President Eisenhower prescribed experimental, untested low-fat, low-cholesterol diet
It is Friday, Sept. 23, 1955. The 64-year-old 34th President of the United States Dwight D. Eisenhower is on a “work and play” vacation in Denver, Colorado (1-4). As required for work, he travels to the Lowry Air Force Base in eastern Denver; for play, he either fishes at the Byers Peak Ranch in the Rocky Mountains or plays golf on any of the many courses in the Denver area. Eisenhower is a compulsive golfer. During his eight years as president, he completes 800 rounds of golf; he plays off a handicap of 13-17.
On this day, Eisenhower plays on the Cherry Hills Golf Club in southern Denver. He completes 18 holes and then lunches on a hamburger and Bermuda onions before playing another nine holes, during which he complains of some abdominal discomfort. He decides not to play the final nine holes and returns home. He eats dinner with his wife and another couple and retires to bed at 10 p.m.
At about 1:30 a.m. on Saturday morning, he is awakened by severe chest pain, which he ascribes to his injudicious lunch at the golf club. He asks his wife for some milk of magnesia. She detects an anxiety in her husband that she finds worrying. After one look, she decides to call the White House physician, Maj. Gen. Howard Snyder, who arrives at 2:00 a.m. Snyder does not initially consider a diagnosis of acute myocardial infarction (heart attack), in part because Eisenhower has a long history of recurrent attacks of abdominal pain, later diagnosed as Crohn’s disease. Snyder likely assumes this is just another such attack. He administers morphine, which allows the president to sleep until mid-morning.
When the president finally awakens at 11 a.m., he again complains of chest pain. Now concerned that the president may have suffered a heart attack, Snyder requests two colleagues from the Fitzsimmons General Hospital to bring an electrocardiogram to the president’s bedside. The electrocardiogram they record confirms the president has suffered an acute anterolateral myocardial infarction. He is transferred to the Fitzsimmons General Hospital, where he is admitted at about 3:00 p.m.
Some time that same afternoon, Col. Thomas W. Mattingly, who is Chief of Cardiology at the Walter Reed Hospital and Chief Consultant in Cardiology to the Surgeon General of the Army, is asked to come without delay to Denver to assist in the management of the president’s heart attack. His flight, delayed and diverted by a rainstorm, causes him to arrive at midnight. He immediately examines the patient.
While all this is happening on Saturday afternoon, Vice President Richard Nixon suggests it would be prudent for a civilian heart specialist to be called in “because we cannot overlook the fact that many people in the country may have more confidence, however unfounded, in a civilian specialist of national reputation” (4, p. 1205).
The consensus is soon reached that Dr. Paul Dudley White of Boston’s Massachusetts General Hospital is the most qualified civilian to support the military cardiologists. White is one of America’s, and indeed the world’s, most eminent cardiologists. At the time, his textbook forms the basis for the teaching of cardiology globally (5).
That same afternoon, White is invited to attend to the president. He catches a plane to Denver on Sunday morning, arriving at 1:10 p.m. He examines the patient and confirms the heart attack diagnosis. He informs the president that he will need to rest in bed for the next two to three weeks, be prescribed a “light diet,” and given Coumadin to prevent blood clotting and quinine to prevent irregularities of heart rhythm (3).
Following White’s examination of the president, a bulletin is released to the media at 4:12 p.m. It states, “The President has had a moderate attack of coronary thrombosis, without complications. His present condition is satisfactory” (3, p. 160).
White remains in Denver for just 24 hours. By leaving within such a short time, he wishes to signal his complete confidence in the competence of the military cardiologists attending the president. He will continue, on and off, as a consultant to Drs. Snyders and Mattingly until the president’s death in 1969.
The Challenges
In the face of global scrutiny (and a collapsing New York Stock Exchange that in response to the president’s heart attack sheds $14 billion (6%) on Monday, Sept. 26 (4)), the challenges faced by Eisenhower’s medical team (Figure 1) are staggering. Given the knowledge of coronary heart disease at the time and the treatment options available to them, they achieve a successful outcome.
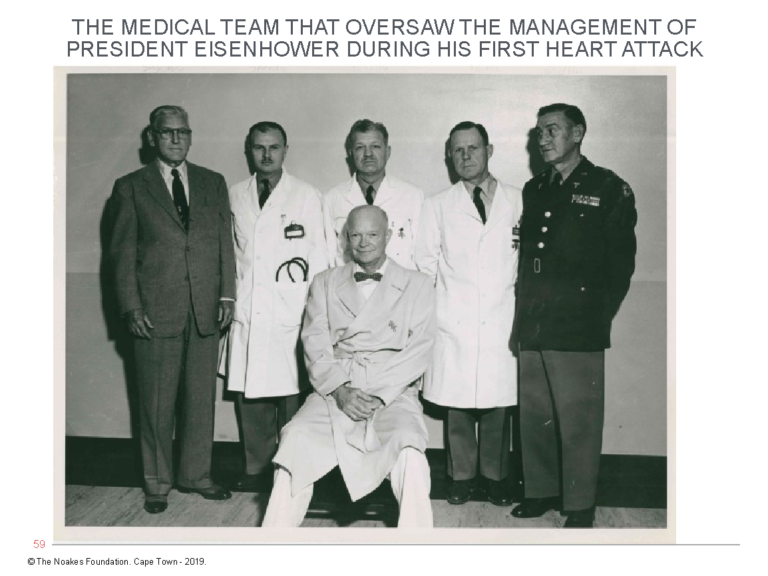
Figure 1: The medical team that oversaw the management of President Eisenhower during his first heart attack in September 1955. President Eisenhower sits with (from left to right) Maj. Gen. Howard Snyder, Lt. Col. John Sheedy, Col. Byron Pollock, Col. George Powell, and Maj. Gen. Martin Griffin. Neither Dr. Paul Dudley White nor Col. Thomas W. Mattingly was present for this photograph.
Not only do they ensure that Eisenhower does not die during the acute phase of the illness, but they help him recover sufficiently to fight a successful presidential re-election campaign in 1956, during which he becomes one of the most popular presidents in U.S. history. In addition, he lives another 14 years after his first heart attack, dying at age 78.
The downside is that during those 14 added years, Eisenhower is plagued by a range of chronic diseases. He suffers a cerebral stroke and a further six heart attacks. He also requires surgery for Crohn’s disease and the removal of his gallbladder (2).
His life is also extended by the timeous development of the cardiac defibrillator by another iconic U.S. cardiologist, Dr. Bernard Lown, in 1962 (6). (Lown is remembered as a medical maverick (7) because he saw little benefit from and actively campaigned against widespread coronary artery bypass grafting for the management of coronary atherosclerosis. His studies (8-11) established that medical management of persons with coronary artery disease and myocardial infarction is just as effective as coronary artery bypass surgery, without the added risks of operation-induced cognitive deficits (12)). Coronary artery bypass grafting is not offered as an option to the president simply because the operation had yet to be developed; the first such operation is performed in 1961 (13).
On 14 occasions, the Lown defibrillator instantly reverses the president’s aberrant heart rhythm, restoring the heart’s output and saving his life.
But during the final year of his life, Eisenhower’s heart functions with barely any blood supply, so severe is the coronary atherosclerosis that strangles his heart. He dies in intractable heart failure.
The autopsy report on the president confirms his coronary arteries show “atherosclerotic occlusive disease, multifocal, severe, with multiple recanalized thrombi” (2, p. 321). Of the three major coronary arteries, only the right coronary artery is patent; the left anterior descending coronary artery has 10% narrowing in various sections; his circumflex artery is totally obstructed in several sections.
In retrospect, it is difficult to avoid the conclusion that whatever good the president’s advisers did in the short term to secure his survival, their long-term management did nothing to reverse the president’s inexorable slide into heart failure. In the end, the sole remaining treatment option is a heart transplant, the operation pioneered by Professor Christiaan Barnard in Cape Town on Dec. 3 or 4, 1967 (14).
But Eisenhower’s cardiologists decide his physical state, including, importantly, the presence of Type 2 diabetes mellitus (T2DM), makes the operation unthinkable (2, p. 314).
With the benefit of hindsight and our modern knowledge, it is difficult to avoid the conclusion that the dietary advice the president received from White contributed to his progression into heart failure.
I draw this conclusion from the evidence that the president developed T2DM in his later years, indicating he was insulin resistant at the time of his first heart attack.
Understandably, this was not diagnosed in 1955, since insulin resistance would only be properly described by Gerald Reaven in the 1980s (15). And only very recently has it been established that the diet the president was prescribed in 1955 should be considered as contraindicated for those with insulin resistance/pre-diabetes/T2DM (16).
This raises the question: What did White understand about the causes of heart disease when he was called to examine the president on Sept. 24, 1955?
The State of the research in 1955
To understand what was known about coronary heart disease, its pathology, and its management in 1955, our best source is the cardiology textbook that was the global standard at the time — the one written by White himself.
The third edition of his iconic textbook Heart Disease, published in July 1946 (5), defines how White understood coronary artery disease when he was summoned to Eisenhower’s bedside on Sept. 25, 1955.
White believed atherosclerosis is “but part and parcel of the process of growing old” (5, p. 475). Although in this edition of his textbook he wrote he was not convinced heart attacks had become more common in the “present generation,” an earlier edition of the textbook included the opposite: “When I graduated from medical school in 1911, I had never heard of coronary thrombosis, which is one of the chief threats to life in the United States and Canada today … . There can be no doubt but that coronary heart disease has reached epidemic proportions in the United States, where it is now responsible for more than 50 per cent of all deaths.”
Elsewhere, he had also said, “See here, I began my practice as a cardiologist in 1921 and I never saw an MI (myocardial infarction) patient until 1928” (17, p. 20).
In his textbook, White wrote that although coronary artery atherosclerosis, the underlying condition that causes heart attacks, had been described by Bonetus in 1700, the classic description of “sudden obstruction of the coronary arteries” (i.e., a heart attack) was first communicated by James Herrick in 1912 (18). Surprisingly, in keeping with the thoroughly modern (2012) and unquestionably “controversial” Subbotin hypothesis (19), White quoted evidence that the initiating event in atherosclerosis is “a simple thickening of the elastic hyperplastic layer of the (arterial) intima” (p. 478); for support he quoted the work of Timothy Leary (20), who argued “the lesions (associated with atherosclerosis) arise constantly in the intima, though late extension to the media may occur” (p. 475).
Of historical interest was that already in 1935, Leary had linked atherosclerosis to both diabetes and high blood cholesterol concentrations. Thus, Leary wrote, “The high sugar concentration and the great fluctuations in sugar concentration in the blood of persons with diabetes could possibly lead to swelling of the intimal ground substance through changes in osmotic pressure,” and, “The most striking evidence indicates that high blood cholesterol is the standard factor from the dietary standpoint in the causation of atherosclerosis” (p. 477). Leary provided no reference for the latter conclusion.
In an accompanying histological picture of a diseased coronary artery (facing p. 480), White provides pictorial evidence (as does Subbotin (19)) that the original injury in atherosclerosis occurs deep in the intimal lining of the affected arteries and not at the surface of the artery as it must if cholesterol is entering the arterial wall directly from the bloodstream.
Thus, White wrote: “Note the almost complete obstruction of the descending branch of the left coronary artery by the extensive intimal fibrosis with necrosis in the deepest layer … just overlying the media (muscular layer of the artery)” (p. 481, my emphasis).
On the basis of this histological evidence, it might have been reasonable for White to conclude that atherosclerosis begins as a result of events occurring within the wall of the coronary artery and is not caused by something (like “cholesterol”) entering the arterial wall directly from the bloodstream. But understandably, this logical inconsistency likely did not tax his mind, just as it has not worried generations of cardiologists and cardiac surgeons since (21).
White admitted he was uncertain of the factors driving the development of coronary atherosclerosis:
The cause of atheroma of the coronary arteries, as well as that of the arteriosclerosis in general, is unknown. Faulty cholesterol metabolism, local arterial strain or overwork, hypertension, infection, allergy, endocrinopathy, and heredity are among the many factors suggested, but none has been proven or even consistently found. The occasional finding of a high blood cholesterol content in fasting cases of coronary heart disease, especially in the young patient under 40, is in favor of a disturbance of fat metabolism, at least as one factor … . Serious coronary sclerosis relatively is more common in hypertensive individuals than in persons with normal blood pressure, the hypertension antedating any evidence of coronary disease; the frequency of coronary disease in myxedema (low thyroid states) and diabetes supports the idea of a factor of disturbed fat metabolism secondary to endocrinopathy; and the factor of heredity is supported by the frequent finding of several members of a single family with serious coronary sclerosis. The combination of several etiologic factors is plausible. (21, p. 479, my emphasis)
White also recognized the disease was much more common in men than women, and in certain ethnic groups. He also thought the disease is “much more often found in sensitive, mentally overworked, and frequently robust or stout professional and business men than in other individuals” (p. 482). “One has the distinct impression that it is distinctly less common in the lean laborer or farmer,” he added (p. 482).
White also postulated hereditary factors might act via diabetes and hypertension, and he wrote tobacco could aggravate the condition while “heavy indulgence in alcohol over many years appears to have a protective influence against the ill effects of coronary disease” (p. 482).
He believed optimism and hope were central to the management of chronic diseases like heart disease: “Without optimism the world would be a sorry place to live in. The natural or acquired ability to look on the bright side of things may easily mean the difference between happiness and unhappiness in any individual life” (3, p. 185).
In the president, he had a patient who understood the importance of optimism perhaps better than anyone else — for Eisenhower had successfully faced the ultimate challenge of leading one of the single greatest military expeditions in history: the D-Day landings in Normandy in June 1944.
As Fred Greenstein writes, during the darkest hours of World War II, Eisenhower had indeed written, “‘During those anxious hours I first realized … how inexorably and inescapably strain and tension wear away at the leader’s endurance, his judgement and his confidence. The pressure becomes more acute because of the duty of a staff constantly to present to the commander the worst side of any eventuality.’” Greenstein writes: “Realizing that the commander has the double burden of ‘preserving optimism in himself and in his command’ and ‘that optimism and pessimism are infectious and they spread more rapidly from the head down than in any direction,’ he made a firm resolution.” The president wrote:
I firmly determined that my mannerisms and speech in public would always reflect the cheerful certainty of victory — and any pessimism and discouragement I might ever feel would be reserved for my pillow. To translate this conviction into tangible results … I adopted a policy of circulating through the whole force to the full limit imposed by physical considerations … I did my best to meet everyone from general to private with a smile, a pat on the back and a definite interest in his problems. (22, p. 43)
Given this attitude, White must have welcomed the opportunity to treat the president. Would there ever be a better patient on whom White and others could practice their healing craft?
Knowledge of dietary factors that might cause coronary atherosclerosis
In 1946, White clearly did not consider that any specific dietary factors caused atherosclerosis. Certainly, he was not yet a dedicated promoter of any particular dietary therapy for the prevention or treatment of coronary atherosclerosis. Instead, his dietary advice was to follow “a limited diet to maintain a low basal metabolic rate.” This, he suggested, would aid in the healing of the heart attack, so he claimed “a light mixed diet of 1800 to 2100 calories in 4 or 5 small meals a day is a good plan” (p. 502). I suspect the goal of this diet prescription was simply weight loss.
So the conclusion is inescapable that at least in 1946, White was unconvinced diet was a major determinant of atherosclerosis. He would not have believed recent dietary changes were the single most important cause of the rising incidence of coronary heart disease in the United States and elsewhere.
And why should he have?
If a change in diet was the singular cause of the growing heart disease “epidemic” in the U.S. after 1928, surely White would have been among the first to notice that change? Logically, it would require a dramatic (and obvious) transformation in the U.S. diet between 1911 — when the disease was so uncommon it was not even mentioned in White’s medical training — and 1928 — when White treated his first heart attack patient. Surely, by the 1950s, when coronary heart disease had reportedly reached epidemic proportions, any possible dietary causes should have been obvious to all, and especially to an inquisitive and interested observer like White.
The question I pose in this and the subsequent column is: If this was indeed so, why, by 1955, had White changed his opinion so radically that he was prepared to put all his faith in an experimental and untested low-fat, low-cholesterol diet as the core component of the treatment for President of the United States?
The answer to that question is central to understanding how our current dietary advice was determined by factors happening in the mid- and late-1950s. Many of these factors involved both President Eisenhower and his key medical advisor, Paul Dudley White.
President Eisenhower’s medical team struggles
The immediate problem faced by the medical team deeply concerned about the president’s future health was, stated simply: What can we change now in the way he lives his life that will improve his prospects of surviving many more years without suffering any further heart attacks (or a stroke)?
The problem was that there did not seem to be much they could change in the president’s lifestyle. Certainly, he did not fit the conventional profile of a heart attack patient. He was neither gluttonous nor lazy, and he had no clear risk factor for heart disease other than a history of smoking (Figure 2) and occasionally elevated blood pressure — the latter, interestingly, now a known marker of insulin resistance (23).
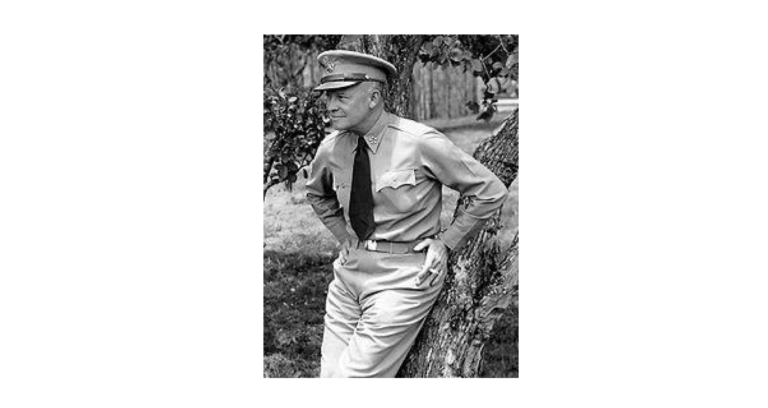
Figure 2: President Eisenhower was a heavy smoker during his army career but had stopped in 1949, six years before his first heart attack. He did not ever restart. This picture is from 1945, when Eisenhower was 54 years old and acting as Supreme Allied Commander of Operation Overlord, the Allied invasion of northwestern Europe. Eisenhower’s athletic physique is apparent. At West Point he had excelled in football. Vice President Richard Nixon considered him “a superb specimen of a man who believed in keeping himself physically fit” (2, p. 23).
In fact, in terms of his health, under the direction of Snyder, Eisenhower had been living a pretty exemplary life since he left the military in 1948.
Although the president had indeed smoked heavily while in the military, he had stopped in 1949, six years before his first heart attack. He did not ever restart, and he was dismissive of those who lacked the will power to stop smoking. When asked how he had stopped smoking cold turkey, he responded “with absolute disgust” and said, “I simply gave myself the order” (2, p. 330).
At the same time Eisenhower quit smoking in 1949, Snyder encouraged him to make other “healthy” lifestyle changes. Included were some dietary changes to treat his recurrent attacks of irritable bowel syndrome, ultimately diagnosed many years later, as Crohn’s disease. He was told to eat a “reasonable” diet, including “yogurt and other dairy products, proteins, and green and yellow vegetables, with elimination of fats and starches and sugars insofar as this is possible” (2, p. 52).
On this diet, his weight remained stable at 172 pounds (78 kg). His blood cholesterol concentration also stabilized; his average blood cholesterol concentration, measured annually between 1949 and September 1955, was a very healthy 203 mg/100mL (5.2 mmol/L), “scarcely high enough to be considered a causal factor in the heart attack” (2, p. 257). After his 1955 heart attack, his blood cholesterol concentration was measured an average of 10 times per year.
On this diet, his blood pressure was also well controlled, if occasionally high. He was considered to have “early labile hypertension,” for the treatment of which he was advised to control his weight and practice “periodic relaxation.”
Eisenhower’s one complaint was that the diet made him “hungry as a bear most of the time … (so that he) was ready to eat the china on which the food was served” (2, p. 54).
Adopting Snyder’s health advice, by the fall of 1951, Eisenhower felt so healthy he boasted, “Ever since I stopped smoking … my only complaint, aside from an occasional cold, has been the difficulty of reminding my appetite to have some consideration for my girth” (2, p. 54). Even so, he was not averse to advising his overweight friends how they should eat to remain slim: “The secret is to do without any butter, sauces, sugar, creams, or anything of that kind and never take more than one small piece of toast as a daily diet of bread” (2, p. 54). Apparently, he did not yet wonder why a “healthy” diet should make him so hungry.
It is quite understandable, then, that the president’s heart attack came as a real surprise to those attending him:
The president gave no indication whatever in these early years (of his presidency) of any personal concern about heart attack, and for good reason. He had none of the accepted conditions or signs that might portend heart disease — no family history, no high cholesterol, only marginally high blood pressure, no abnormal ekgs, and no overweight. In addition, he had been serious about his health, tending to it in every way he knew how, and the experts said that his heart was perfectly normal. It seemed beyond the realm of possibility that the nation’s number one killer could affect its number one citizen. (2, p. 69-70)
So once the medical team had seen him through the first nine difficult weeks following his heart attack, this was the dilemma they faced:
Indeed, after the 10 December examination Snyder, Mattingly and Heaton talked to (President Eisenhower) about cholesterol but admitted that otherwise they were perplexed and mentioned the attack as an ‘act of God.’ There was good reason for their uncertainty. Eisenhower’s parents had lived into their eighties with no discernible symptoms of coronary disease; his cholesterol level was below the normal level for Americans; he exercised regularly and was not overweight; his blood pressure was only mildly elevated and occasionally high; and he had stopped smoking in 1949. Thus, as he saw it, his fate was more problematic than that of the typical heart patient, who could change his lifestyle in some specific way and thereby enhance his prospects of avoiding another attack. (2, p. 144)
This frustrated Eisenhower enormously. He frequently complained that his doctors’ inability to explain why he had personally suffered a heart attack was “a sword of Damocles” hanging over his head (2, p. 151).
One of the few factors on which they could focus was the effect of stress on the president’s Type A personality. During World War II, General Omar Bradley had noted, “Another aspect of Ike was new to me: a deep-seated barely controlled anger. The public perceived him as smiling and genial. But I saw that he had a very thin skin, a short fuse and an explosive temper” (p. 38). He had occasional outbursts, which “had increased in both number and volume during his years in office” (p. 68).
The president’s temperament worried Snyder, who was concerned Eisenhower might have a stroke during one of his outbursts. Snyder realized that while recovering, Eisenhower would need to be shielded from unnecessary stress-inducing events. Eisenhower would need to “adopt a more passive philosophy” that, ironically, would “necessitate deliberate and continuous efforts on his part” (p. 162).
Jokingly, Eisenhower described how this advice affected his attitude on the golf course: “My doctor has given me orders that if I don’t start laughing instead of cussing when I miss those shots he’s going to stop me from playing golf. So every time I miss a shot you’re going to hear a haw-haw-haw” (24).
Apart from stress management, the only remaining factor on which the president’s medical team could focus real attention was his diet.
Dietary and other advice given to President Eisenhower
When President Eisenhower returned to the White House in January 1956, he received the following instructions from his medical team: He was to continue on a low-fat diet, with fat consumption remaining below 25% of his total calories; he was to maintain a weight of between 170 and 172 pounds; and he was to exercise daily and take one and a half hours’ rest at lunchtime. He also was instructed to “cultivate an attitude of equanimity towards personal and ever-present official problems.” He was told, “Emotional states are to be avoided to the greatest extent possible, that is, annoyance, anger, perturbation, anxiety, and apprehension. Avoid where possible situations conducive to emotional tension” (2, p. 172).
White’s specific dietary advice included the following: “a stringent low-fat diet, getting rid of egg yolks, all glandular organs, very fat meats, milk and cheese products, concentrated fats in salad dressings and vegetable oils, most desserts, rich gravies, olives, nuts and avocados” (p. 204). White also emphasized the importance of keeping the president’s blood cholesterol concentration low.
This diet was the forerunner of the low-fat, low-cholesterol “heart healthy” diet that would become the foundation for diets promoted by the American Heart Association (25), the American Diabetes Association (26), and the Dietary Guidelines for Americans (27).
The president’s response to the diet
During his second presidential term, Eisenhower was able to maintain his weight between 169 (77 kg) and 180 pounds (82 kg). He was convinced his body weight determined his blood cholesterol concentration, which in turn determined his risk of suffering a further heart attack. Whenever his body weight increased, he became increasingly restrictive in what he ate. This brought him into conflict with Snyder.
By the summer of 1958, Eisenhower had replaced his usual steak breakfast with fruit (papaya or melon), Melba toast, and decaffeinated coffee (2, p. 258). Snyder warned the president that he was trying to maintain his weight “at the expense of proper eating habits” (p. 258).
By the fall of that same year, when his weight had increased to 176 pounds, Eisenhower again complained that despite not eating much — by then he was eating only fruit for breakfast — “he was carrying too much weight” (p. 258). Snyder was likewise confused: “It is difficult for me to understand why he remains at this weight in as much as he played golf the last three afternoons, and did a great deal physically on his trip West over the weekend” (p. 258). A few days later, the president refused to eat any breakfast at all.
By April 1959, his blood cholesterol concentration was also beginning to rise. The next 15 of 16 measurements were above 200 mg/100 mL, the average he had maintained between 1949 and 1955 before he adopted this “heart healthy,” cholesterol-lowering diet. In response, he further reduced his dietary fat intake. He stopped using butter and removed the visible fat from all his foods.
By February 1960, his blood cholesterol concentration had increased to 214 mg/100 mL (5.53 mmol/L), and he was “having a hell of a time losing weight.” He found “a diet on which he had formerly been able to lose when he wanted to no longer served that purpose” (p. 259).
In April of the same year, Snyder noted, “He is in the same irascible mood because of his faulty manner of eating. He eats nothing for breakfast, nothing for lunch, and therefore is irritable during the noon hour. The butler, Charles, and I do not seem to be able to do anything about this. The president does this to maintain weight, and comes in and gives us hell at noon” (p. 259).
During that month, the president’s weight climbed to 179 pounds, and his blood cholesterol concentration was 223 mg/100 mL. Snyder noted, “He has eaten only one egg in the last four weeks; only one piece of cheese. For breakfast he has skim milk, fruit and Sanka. Lunch is practically without cholesterol, unless it would be a piece of cold meat occasionally. He has no fried foods. … His bread is the Vita-Pro Health Bread” (p. 260). After a brief respite when his blood cholesterol concentration dropped below 200 mg/100 mL, by August 1960, it had risen again to 259 mg/100 mL (Figure 3).
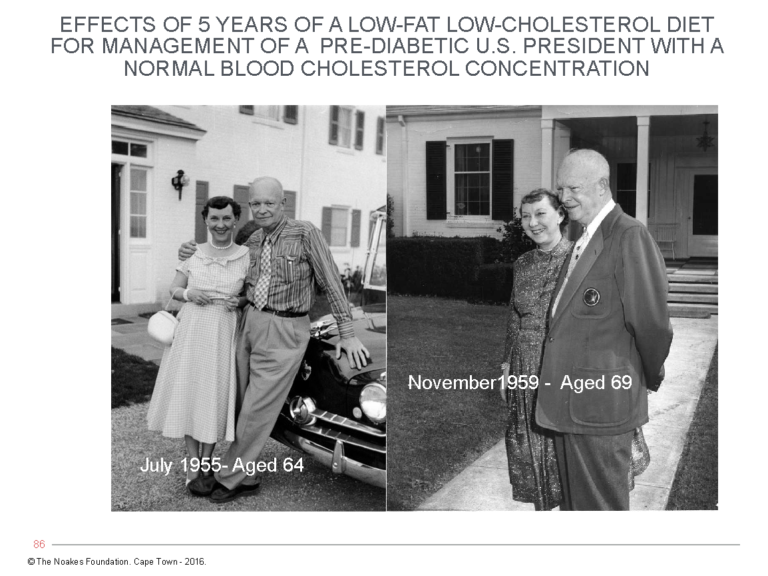
Figure 3, left: President Dwight and First Lady Mamie Eisenhower on their 39th wedding anniversary, July 1, 1955. Right: The presidential couple at the Augusta National Golf Club in November 1959, celebrating Mrs. Eisenhower’s birthday. Comparing the two photographs shows that, despite his best efforts on the “heart healthy” diet, the president had gained weight. His posture is stooped and he is losing muscle mass (developing sarcopenia). These are the expected responses to a low-fat, high-carbohydrate diet in a person who is insulin resistant.
Finally, in 1965 Eisenhower was diagnosed with Type 2 diabetes (T2DM) (p. 299). The following year he underwent surgery for removal of his gallbladder, which contained nine gallstones. Risk factors for gallstones include high-carbohydrate, low-fat diets in persons with insulin resistance (28).
Eisenhower described the difficulties he had experienced when eating a low-fat diet to a group of American Medical Association doctors. He told them maintaining a balanced diet was as difficult, and as important, as holding a balanced budget (p. 330). “There are some useless items of food all of us crave and often eat no matter unwisely … but we must conduct ourselves with a wary eye on the consequences or suffer ruined health. The choice is ours and we must act with clear mind and resolution,” he said (p. 330).
To summarize: The low-fat, low-cholesterol, “heart healthy” diet did not prevent the remorseless progression of Eisenhower’s coronary artery disease, which ultimately led to multiple heart attacks, a stroke, and death from intractable heart failure.
Instead, I would argue, the low-fat, low-cholesterol, high-carbohydrate diet converted his state of insulin resistance into full-blown T2DM, which was finally diagnosed only when the president was 74 years old, just four years before his death.
In addition, the low-fat diet caused the president to be continuously hungry and unable to control his weight, even when he attempted to severely restrict his caloric intake. Also, instead of lowering his blood cholesterol concentrations, the diet was associated with progressively rising cholesterol.
In retrospect, we can now conclude Eisenhower suffered many of the common responses exhibited by persons trying to exist on diets too low in the satiating macronutrients fat and protein. As I explained in a previous column (29), already in the 1940s, Dr. A. W. Pennington (30, 31) in New York was improving satiety in executives of Eisenhower’s age with the prescription of what would become the Atkins “no hunger” diet.
Perhaps if White had been from New York and not Boston, he might have come under the influence of Pennington, and the trajectory of global health would have been quite different.
Instead, as I will describe in the next column, White’s dietary advice for the treatment and prevention of coronary heart disease would come exclusively from one man, Dr. Ancel Keys, Ph.D.
This, as I will argue, led to disastrous results, not just for Eisenhower in 1955, but for the entire world after 1977.
Why the president’s medical team couldn’t provide answers
As was to be expected, Eisenhower was the model patient. Without complaint, he did everything asked of him by his medical team. This included following a diet that made him perpetually hungry, caused his blood cholesterol concentration to rise progressively, and made it impossible for him to control his weight.
As his disease progressed, despite diligently obeying their instructions, he had even more reason to keep asking the question: Why me?
For a number of reasons, this was the one question his medical team was unable to answer.
Understandably, their state of knowledge in 1955 was not enough for them to understand what was happening to Eisenhower from the moment of his first heart attack until his death in 1969. As a result, they missed the proverbial elephant in the room. But they were not alone — and they may count many of today’s doctors among their ranks as well.
When he was first called to attend to the president, White should have asked himself the following questions:
- Why has the president suffered a serious heart attack in the absence of any overt coronary risk factors?
- Why, if he religiously followed a healthy lifestyle from 1949 to 1955, has he suffered this heart attack?
- If an elevated blood cholesterol concentration is the crucial driver of coronary atherosclerosis, why has the president’s blood cholesterol concentration been normal for all the years (1949-1955) it has been measured?
- Are we perhaps missing something?
Recall that in his 1946 textbook, White had written, “The occasional finding of a high blood cholesterol content in fasting cases of coronary heart disease, especially in the young patient under 40, is in favor of a disturbance of fat metabolism” (5, p. 479).
But Eisenhower was 64 at the time of his first heart attack, and his blood cholesterol concentration was normal.
All this raises another crucial question: Why would White condone the prescription of the untested, entirely experimental, low-fat, low-cholesterol, high-carbohydrate diet to the president in order to lower his already normal blood cholesterol concentration?
And when the diet caused the president to be perpetually hungry, unable to control either his weight or his blood cholesterol concentration, and to suffer multiple recurrent heart attacks, why did the medical team continue with what was clearly a disastrously failed experiment of one?
What modern knowledge would have helped White make the correct diagnosis?
Had he been able to think outside the box, White might have stumbled on a key fact that he already knew because he had himself described the phenomenon in the medical literature.
In 1939, White had co-authored a study (32) of 349 deceased patients with T2DM whose postmortems were performed at two hospitals in New England. The findings were unambiguous. There was “excessive development of coronary disease in the diabetic patients of this series” (p. 29), and “coronary occlusion in this series was much more frequent in diabetic than in non-diabetic persons” (p. 29). In fact, the difference indicated coronary occlusion in four times as many diabetic patients. More modern studies have confirmed this (33).
White also likely knew of a 1931 study that reported the opinion of S. A. Levine, MD, from Peter Bent Brigham Hospital, across the way from the Harvard Medical School where White worked. Levine claimed, “Among the disease entities that are etiologically related to coronary thrombosis, diabetes is second in importance only to a previously existing hypertension” (34, p. 618). (Recall that arterial hypertension (23) is itself a marker of insulin resistance and is therefore also linked to T2DM).
The problem then as now is that the presence of T2DM will always be underestimated unless the appropriate testing is performed. For example, a 1937 Boston study of persons under 40 years of age with coronary heart disease found only 2% had been diagnosed with T2DM (35). But this figure cannot be correct if, at a slightly older age, diabetes was considered the second most important predictor of coronary thrombosis (heart attack) (34).
The point is, in 1955, T2DM was diagnosed only when the patient was perpetually thirsty because he or she was passing urine at high rates. Alerted to the possibility of T2DM, the attending physician would only then feel compelled to measure the blood glucose concentration. If elevated, a diagnosis of T2DM would then be made.
But we now know this form of disease presentation occurs only in very late stages of T2DM, after a person with insulin resistance has eaten a high-carbohydrate diet for many decades. Initially, the blood glucose concentration is held in check by the secretion of increasing amounts of insulin by the pancreatic beta cells.
But ultimately, the beta cells become exhausted, and the decades-long state of high blood insulin concentrations (hyperinsulinemia) is replaced with the sudden development of relative hypoinsulinemia, at which stage, the blood glucose concentration rises dramatically and the diagnosis of T2DM becomes obvious.
None of this was known in 1955 because the method used to measure blood insulin concentrations became available only in the 1970s (36).
So the only way White might have detected a state of pre-diabetes/insulin resistance in the president in 1955 was if he had measured fasting blood glucose concentrations — which indeed was done, if infrequently — and then followed this up with a glucose tolerance test. Even then, without the simultaneous measurements of blood insulin concentrations for up to five hours, insulin resistance and T2DM would be missed (37).
This explains the crux of the problem. Because the tools for measuring insulin resistance/pre-diabetes/T2DM were so primitive in 1955, the true contribution of insulin resistance/pre-diabetes/T2DM to coronary heart disease, including heart attacks, was profoundly underestimated.
No one had any reason to search diligently for those conditions in patients presenting with heart attacks.
In addition, Eisenhower’s heart attack occurred before the work of Peter Kuo and Margaret Albrink showed carbohydrate-sensitive hypertriglyceridemia (CSHT), not elevated blood cholesterol concentrations, is a better predictor of heart attack risk in those with T2DM (38). And his heart attack happened decades before Reaven’s work established insulin resistance as the key driver of coronary heart disease (39).
So, it is no wonder Eisenhower was not tested for insulin resistance/T2DM and the cause of his heart attack went undetermined during his lifetime.
What relevance does Eisenhower’s heart attack have in 2020?
Case reports like this can provide only limited evidence of what is and is not good medical practice. But Eisenhower’s story is epoch-making, not least because his adherence to what he was told to do made him the best possible patient any cardiologist could ever wish to have. He followed the medical advice he was given with military precision. Yet it seemed to make no difference. His heart disease advanced remorselessly. My argument is that the advice he received accelerated his development of coronary atherosclerosis.
The outstanding problem was that the true cause of Eisenhower’s heart attack, his state of insulin resistance, was missed — and understandably, because the concept of insulin resistance had yet to be discovered.
Then the president was placed on an untested, experimental diet we now know promotes the development of T2DM in those who are insulin resistant. And with T2DM comes all its distressing complications, including progressive obstructive arterial disease (33).
Today it is estimated that 88% of U.S. citizens are metabolically unhealthy, in most cases because, like Eisenhower, they are insulin resistant (40).
Here are a few key points:
- In the vast majority of persons affected by insulin resistance, the diagnosis will never be made. It will be missed, just as it was when Eisenhower had first heart attack in 1955.
- Even today, the condition, though now properly described in the medical literature (15, 23, 28, 39, 41), is still not taught in the majority of medical schools around the world.
- Lack of formal education about the insulin resistance model of coronary heart disease is probably related to the fact that the model conflicts with the simple, wrong, but still fashionable diet-heart and lipid hypotheses, which continue to be taught in medical schools globally.
- The diet-heart and lipid hypotheses contend a high-fat diet causes coronary heart disease by elevating blood cholesterol levels.
- Since this cholesterol model of heart disease underpins a massive pharmacological enterprise, including the prescription of statin drugs for lowering blood cholesterol concentrations, and since the financial survival of medical schools around the world depends on their financial support from that industry, there is absolutely no incentive to adopt a novel teaching idea that would seriously jeopardize their access to that industry’s largesse.
- As a result, medical practitioners and dietitians will continue to graduate from medical schools without any understanding of the importance of insulin resistance in the development of a multitude of chronic diseases (41).
- Inevitably, they will continue to prescribe the same bad dietary advice as that given to Eisenhower and the 88% of Americans (and similar percentages in other countries) for whom this advice is frankly life-threatening (as it was for Eisenhower).
Summary
Eisenhower’s heart attack had a profoundly influential effect in popularizing a particular idea about how heart attacks happen and how they can be prevented.
As I will show in the next column, Eisenhower’s heart attack was used by White and the man whose dietary ideas he sought and promoted — those of Ancel Keys — to advance two untested and unproven hypotheses regarding the role of dietary fat and cholesterol in the development of atherosclerosis.
Yet Eisenhower’s case study provides compelling evidence that the dietary advice corresponding to these hypotheses cannot be correct. Instead, as I argue, the diet produced T2DM in the insulin-resistant Eisenhower.
The clearest pathological effect of T2DM is the development of a specific progressive, obliterative arterial disease (33) of the kind Eisenhower developed.
Yet no one ever seems prepared to ask why the low-fat, low-cholesterol, high-carbohydrate diet, which did not work for Eisenhower, would work for them.
Perhaps it’s finally time to get real and admit to past mistakes.
The relevance of Eisenhower’s story is to warn that if low-fat, high-carbohydrate diets continue to be prescribed to persons with insulin resistance, a population that is rapidly becoming the majority (41), the outcomes will not be good.
ADDITIONAL READING
- It’s the Insulin Resistance, Stupid: Part 1
- It’s the Insulin Resistance, Stupid: Part 2
- It’s the Insulin Resistance, Stupid: Part 3
- It’s the Insulin Resistance, Stupid: Part 4
Professor T.D. Noakes (OMS, MBChB, MD, D.Sc., Ph.D.[hc], FACSM, [hon] FFSEM UK, [hon] FFSEM Ire) studied at the University of Cape Town (UCT), obtaining a MBChB degree and an MD and DSc (Med) in Exercise Science. He is now an Emeritus Professor at UCT, following his retirement from the Research Unit of Exercise Science and Sports Medicine. In 1995, he was a co-founder of the now-prestigious Sports Science Institute of South Africa (SSISA). He has been rated an A1 scientist by the National Research Foundation of SA (NRF) for a second five-year term. In 2008, he received the Order of Mapungubwe, Silver, from the President of South Africa for his “excellent contribution in the field of sports and the science of physical exercise.”
Noakes has published more than 750 scientific books and articles. He has been cited more than 16,000 times in scientific literature and has an H-index of 71. He has won numerous awards over the years and made himself available on many editorial boards. He has authored many books, including Lore of Running (4th Edition), considered to be the “bible” for runners; his autobiography, Challenging Beliefs: Memoirs of a Career; Waterlogged: The Serious Problem of Overhydration in Endurance Sports (in 2012); and The Real Meal Revolution (in 2013).
Following the publication of the best-selling The Real Meal Revolution, he founded The Noakes Foundation, the focus of which is to support high quality research of the low-carbohydrate, high-fat diet, especially for those with insulin resistance.
He is highly acclaimed in his field and, at age 67, still is physically active, taking part in races up to 21 km as well as regular CrossFit training.
References
- Taubes G. Good calories bad calories: Fats, carbs, and the controversial science of diet and health.New York, NY: Anchor Books, 2008.
- Lasby CG. Eisenhower’s heart attack: How Ike beat heart disease and held on to the Presidency. Lawrence, KA: University Press of Kansas, 1997.
- Paul O. The life and prescription of Paul Dudley White, the world’s premier cardiologist.Boston, MA: Harvard University Press, 1986.
- Messerli FH, Messerli AW, Luscher TF. Eisenhower’ billion-dollar heart attack – 50 years later. N Engl J Med. 353(2005): 1205-1207.
- White PD. Heart disease, 3rd ed. New York, NY: Macmillan, 1946.
- Eisenberg M. Bernard Lown and defibrillation. Resuscitation 69(2006): 171-173.
- Lown B. A maverick’s lonely path in cardiology (Essay 28). Dr. Bernard Lown’s Blog. Accessible here.
- Podrid PJ, Graboys TB, Lown B. Prognosis of medically treated patients with coronary-artery disease with profound ST-segment depression during exercise testing. N Engl J Med. 305(1981): 1111-1116.
- Grayboys TB, Headley A, Lown B, et al. Results of a second-opinion program for coronary artery bypass graft. JAMA 258(1987): 1611-1614.
- Jabbour S, Young-Xu Y, Grayboys TB et al. Long-term outcomes of optimized medical management of outpatients with stable coronary artery disease. Am J Cardiol. 93(2004): 294-299.
- Grayboys TB, Lown B. Good outcomes in coronary artery disease without invasive procedures. Arch Intern Med. 166(2006): 1325.
- Knipp SC, Matatko N, Wilhelm H et al. Cognitive outcomes three years after coronary artery bypass surgery: Relation to diffusion-weighted magnetic resonance imaging. Ann Thorac Surg. 85(2008): 872-879.
- Goertz RH, Rohman M, Haller JD, et al. Internal mammary-coronary artery anastomosis. A nonsuture method employing tantalum rings. J Thorac Cardiovasc Surg. 41(1961): 378-386.
- Barnard CN. A human heart transplant: An interim report of a successful operation performed at Groote Schuur Hospital, Cape Town. S Afr Med J. 41(1967): 1271-1274.
- Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 37(1988): 1595-1607.
- Accurso A, Bernstein RK, Dahlqvist A, et al. Dietary carbohydrate restriction in type 2 diabetes mellitus and metabolic syndrome: time for a critical appraisal. Nutr Metab. 5(2008): 9; Feinman RD, Pogozelski WK, Astrup A, et al. Dietary carbohydrate restriction as the first approach in diabetes management: Critical review and evidence base. Nutrition 1(2015): 1-13.
- Enig M, Fallon S. The oiling of America: Part 1 of 2. Nexus Dec. 1998-Jan. 1999; 19-23; 80-82. Accessible here.
- Herrick JB. Clinical features of sudden obstruction of the coronary arteries. JAMA 23(1912): 2015-2022; Herrick JB. An intimate account of my early experience with coronary thrombosis. Am Heart J. 27(1944): 1-18.
- Subbotin VM. Excessive intimal hyperplasia in human coronary arteries before intimal lipid depositions is the initiation of coronary atherosclerosis and constitutes a therapeutic target. Drug Disc Today 21(2016): 1578-1595.
- Leary T. Atherosclerosis, the important form of arteriosclerosis, a metabolic disease. JAMA 105(1935): 475-481.
- Haverich A. A surgeon’s view on the pathogenesis of atherosclerosis. Circulation 135(2017): 205-207.
- Greenstein FI. The President who led by seeming not to: A centennial view of Dwight Eisenhower. The Antioch Review 49(1991): 39-44.
- Reaven GM. Relationship between insulin resistance and hypertension. Diabetes Care 14(1991): 33–38. Reaven GM. Insulin resistance/compensatory hyperinsulinemia, essential hypertension, and cardiovascular disease. Diabetologia 37(1994): 948-952.
- Zern E, Lineaweaver T. Ike returns to the fairways. Sports Illustrated. 30 April 1956. Accessible here.
- The American Heart Association’s Diet and Lifestyle Recommendations. Accessible here.
- American Diabetes Association. Principles of nutrition and dietary recommendations for individuals with diabetes mellitus: 1979. Diabetes Care 2(1979): 520-523.
- U.S. Senate Select Committee on Nutrition and Human Needs. Dietary Goals for the United States, 2nd ed. Washington, DC, U.S. Government Printing Office, 1977 (See Committee Report here).
- Diehl AK. Cholelithiasis and the insulin resistance syndrome. Hepatology 31(2000): 528-529; Ruhl CE, Everhart JE. Association of diabetes, serum insulin, and C-peptide with gallbladder disease. Hepatology 31(2000): 299-303; Biddinger SB, Haas JT, Yu BB et al. Hepatic insulin resistance directly promotes formation of cholesterol gallstones. Nat Med. 14(2008): 778-782.
- Noakes TD. It’s the insulin resistance, stupid: Part 3. CrossFit.com. 30 July 2019. Available here.
- Pennington AW. Obesity in industry; the problem and its solution. Industr Med Surg. 18(1949): 259-260.
- Pennington AW. The use of fat in a weight reducing diet. Del Med J. 23(1951): 79-86.
- Root HF, Bland EF, Gordon WH, et al. Coronary atherosclerosis in diabetes mellitus. JAMA 113(1939): 27-30.
- Goraya TY, Leibson CL, Palumbo PJ, et al. Coronary artherosclerosis in diabetes mellitus. J Am Coll Cardiol. 40(2002): 946-953.
- Cruickshank N. Coronary thrombosis and myocardial infarction, with glycosuria. BMJ 1(1931): 618-619.
- Glendy RE, Levine SA, White PD. Coronary disease in youth. Comparison of 100 patients under 40 with 300 persons past 80. JAMA 109(1937): 1775-1781.
- Hodgkin DC. The Banting Memorial Lecture 1972. The structure of insulin. Diabetes 21(1972): 1131-1150.
- Kraft JR. Detection of diabetes mellitus in situ (occult diabetes). Lab Med. 6(1975): 10-22; Crofts C, Schofield G, Zinn C, et al. Identifying hyperinsulinaemia in the absence of impaired glucose tolerance: An examination of the Kraft database. Diabetes Res Clin Pract. (2016); DiNicolantonio JJ, Bhutani J, OKeefe JH et al. Postprandial insulin assay as the earliest biomarker for diagnosing pre-diabetes, type 2 diabetes and increased cardiovascular risk. Open Heart 4(2017): e000656.
- Noakes TD. It’s the insulin resistance, stupid: Part 1. CrossFit.com. 6 July 2019. Available here.
- Reaven GM. Insulin resistance and coronary heart disease in nondiabetic individuals. Arterioscler Thromb Vasc Biol. 32(2012): 1754-1759.
- Araujo J, Cai J, Stevens J. Prevalence of optimal metabolic health in American adults: National Health and Nutrition Examination Survey 2009–2016. Metabol Syndr Relat Disord. 17(2019): 46-52.
- Crofts CAP, Zinn C, Wheldon MC, et al. Hyperinsulinemia: A unifying theory of chronic disease? Diabesity 1(2015): 34-43.
Comments on It’s the Insulin Resistance, Stupid: Part 5
Thanks so much Mary Dan. My dad too died from advanced arterial disease due to type 2 diabetes. He too was prescribed the incorrect (high carbohydrate diet). At that time I too was a firm advocate of the low-fat high-carbohydrate diet for everyone, athletes especially (as I promoted in my book Lore of Running). Only 18 years after my dad's death did I experience my Damascene Moment and begin to severely restrict my dietary carbohydrate intake. Then some months later I realised that, like my father, I too have type 2 diabetes (now mercifully "in remission" thanks to a low carbohydrate diet with added CrossFit training).
President Eisenhower was a giant. He taught us to take responsibility for our actions. As you know on the day he ordered the D-Day landings on the Normandy Coast, he also wrote the following to be released if the landings failed: "Our landings in the Cherbourg-Havre area have failed to gain a satisfactory foothold and I have withdrawn the troops. My decision to attack at this time and place was based upon the best information available. The troops, the air and the Navy did all that Bravery and devotion to duty could do. If any blame or fault attaches to the attempt it is mine alone."
Medicine failed Eisenhower and both our dads. We, who understand the truth, can't allow this to continue.
Love these Noakes pieces -- and they so perfectly describe the deleterious consequences of treating the wrong thing, of treating a value instead of a patient. Of treating the fever not the strep. Or more to the point, the cholesterol instead of the insulin resistance underlying it. It makes you want to shout: 'For pity's sake, if a patient isn't getting better with your treatment course, don't double down, change course!'
Through the retrospectoscope we can watch as 'Ike' declines in health and gains in girth, while faithfully following the prescription of that day's medical wizards (which advice is sadly not all that different from what today's wizards' would recommend.) Though admittedly the low-fat high carb diet isn't all that is to blame here. There is little doubt that his long-term heavy smoking played an important and causative role in the development of his atherosclerotic cardiovascular disease, as it did for so many of his generation, when GIs were issued cigarettes and told when at ease to 'smoke 'em if you've got 'em.' There were many like Ike, but few as famous. Here's one I know about first hand.
My own father was of that generation; he enlisted at age 17 in 1942 and served in the Pacific theater with the Army (building air strips with the Airborne Engineers) for the duration plus 6 months. And like Ike, he developed crippling ASCVD, suffering his first MI at age 39. (His case was complicated additionally by the onset of equally crippling Rheumatoid Arthritis at about the same time.) He, like Ike, was put on a low-fat, high carb diet prescription designed to save him, given the standard medical therapy of the day, and told to stop smoking. (He finally quit smoking when inhaling caused angina.)
That first MI was followed by 8 or 9 more over the next 19 years, huge weight gain, congestive failure, and ultimately a 4 vessel bypass that was deemed mostly palliative to relieve intractable angina, since his ejection fraction was something around 25% by then; they didn't hold out too much hope. He survived, however, and the angina improved, and he was even cleared to undergo two knee replacements and a hip replacement in the next couple of years. But his progress was sidelined by an emergency cholecystectomy--his cholecystitis being , like Ike's, another manifestation of the insulin resistance syndrome. The general anesthesia took a toll and the surgery itself was more difficult than would be usually the case with a simple gall bladder. His surgeon said he'd never seen a gall bladder that huge -- he sent it out to the waiting room for me to see. It completely filled a kidney basin.
In 1983 (years before Mike and I had had our 'nutritional brain transplants' about the impressive health benefits of the lower carb WOE that we were later to embrace and use to treat thousands of patients) my father died of end stage congestive failure at age 58.
His case is an 'n of 1' or I guess 'n of 2' if you count Ike. But the clear message of his trajectory and Ike's is that the prevailing 'state of the art' medical and dietary therapy utterly failed them. Medicine failed them. And so many others. They were treating the wrong thing with a damaging therapy. They were looking in the wrong place.
As Prof Noakes reminds us here, 'It's the Insulin Resistance, Stupid!' Treat that with a diet of meat (fish, poultry, eggs, full fat dairy), low-starch vegetables, some nuts and seeds and low-sugar fruits and no concentrated sugars or starches and get off the couch and the results will amaze you.
It’s the Insulin Resistance, Stupid: Part 5
2