily lead to a reduced incidence of new events of CHD.
Ahrens’ warned: “The fact that the available evidence is soft ensures that opinions are divided. The fact that the argument has recently become less objective seems to me to be proof-positive that the experts do not yet know — for sure — what to advise and when to advise it” (p. 1345).
Cleary, Ahrens was not of the opinion that, at that time, Keys or anyone else had produced any new evidence to prove his hypothesis sufficiently to justify population-based dietary changes. He repeatedly emphasized, “There has been no previous test of the ‘prudent’ diet” (p. 1346) and “a trial of the low-fat dietary regimen recommended by the McGovern Committee (47) and the American Heart Association (48) has never been carried out.”
Six years later, in response to the statement produced by the National Institute of Health Consensus Development Conference on Lowering Cholesterol to Prevent Heart Disease, Ahrens’ critique included the following (45):
I know of no evidence that the prudent diet will prevent the development of arterial atheroma at any age: the hypothesis is reasonable but not proven, especially in children considered to be at high by the panel criteria … . One of the weaknesses of the consensus statement is the failure to acknowledge the paucity of data available to us with regard to risk/benefit ratios of the prudent diet or of the several alternatives discussed above … . I would have been content with the consensus statement if it had confined itself to what we do know what we do not. It promises benefit without giving the evidence to back up that promise. By failing to emphasize we do not know the statement sweeps these weaknesses in our evidence under the rug as it they were trivial. I have disagreed with that position. (pp. 1086-1087)
Ahrens’ prediction that the recommendations were unwise would turn out to be spot on. By 1985, the immediate result of these population-based dietary guidelines that were not based on firm evidence was beginning to appear. The incidence of obesity, especially in the U.S., was starting to rise exponentially.
Or perhaps it’s the sugar in the diet?
The fatal weakness of associational studies is the undetected “confounding effects of a number of genetic, environmental, and socioeconomic factors” alluded to by the American Society of Clinical Nutrition. In 1957, British nutritionist Dr. John Yudkin, MD and Ph.D., began to suggest that in his rush to condemn saturated fat, Keys had perhaps overlooked any possible effects of high sugar intake in persons living in countries in which dietary fat intake was also high.
Thus, in 1957 Yudkin presented his rebuttal to Keys’ hypothesis. He began by stating that: “As more and more of these awkward facts turn up, one begins to have the uneasy feeling that both the proponents and the opponents of a dietary hypothesis are quoting only those data which support their view” (49, p. 155). His general conclusion was “coronary thrombosis is associated with higher living standards,” so “it is difficult to support any theory which supports a single or major dietary cause of coronary thrombosis” (p. 162). Instead, he preferred “a theory of multiple causes” (p. 162). But sugar (Figure 5) was the single dietary factor that best matched CHD mortality rates in the countries either included or excluded by Keys in his initial analysis (Figure 1).
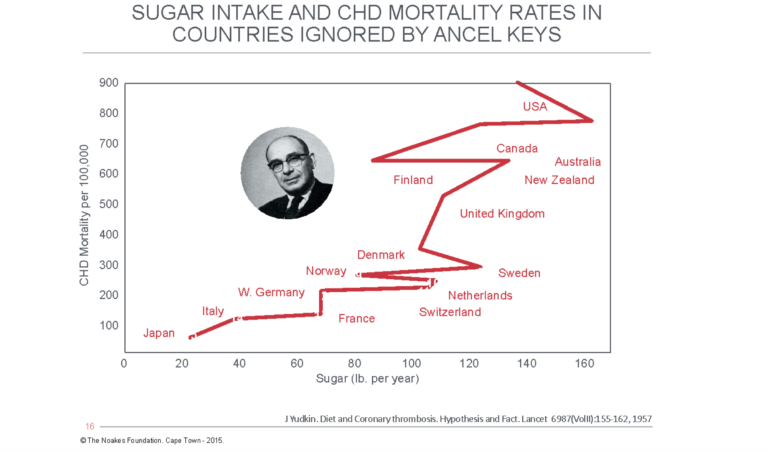
Figure 5: When Yudkin evaluated possible alternate dietary explanations for the rising CHD rates of the 1950s, he found sugar intake was more closely associated with CHD mortality than was dietary fat intake in 15 countries, the majority of which were not included in Keys’ original analysis (Figure 1). Reproduced from reference 49.
Subsequently, Yudkin proposed the hypothesis that increased sugar intake, far from being simply a marker of wealth, might actually be the direct cause of CHD (50).
In his 1964 paper (50), he proposed an alternate hypothesis to that of Keys. He suggested the association between fat intake and CHD mortality might be explained by an “extremely close association between national consumption levels of fat and sugar” (p. 4). He observed, “Many of the sugar-containing foods that we eat contain also fat. These include many cakes, sweets, biscuits, chocolates, ice-cream and several sorts of puddings” (p. 5). He concluded: “Statistics relating fat intake to ischemic heart-disease or diabetes mellitus in different populations may therefore express only as indirect relationship, and the causal relationship may be with sugar” (p. 5). Subsequently, Yudkin would establish that sugar intake was higher in persons with CHD than in disease-free comparison groups (51, 52).
Naturally, Keys could not let this challenge go unanswered, so in the dismissive manner that was his personal trademark, he began his response: “Most students of the etiology of CHD have recognized that the arguments for a role of sucrose in CHD are tendentious and the evidence flimsy indeed; they tend to ignore the occasional reiterations in the popular press. But such neglect leaves the way open for exploitation. A brief review seems overdue” (53, p. 193).
Keys’ bluster would win the day and Yudkin’s life and career would ultimately be destroyed: “Prominent nutritionists combined with the food industry to destroy his reputation, and his career never recovered … . He found himself uninvited from international conferences on nutrition. Research journals refused his papers. He was talked about by fellow scientists as an eccentric, a lone obsessive. Eventually, he became a scare story … . ‘They took him down so severely — so severely — that nobody wanted to attempt [similar research] on their own’… . He died, in 1995, a disappointed, largely forgotten man” (54).
I suspect Yudkin’s destruction was aided by a 1970 publication (55) by the man who at the time was considered scientifically untouchable because he had proved the link between cigarette consumption and lung cancer, Sir Richard Doll (56).
In that 1970 publication, Doll and colleagues argued “cigarette smokers … drink more tea and coffee” (55, p. 1013). Since there is “a close association between the number of cups of hot drinks consumed daily and the intake of sugar” then, quite obviously, “it is cigarette smoking and not sugar consumption which is implicated in the aetiology and manifestation of myocardial infarction” (p. 1011).
Recall for the moment that in his untouchable position, Doll was an obvious target for industries wishing to find scientists prepared to “health-wash” their products — naturally, at a richly rewarding price. It is now established that Doll served as a consultant for the chemical companies Monsanto, Dow Chemicals, and ICI, during which time he provided “expert” evidence that their chemicals did not cause cancer (57, 58). He was very well remunerated for this work.
This happened at the very time the sugar industry had embarked “on a major program (to counter Yudkin and other) negative attitudes towards sugar” (59, p. E2). This included paying for a review article by Harvard nutritional scientists that essentially absolved sugar of any proven role in the causation of CHD. When published, the paper did not disclose the authors’ conflicts of interest, failing to mention they had been paid by the sugar industry to write the article and arrive at conclusions that would help exonerate sugar from any role in the CHD epidemic.
Is it at all possible that the sugar industry reached out only to Harvard for help with their “Yudkin” problem? Or did they perhaps also approach Doll, who worked across the Atlantic in the cloistered seclusion of one of England’s two greatest universities?
In the end, Keys’ own work would provide the best evidence that sugar was involved. Data from the Seven Countries Study found that, of 21 different foodstuffs, the category labeled “sweets” had the second strongest association with CHD mortality (60). What irony!
More criticisms of the manner in which Keys chose the countries for his studies
More recently, P. D. P. Wood (61) has analyzed the validity of Keys developing a hypothesis based on data from a few handpicked countries. He showed that when Keys finally selected the seven countries for his Seven Countries Study (28), his choice came from the 21 member states of the Organization of Economic Cooperation and Development. When categorized by the amount of visible animal fat eaten each day in those 21 countries, the data fell neatly into two distinct groups: Six countries in which daily consumption of visible fat was lower than ~5 grams/day and the remaining 15 in which the intake was greater than 9 grams/day (Figure 6).
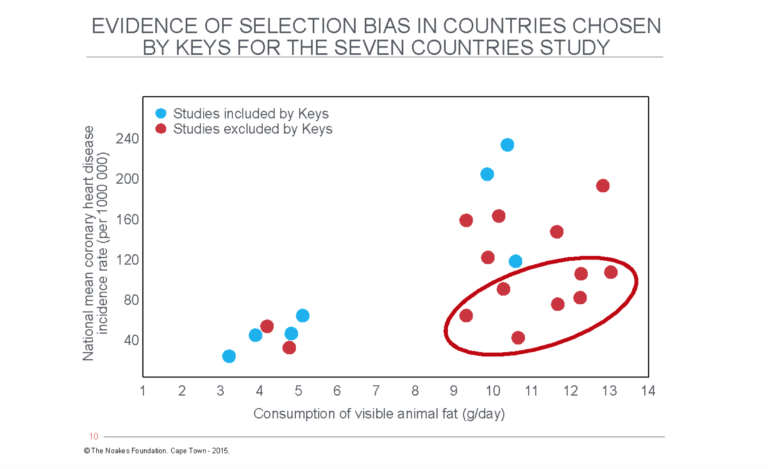
Figure 6: Wood (61) found the countries studied by Keys in his Seven Countries Study (28) fell into two distinct groups when categorized by the amount of visible animal fat eaten each day. Had Keys selected data from fewer countries with low rates of visible animal fat intake, he would not have been able to (mis-)represent such an apparently clear association between fat intake and coronary heart disease rates. The circled countries are those with high rates of fat intake but lower rates of heart disease. Keys excluded these from his study. Reproduced from reference 61.
Wood’s thesis was that Keys selected four of the six (67%) countries with low fat intakes but only three of the 15 (20%) with high fat intakes. Wood did not notice Keys also chose to exclude seven countries with high rates of fat intake but lower levels of heart disease (circled).
Using statistical methods, Wood established that if Keys included fewer of the countries with low fat intake in his final analysis, the probability that he would find any significant correlations fell sharply. Thus: “It seems probable therefore that the Seven Countries Study suffered from a selection effect of some magnitude. It is prudent whenever very small samples are offered as evidence of a hypothesis to make sure that they are fully representative of the population from which they are drawn” (61, p. 134-135).
K. D. Pett and colleagues (62) have recently presented detailed evidence that the countries for the Seven Countries Study were chosen for practical reasons. They argue Keys did not choose only those countries he knew beforehand would produce the outcomes he desired. Their argument appears reasonable.
However, this is much like the declaration of a conflict of interest by researchers wishing to distance themselves from any possible influence from their research funders.
Declaring a conflict of interest does not cause that conflict suddenly to disappear. The practical reasons why Keys may have chosen to study these seven countries does not suddenly negate the serious flaws identified by Wood.
The selection produced a biased sample of countries for study. It was not a random selection. All the results of the study will therefore be influenced by that bias.
Keys continues to collect evidence from population-based, associational, epidemiological studies
Yerushalmy and Hilleboe’s criticism of Keys’ ideas focused only on one aspect of the diet-heart hypothesis; that is, that high-fat diets cause coronary heart disease. Keys had yet to publish any population-based studies showing the second requirement of that hypothesis: specifically, that elevations in blood cholesterol concentrations induced by dietary fat explain why persons living in countries known to eat more fat suffer from higher rates of coronary heart disease.
Keys’ next studies (63-65) were the first (before the Seven Countries Study (28)), in which he reported real data in the collection of which he had been personally involved and which specifically addressed that component of the diet-heart hypothesis.
In one study, Keys’ team measured blood cholesterol concentrations in three different ethnic groups in my hometown, Cape Town, South Africa (65). In the other two studies, similar measurements were taken in persons living in Madrid, Spain (63), and Naples, Italy (64).
The study in South Africa showed blood cholesterol concentrations were higher in the more well-to-do citizens of European descent in Cape Town who also ate more animal fat than did those of African or mixed ancestry. These differences mirrored differences in heart disease rates in the three groups, being highest in those of pure European descent, least in those of pure African descent, and intermediate in the group of mixed ancestry. The authors concluded, “The results of this study support the hypothesis that the dietary intake of fat influences the level of the serum cholesterol, particularly that in the lipoprotein, and in turn may be one of the major factors influencing the pathogenesis of coronary heart-disease” (65, p. 1107, my emphasis).
At least in 1955, the year his “scientific” diet was prescribed for the management of President Eisenhower, Keys and his University of Cape Town co-authors acknowledged these dietary ideas were still just hypothetical and no more.
But Keys’ conclusion continues to ignore the central weakness in all epidemiological associational (observation) studies, which he knew all along (25) and which was again emphasized in his wrangle with Yerushalmy and Hilleboe — specifically, that the three different population groups differ in a host of other ways, not just in their diets. Indeed, the only justification for assuming diet alone explains these differences is if one begins with the conclusion that diet alone determines these differences. We call this model-dependent reality (66). It seems Keys was not aware his conclusions were pre-determined by what he desperately wanted to be true.
One might add that once Keys’ hypothesis had been accepted as fact by influential people like Eisenhower and White, who had influence over the American Heart Association (AHA) and the National Heart Lung and Blood Institute (NHLBI) (40), there was no going back. That particular horse had already bolted.
Sixty-six years later, Keys’ unproven hypotheses are still galloping merrily along, seemingly unconstrained by a mountain of evidence that disproves them.
Keys publishes another iconic graph to support his emerging hypotheses
Keys’ next study (27), which was published in 1957, was a work in progress at the time of Eisenhower’s heart attack. With its publication, Keys hoped to complete the evidence needed to secure his diet-heart hypothesis as irrefutably true.
He began by stating an incontrovertible fact: The incidence of heart disease differs substantially in different populations around the globe. What could possibly explain this difference in susceptibility?
Conveniently, Keys provided a partial answer to his rhetorical question by telling us what the causes cannot be:
It is easy to rule out of primary consideration many factors that show no consistency with regard to the relative frequency of the disease. Climate, race, the use of alcohol and tobacco, degree of urbanization and industrialization, the stress forces of exposure to telephones, radios, street traffic hazards, personal cleanliness and sports, availability of doctors and hospitals seem to fall in this category; any or all of these may exert some influence but, if so, it would seem to be minor and secondary to other and more basic factors. (27, p. 1522)
Instead, the cause is obvious, according to Keys in 1957; it is solely differences in blood cholesterol concentrations caused by differences in the amount of animal fat in the diets of populations with different rates of coronary heart disease. All else can, henceforth, be conveniently ignored. In effect, Keys was signaling that he had crossed a threshold. He “knew,” perhaps as a result of some divine intercession, that his twin hypotheses were true; he needed no further evidence. His responsibility was no longer to good and honorable science.
Rather, it had become his responsibility to convince the rest of the world that they should share his convictions — without skepticism, without questioning, and in the absence of definitive proof.
Thus, he and his colleagues wrote:
An important connection between the cholesterol-lipoprotein system in the blood and the production of atherosclerosis in man has long been recognized from innumerable demonstrations of a tendency for the serum cholesterol to be high in persons with recognized coronary heart disease and of the fact that persons suffering from other diseases characterized by elevated serum cholesterol values — myxedema, diabetes, nephrosis, xanthomatosis, familial hypercholesterolemia — are unusually prone to develop coronary heart disease. Recently it has been shown that even single serum cholesterol measurements on American men who are apparently clinically “healthy,” have prognostic value in regard to the subsequent development of unequivocal signs of coronary heart disease. (p. 1522, my emphasis)
They continued: “And the work of recent years has increasingly shown the dominant influence of the diet of man as well as of animals on the cholesterol-lipoprotein system of the blood” (p. 1523, my emphasis). They then wrote that controlled human experiments have little relevance “to normal life” (p. 1523), so the best way to investigate the relationship between diet and coronary atherosclerosis is “the study of the natural dietary experiments of human populations and the associated experiences of atherosclerosis and coronary heart disease. This is the epidemiological approach which we wish to emphasize here” (p. 1523).
They next provided evidence that different populations have different rates of coronary heart disease before explaining to their readers why this is so:
Since, experimentally, the closest connection exists between diet and atherogenesis, it is reasonable to examine the diets of populations differing in the frequency of atherosclerosis and coronary heart disease. And since a major connection between the diet and the disease seems to be through the serum cholesterol concentration, we must keep this variable in mind. It will be seen that the incidence of coronary heart disease seems to be related to the proportion of fat in the habitual diet, and this fact is in general agreement with the theory (actually hypothesis – my addition) that atherosclerosis is usually primary in coronary heart disease and that atherosclerosis is promoted by the cholesterol-lipoprotein in the blood which, in turn, is strongly influenced by the fat content of the diet. (p. 1526, my emphasis)
Keys is clearly guilty of the behavior about which Yerushalmy and Hilleboe had warned us in 1957: “But quotation and repetition of the suggestive association soon creates the impression that the relationship is truly valid, and ultimately it acquires status as a supporting link in a chain of presumed proof” (33, p. 2343, my emphasis).
The point of all this is, as Teicholz asserts, that in science, one is meant first to present the evidence and then explain what one’s findings mean. The “science” Keys had begun to practice in 1957 was the polar opposite. After 1957, he informed us what his “science” was going to find and why. And then he set out to provide us with the “evidence” he believed would miraculously turn his hypotheses into established fact.
Keys next presented results from 21 groups of men aged 40-49 years in whom blood cholesterol concentrations were measured and the fat content of the diet was estimated. The study included the data from Keys’ three previous studies (62-64). The primary finding, as presented by Keys, is shown in Figure 7. A subsequent figure, published the following year (1958) and including data for 1,288 men aged 40-49, appeared even more impressive since the data fitted even more closely to a perfect linear relationship (67, p. 88).
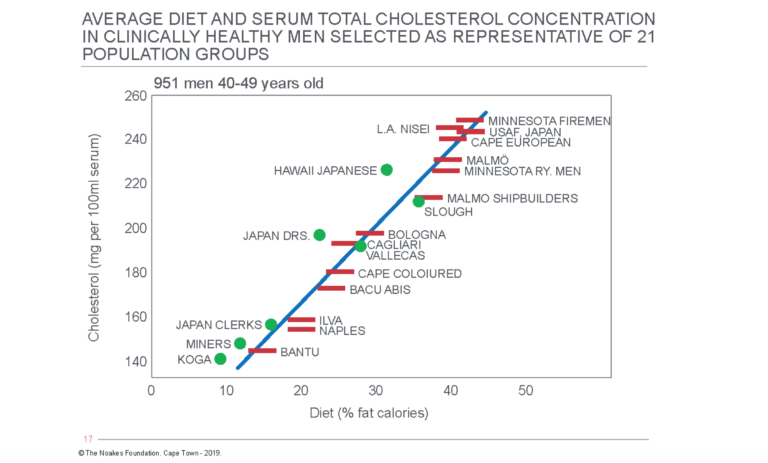
Figure 7: Keys’ 1957 publication (27) included this figure showing the average blood cholesterol concentrations and average fat-calorie percentages in the diets of “clinically healthy men selected as representative of 21 population groups.” Again, Keys provided a neat relationship between the variables he decided were the most important. Reproduced from reference 27.
As I examined this figure, I began to marvel at how, in the early 1950s, Keys was able to measure with such extreme precision, the different fat intakes in the different populations. For example, he was able to show that in the diet of South African Bantu, 12% of the calories came from fat, while fat provided 22% of the calories consumed by mixed ancestry South Africans (“Cape Coloured”). He also claimed this 10% difference in daily fat intake produced an increase of about 40 mg/100 ml in blood cholesterol concentrations. The specificity of these determinations is quite remarkable.
In their Cape Town paper, Keys and colleagues described how they measured dietary fat intake: “The nature of each person’s diet was assessed, particularly as regards consumption of fat-containing foods. The intake of fat was further subdivided into that from animal and that from vegetable sources. Figures denoting the degree of consumption of fat can be regarded as semi-quantitative only because it was assumed that each person consumed an ‘average’ helping” (65, p. 1104, my emphasis). The report for the study from Naples (64) also included no intelligible explanation of how these dietary data were collected and analyzed. The study of the Madrid families included this statement: “The method of dietary survey by families in Vallecas did not allow precise estimation of the diets of the individuals, but it appeared that there were no systematic differences between men of different ages that the proportion of dietary fat in the diet was fairly uniform within each family” (63, p. 197).
To calculate fat-calorie percentage intake, one needs an accurate measure of total caloric intake. Yet the authors provided no explanation of how that value was derived.
I think one can conclude with a high degree of certainty that the numbers for the fat-calorie percentages on the x-axis of Figure 7 are little better than guesswork. This would help explain why there is such a neat linear relationship in the figure between fat intake and serum cholesterol concentrations in these 21 different populations.
Recall that Figure 1 also shows a similarly neat relationship between two variables.
Perhaps Keys enjoyed presenting his evidence as neatly as possible (8, 27), since he might have believed that doing so would make his hypotheses more credible (Figures 1 and 7).
Once Keys had produced the data for Figure 7, he was able to convince first himself and then almost everyone else in the rest of the world (at least for the next 70 years) that the sole determinant of the blood cholesterol concentration is the percentage of the dietary calories derived from fat (68).
And when he combined Figure 7 with Figure 1, he probably assumed he now had all the “evidence” needed to prove elevated blood cholesterol concentrations are the sole cause of the coronary heart disease epidemic.
Keys argued the sole explanation for differences in coronary heart disease rates between different countries was that all the citizens in countries with high rates of heart disease, such as America, Australia, and Canada, have high blood cholesterol concentrations because every citizen in those countries eats a diet too rich in animal fat. The converse applies in countries with low rates of coronary heart disease. There is no other possible explanation.
Of course, this cannot explain why the majority of persons living in countries with high heart disease rates do not actually ever develop heart disease, even if they have high blood cholesterol concentrations and eat fat-rich diets.
Keys concluded his 1957 paper with yet another restatement of his hypothesis as proven fact:
It seems probable that the more common fats of the American diet, when eaten in large amounts as is often the case in the United States, may contribute to the production of relative hypercholesterolemia and so to atherogenesis. Further, there is suggestive evidence that fatty meals may induce hypercoagulability of the blood and inhibition of fibrinolysis … . While dietary fat cannot be the sole responsible agent, the weight of accumulating evidence is such that the most extensive research on the question of the role of dietary fat in atherogenesis and thrombogenesis is warranted. (27, pp. 1529-1530)
Probably, he should have added: “… provided it supports my diet-heart and lipid hypotheses.”
That these ideas are still dominant in the teaching and practice of cardiology and nutrition across the globe indicates the lasting influence of these original and deeply simplistic studies by Keys. Generally, the assumption is that Keys provided “irrefutable evidence” to support his twin hypotheses (68).
Summary
In this and the previous column, I reviewed the evidence that Keys had published by 1957, two years after his experimental low-fat, low-cholesterol, high-carbohydrate diet had been prescribed to President Eisenhower, ostensibly to protect the president from any further heart attacks (2).
I showed the evidence he had presented by 1957 was purely associational and circumstantial and was derived from multiple sources. The original study (8), which was perhaps his most influential at the time (because it was the foundation upon which he built his scientific empire), comprised what we now refer to as “armchair science.” Keys did not need to venture from his living room to do the “research.” He simply collected some generally available information in a WHO document (Figure 2) that appealed to him, found an associational relationship between the two variables he fancied (Figure 1), and described what he personally thought it all meant. In this way, he began a process in which his own personal belief became perpetuated, over the years, as proven fact.
Because they were purely associational studies, none of Keys’ original studies could ever prove causation — and Keys knew this. In 1952, he (25) accused Malmros (11) of falIing into that very same intellectual trap, a trap about which Mann would later write, “The naiveté of such an interpretation of associated attributes is now a class-room demonstration” (69, p. 644).
In the course of normal science, Keys’ pretense of proof of causation should have been rejected for all the reasons presented by Yerushalmy and Hilleboe (33).
In the next three columns, I analyze the remaining studies Keys undertook during his academic career. I attempt to explain how and why, instead of being rejected, Keys’ unproven hypotheses were warmly received and enthusiastically embraced by the global medical profession, even as Keys collected evidence that clearly refuted both his hypotheses.
Nevertheless, the desire of many leading scientists and cardiologists to be part of a global herd embarking on a great “scientific adventure in cardiovascular disease epidemiology” (28) and all eager to accept and promote this exciting scientific “breakthrough,” suppressed any urge for skepticism about Keys’ unproven hypotheses.
Their lack of skepticism and eagerness to conform had grave consequences, not least because the unquestioning acceptance of Keys’ hypotheses opened the doors for different industries to produce and promote foods considered to be heart-healthy; or develop pharmaceutical drugs to lower blood cholesterol concentrations in order to prevent and reverse heart disease.
ADDITIONAL READING
- It’s the Insulin Resistance, Stupid: Part 1
- It’s the Insulin Resistance, Stupid: Part 2
- It’s the Insulin Resistance, Stupid: Part 3
- It’s the Insulin Resistance, Stupid: Part 4
- It’s the Insulin Resistance, Stupid: Part 5
- It’s the Insulin Resistance, Stupid: Part 6
Professor T.D. Noakes (OMS, MBChB, MD, D.Sc., Ph.D.[hc], FACSM, [hon] FFSEM UK, [hon] FFSEM Ire) studied at the University of Cape Town (UCT), obtaining a MBChB degree and an MD and DSc (Med) in Exercise Science. He is now an Emeritus Professor at UCT, following his retirement from the Research Unit of Exercise Science and Sports Medicine. In 1995, he was a co-founder of the now-prestigious Sports Science Institute of South Africa (SSISA). He has been rated an A1 scientist by the National Research Foundation of SA (NRF) for a second five-year term. In 2008, he received the Order of Mapungubwe, Silver, from the President of South Africa for his “excellent contribution in the field of sports and the science of physical exercise.”
Noakes has published more than 750 scientific books and articles. He has been cited more than 16,000 times in scientific literature and has an H-index of 71. He has won numerous awards over the years and made himself available on many editorial boards. He has authored many books, including Lore of Running (4th Edition), considered to be the “bible” for runners; his autobiography, Challenging Beliefs: Memoirs of a Career; Waterlogged: The Serious Problem of Overhydration in Endurance Sports (in 2012); and The Real Meal Revolution (in 2013).
Following the publication of the best-selling The Real Meal Revolution, he founded The Noakes Foundation, the focus of which is to support high quality research of the low-carbohydrate, high-fat diet, especially for those with insulin resistance.
He is highly acclaimed in his field and, at age 67, still is physically active, taking part in races up to 21 km as well as regular CrossFit training.
References
- Keys A, Keys M. Eat Well and Stay Well. Garden City, NY: Doubleday and Company, Inc., 1963.
- Noakes TD. It’s the insulin resistance, stupid: Part 5. CrossFit.com. 22 October 2019. Available here.
- White PD. Heart Disease, 3rd ed. New York, NY: The Macmillan Company, 1946.
- Keys A, Brozek J, Henschel A, et al. The Biology of Human Starvation. Minneapolis, MN: University of Minnesota Press, 1950.
- Olszewski TM. The causal conundrum: The diet-heart debates and the management of uncertainty in American Medicine. J Hist Med Allied Sci. 70(2014): 218-249.
- Keys A, Taylor HL, Blackburn H, et al. Coronary heart disease among Minnesota business and professional men followed fifteen years. Circulation 28(1962): 381-394.
- Smalley A. St. Paul Pioneer Press, October 11, 1949. In: Henry Blackburn reviews 1938-1955 albums of Laboratory of Physiological Hygiene news reports as now preserved on CDs in the Division of Epidemiology and in University Archives. Available here.
- Keys A. Atherosclerosis: A problem in newer public health. J Mt Sinai Hosp. 20(1953): 118-139.
- Taubes G. Good Calories, Bad Calories: Fats, Carbs, and the Controversial Science of Diet and Health. New York, NY: Anchor Books, 2008.
- Keys A, Anderson JT. The relationship of the diet to the development of atherosclerosis in man. In: Symposium on atherosclerosis. National Academy of Sciences – National Research Council Publication 338. Washington, D.C.: 1954. pp. 181-197.
- Malmros H. The relation of nutrition to health. A statistical study of the effects of the war-time on arteriosclerosis, cardiosclerosis, tuberculosis and diabetes. Acta Med Scand Suppl. 246(1950): 137-53.
- Pihl A. Cholesterol studies. II. Dietary cholesterol and atherosclerosis. Scan J Clin Lab Invest. 4(1954): 122-133.
- Strom A, Jensen AR. Mortality from circulatory diseases in Norway 1940-45. Lancet 260(1951): 126-129.
- Henschen F. Geographic and historical pathology of arteriosclerosis. J Gerontol. 8(1953): 1-5.
- Strom A. Examination of the diet of Norwegian families during the war years 1942-1945. Acta Med Scand. 131 suppl. 214(1948): 1-47.
- Vartainen I, Kanerva K. Arteriosclerosis and war-time. Ann Med Intern Fenn. 36(1947): 748-758.
- Gofman JW, Jones HB, Lindgren FT, et al. Blood lipids and human atherosclerosis. JAMA 11(1950): 161-178.
- Jones HB, Gofman JW, Lindgren FT, et al. Lipoproteins in atherosclerosis. Am J Med. 11(1951): 358-380.
- Gofman JW. Diet and lipotrophic agents in atherosclerosis. Bull NY Acad Med. 28(1952): 279-293.
- Gofman JW, Glazier F, Tamplin A, et al. Lipoproteins, coronary heart disease and atherosclerosis. Physiol Rev. 34(1954): 598-607.
- Gofman JW, Tamplin A, Strisower B. Relation of fat intake to atherosclerosis. J Am Diet Assoc. 30(1954): 317-326.
- Lyon TP, Yankley A, Gofman GW, et al. Lipoproteins and diet in coronary heart disease. A five-year study. Cal Med. 84(1956): 325-328.
- Levenstein H. Fear of Food. A History of Why We Worry About What We Eat. London, U.K.: University of Chicago Press, 2012.
- Keys A. The inception and pilot surveys. In: Kromhout D, Menotti A, Blackburn H. The Seven Countries Study. A scientific adventure in cardiovascular disease epidemiology. Marjan Nijssen-Kramer, Studio RIVM, Bilthoven, The Netherlands, 1993. pp. 15-25. Available here.
- Keys A. Human atherosclerosis and the diet. Circulation 5(1952): 115-118.
- Keys A. Prediction and possible prevention of coronary disease. Am J Publ Health 1953: 1399-1407.
- Keys A, Grande F. Role of dietary fat in human nutrition. III – Diet and the epidemiology of coronary heart disease. Am J Pub Health 47(1957): 1520-1530.
- Kromhout D, Menotti A, Blackburn H. The Seven Countries Study. A scientific adventure in cardiovascular disease epidemiology. Marjan Nijssen-Kramer, Studio RIVM, Bilthoven, The Netherlands, 1993. Available here.
- Teicholz N. The Big Fat Surprise: Why Butter, Meat and Cheese Belong in a Heathy Diet. New York, NY: Simon and Schuster, 2014.
- Harcombe Z. An examination of the randomized controlled trials and epidemiological evidence for the introduction of dietary fat recommendations in 1977 and 1984: A systematic review and meta-analysis. Ph.D. thesis, University of West Scotland, March 2016.
- Keys A. “Giant molecules” and cholesterol in relation to atherosclerosis. Bull J Hopkins Hosp. 88(1951): 473-483.
- Keys A. Cholesterol, “Giant molecules” and atherosclerosis. JAMA 147(1951): 1514-1519.
- Yerushalmy J, Hilleboe HE. Fat in the diet and mortality from heart disease. A methodological note. New Y State J Med. 57(1957): 2343-2354.
- Mann GV. A short history of the diet/heart hypothesis. In: Coronary Heart Disease. The Dietary Sense and Nonsense. An Evaluation by Scientists. London, England: Janus Publishing Company, 1993. pp. 1-17.
- Mann GV. Diet and coronary heart disease. Arch Intern Med. 104(1959): 921-929.
- “Medicine: The Fat of the Land.” Time Magazine. 1961 Jan. 13. Available here.
- Subbotin VM. Excessive intimal hyperplasia in human coronary arteries before intimal lipid depositions is the initiation of coronary atherosclerosis and constitutes a therapeutic target. Drug Dis Today 21(2016): 1578-1595.
- Stehbens WE. The pathology of atherosclerosis. In: Coronary Heart Disease. The Dietary Sense and Nonsense. An Evaluation by Scientists. Mann GV, ed. London, England: Janus Publishing Company, 1993; pp. 18-27.
- Kealey T. Why does the federal government issue damaging dietary guidelines? Lessons from Thomas Jefferson to today. Policy Analysis 10 July 2018. Available here.
- Noakes TD. It’s the insulin resistance, stupid: Part 10. (forthcoming on CrossFit.com)
- Keys A. Epidemiological aspects of coronary artery disease. J Chron Dis. 6(1957): 552-559.
- Ahrens EH, Hirsch J, Insull W, et al. Dietary control of serum lipids in relation to atherosclerosis. JAMA 164(1957): 1905-1911.
- Noakes TD. It’s the insulin resistance, stupid: Part 1. CrossFit.com. 6 July 2019. Available here.
- Ahrens EH. Dietary fats and coronary heart disease: Unfinished business. Lancet 314(1979): 1345-1348.
- Ahrens EH. The diet-heart question in 1985: Has it really been settled. Lancet 1(1985): 1085-1087.
- Ahrens EH. The evidence relating six dietary factors to the Nation’s health. Introduction. Am J Clin Nutrition 32(1979): 2627-2631.
- S. Senate Select Committee on Nutrition and Human Needs. Dietary Goals for the United States, 2nd ed. Washington, DC, U.S. Government Printing Office, 1977. (See also https://health.gov/dietaryguidelines/dga2005/report/PDF/G5_History.pdf).
- American Heart Association Committee Report. Circulation 58(1978): 762-765.
- Yudkin J. Diet and coronary thrombosis. Hypothesis and fact. Lancet 273(1957): 155-162.
- Yudkin J. Dietary fat and dietary sugar in relation to ischaemic heart disease and diabetes. Lancet 2(1964): 4-5.
- Yudkin J, Roddy J. Levels of dietary sucrose in persons with occlusive atherosclerotic disease. Lancet 2(1964): 6-8.
- Yudkin J, Morland J. Sugar intake and myocardial infarction. Am J Clin Nutr. 20(1967): 503-506.
- Keys A. Sucrose in the diet and coronary heart disease. Atherosclerosis 14(1971): 193-202.
- Leslie I. The sugar conspiracy. The Guardian 7 April 2016. Available here.
- Bennett AE, Doll R, Howell RW. Sugar consumption and cigarette smoking. Lancet 1(1970): 1011-1014.
- Petro R, Darby S, Deo H, et al. Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies. BMJ 321(2000): 323-329.
- Tweedale G. Hero or villain?—Sir Richard Doll and occupational cancer. Int J Occup Environ Health 13(2007): 233-235.
- Boseley S. Renowned cancer scientist was paid by chemical for 20 years. The Guardian. 8 Dec. 2006. Available here.
- Kearns CE, Schmidt LA, Glantz SA. Sugar industry and heart disease research. A historical analysis of internal industry documents. JAMA Internal Medicine 176(2016): 1680-1685.
- Menotti A, Kromhout D, Blackburn H, et al. Food intake patterns and 25-year mortality from coronary heart disease: Cross-cultural correlations in the Seven Countries Study. Europ J Epidemiol. 15(1999): 507-515.
- Wood PDP. A possible selection effect in medical science. J Roy Stat Soc. 30(1981): 131-135.
- Pett KD, Kahn J, Willett WC, et al. Ancel Keys and the Seven Countries Study: An evidence-based response to revisionist histories. White Paper commissioned by the True Health Initiative. 1 Aug. 2017. Available here.
- Keys A, Vivanco F, Minon JLR, et al. Studies on the diet, body fatness and serum cholesterol in Madrid, Spain. Metabolism 3(1954): 195-212.
- Keys A, Fidanza F, Scardi V, et al. Studies on serum cholesterol and other characteristics of clinically healthy men in Naples. Arch Int Med. 93(1954): 328-336.
- Bronte-Stewart B, Keys A, Brock JF, et al. Serum-cholesterol, diet, and coronary heart-disease. An inter-racial survey in the Cape Peninsula. Lancet 269(1955): 1103-1107.
- Noakes TD. 1996 JB Wolffe Memorial Lecture. Challenging beliefs: ex Africa semper aliquid novi. Med Sci Sports Exerc. 29(1977): 571-590.
- Keys A, Kusukawa, Bronte-Stewart B, et al. Lessons from serum cholesterol studies in Japan, Hawaii and Los Angeles. Ann Intern Med. 48(1958): 83-94.
- Mayosi BM, Forrester T. Commentary: “Serum-cholesterol, diet, and coronary heart-disease in Africans and Asians in Uganda” by AG Shaper and KW Jones. Int J Epidemiol 41.5(2012): 1233-1235.
- Mann GV. Diet-heart. End of an era. N Engl J Med. 297(1977): 644-650.
It's the Insulin Resistance, Stupid: Part 7