It is November 1963. The 33-year-old New York physician Dr. Robert Atkins, MD, is dissatisfied with his life — and his physical appearance. He reckons he has gained 90 pounds in the 16 years since he graduated from high school in Dayton, Ohio. But his medical training at the University of Michigan and Cornell Medical College has provided no answers to his persistent worry: How do I lose this excess weight (2)? He has already experimented with a number of different weight-loss diets but without any lasting success. Always the outcome is the same: His willpower capitulates to ravenous hunger.
Then the unimaginable happens. At midday on November 22, 1963, President John F. Kennedy is assassinated in Dealey Plaza, Dallas, Texas. As he watches the story unfold on national television, Atkins becomes deeply depressed. He decides that it is time to save his own life. He vows that his recovery must begin immediately. To start, he must somehow find a way to lose his excess weight.
He begins with one rule: He will never again attempt any diet that makes him hungry — not even for a single day. He decides to devote himself to solving this baffling riddle: How can one eat less without being perpetually hungry? His natural inclination is to search for answers in the medical literature, and he begins in the medical school library.
His first discovery is the work of Garfield Duncan, MD (3-5). Duncan describes his use of total fasts lasting one to 15 days for the treatment of intractable obesity. There, Atkins uncovers the first two clues: “Anorexia was the rule after the first day of fasting and paralleled the degree of hyperketonemia. A sense of well-being was associated with the fast” (2, p. 309); “Ketonuria usually occurred on the first or second day of the fast and hyperketonemia was detectable on the second day and increased as the fast progressed (3, p. 124-125). The sense of well-being and cheerfulness was surprisingly constant; anorexia was striking, notably after the first day of the fast, but in many patients, hunger was not a complaint at any time. Several patients expressed a desire to continue the fast beyond 14 days; there was a close relationship between hyperketonemia and the loss of appetite in every case (p. 126). The anorexia during total abstinence from food, Duncan writes, is associated with and believed to be due to the hyperketonemia provoked by the fast (p. 126).
Atkins concludes that the development of ketosis explains the anorexia of fasting, but he knows fasting cannot be a long-term solution. He narrows his search to discover a diet that will produce persistent ketosis while providing sufficient calories for sustained health.
His search takes him to a study published just eight months earlier by G.J. Azar and W.L. Bloom, two physicians from Atlanta, Georgia. In their article, entitled “Similarities of carbohydrate deficiency and fasting. II. Ketones, nonesterified fatty acids, and nitrogen excretion” (6), Azar and Bloom note, “At a cellular level, the major characteristic of fasting is limitation of available carbohydrate as an energy source. Since fat and protein are the energy sources in fasting, there should be little difference in cellular metabolism whether the fat and protein come from endogenous or exogenous resources” (p. 92).
Azar and Bloom’s study reports that the low-carbohydrate diet “similar to the endogenous caloric mixture of fasting” produced a 10-fold increase in blood ketones within the first 24 hours that continued until the subjects again ate carbohydrates. The authors conclude that the availability of dietary carbohydrate determines this ketogenic response. In addition, they note, “The fat-sparing action of glucose in normal metabolism is out of proportion to its calorigenic capacity” (p. 341).
So, if fasting and low-carbohydrate diets have the same effects on human metabolism, and both produce significant ketosis, Atkins reasons that perhaps a “carbohydrate-deficient” diet is the hunger-free, healthy eating plan for which he is searching.
Returning home, he decides to test the idea on himself: “He threw out the bread and donuts in his kitchen, instead filling the refrigerator with as much fresh shrimp as he could hold. He followed the same routine when he wasn’t at home.”
“He lost twenty-eight pounds in six weeks. The rest is history” (2, p. 55).
Atkins discovers the work of Drs. Blake Donaldson and Alfred Pennington
Atkins’ subsequent academic search introduces him to the work of two other New York physicians, Drs. Blake F. Donaldson and Alfred Pennington, both of whom had been promoting low-carbohydrate diets, Donaldson from as early as the 1920s.
As Gary Taubes, who carefully researched the topic, explains, Donaldson had been working with a group of “fat cardiacs” in New York (7). Frustrated at their inability to lose weight when trying to eat less and exercise more, Donaldson seeks another explanation (1). By chance, he befriends a Canadian engineer who is himself a friend of the Arctic explorer Vilhjalmur Stefansson, author of a series of books describing his life among the Arctic Inuit (8-12). After they meet in New York City and Stefansson describes how the Inuit live on a purely carnivorous diet, Donaldson recalls wondering, “What was I worrying about? If Stefansson could get his people (North American Europeans) to live that way, I certainly should have enough executive ability to get my patients to stick to a beautifully broiled sirloin and a demitasse of black coffee” (1, p. 41).
Based on the meat-only diet Stefansson had eaten for a full year during the iconic laboratory study that included himself and fellow explorer Karsten Anderson (13), Donaldson designs an identical diet of three meals a day, each of a half-pound of fatty meat, three parts fat to one part lean protein by calories. After cooking, this would provide 18 ounces of lean meat with six ounces of attached fat per day (1). The Stefansson/Donaldson diet prohibits all sugar, flour, alcohol, and starches, with the exception of a small portion of raw fruit or potato once a day.
According to Taubes (7), Donaldson claims to have treated about 17,000 patients over four decades, most of whom lost two to three pounds per week on the diet without experiencing hunger. The only patients who failed to lose weight were those with a “bread addiction,” for which his advice was, “No breadstuff means any kind of bread … . They must go out of your life, now and forever.” To diabetics, he admonished: “You are out of your mind when you take insulin in order to eat Danish pastry.”
Donaldson does not publish any personal scientific research, preferring to speak only to audiences at the New York Hospital, where Pennington, a local internist, hears him speak. Impressed, Pennington tests the diet on himself and soon begins prescribing it to his patients.
At the time, Pennington is employed as a company physician in the medical care division of E.I. du Pont de Nemours and Company. By 1948, the company is becoming concerned about the rising incidence of heart attack among its employees; the target of the diet prescription is the prevention and reversal of obesity in the hope that this will reduce heart-disease risk.
The original dietary intervention followed the standard for the day, which called for a reduction in portion size, calorie counting, limiting the amount of fat and carbohydrate consumed in meals, and exercising more (7). The results of the original diet were predictable: None of those things worked, so instead Pennington and his team decided to test Donaldson’s diet on their overweight executives.
In his first publications (14, 15), Pennington reports the outcomes in 20 Du Pont executives who have lost between nine and 54 pounds at an average rate of nearly two pounds per week. Subjects ate a minimum of 2,400 calories.
“Notable was a lack of hunger between meals, increased physical activity and sense of well-being,” Pennington writes. Although carbohydrate intake was restricted to no more than 80 calories (20 grams) at each meal, he notes that “in a few cases even this much carbohydrate prevented weight loss, though an ad-libitum (unrestricted) intake of protein and fat, more exclusively, was successful” (14, p. 260).
Pennington subsequently writes extensively on what he learns from his clinical experience working with these patients (16-23). The model of obesity he develops includes the following:
- Appetite is homeostatically regulated to ensure energy intake exactly matches energy expenditure. The mechanism can be affected by (i) altered hormonal influences, as in hyperinsulinemia or through the action of the stress hormones; (ii) structural damage to the center (in the hypothalamus); (iii) conscious overeating (“careless or perverted eating habits”).
- Alterations in “lipophilia,” which is the theory that obesity is the result of “increased fat storage in the body (and which is) presumed an active regulation of the size of the adipose deposits, rather than the mere passive response to the balance between calorie intake and output” (18, p. 102, my emphasis). (This concept is first described in the English scientific literature by Julius Bauer (24): “The adipose tissue is not merely a passive storing place for reserve fat, but a living and active part of the body, with its own physiologic and pathologic processes” (p. 993). Lipophilia explains, for example, why hunger is stimulated by weight loss and is only restrained when the adipose fat stores are again refilled.)
- Fat is stored in adipose tissue, not just from ingested fat but also from carbohydrate (22), and this later process is stimulated in the presence of insulin.
- The oxidation of fat is impaired in the obese, a consequence of a reduced capacity to fully oxidize carbohydrates. Instead, partial (glycolytic; fermentation) carbohydrate metabolism causes blood pyruvic (and lactic) acid levels to rise. Higher pyruvic acid levels then inhibit fat oxidation in all tissues, particularly in the muscles. Thus, pyruvic acid is a metabolic regulator, “stimulating fat formation and inhibiting fat oxidation” (18, p. 104).
- Since the obese have an impaired capacity to generate energy from both carbohydrate and fat, they will be continually hungry. As a result, “excessive fat storage, or obesity, would be the cause of an increased appetite, rather than the result of it” (22, p. 71).
Pennington states his hypothesis in the following terms: “Obesity, in most cases, is a compensatory hypertrophy of the adipose tissues, providing for a greater utilization of fat by an organism that suffers a defect in its ability to oxidize carbohydrate” (21, p. 68).
He concludes that if obesity is due to excessive fat storage (lipophilia) directed by the fat cells themselves, then caloric restriction is a non-specific therapy that acts solely at the level of the appetite, reducing calorie consumption without addressing the disordered drive of the fat cells to store excessive amounts of fat. His solution is to promote treatment “directed primarily toward mobilization of the adipose deposits,” which would allow the appetite “to regulate the intake of food needed to supplement the mobilized fat in fulfilling the energy needs of the body.”
Since incomplete metabolism of carbohydrate is the key factor preventing fat utilization, “Limitation of dietary carbohydrate, specifically, as the chief source of pyruvic acid makes possible a treatment of obesity without restriction of the total caloric intake” (22, p. 73). His experience with the Du Pont executives teaches him, “The use of a diet allowing an ad libitum intake of protein and fat and restricting only carbohydrate appears to meet the qualifications of such a treatment” (18, p. 104).
The advantages of this approach include the following:
Restriction of carbohydrate, alone, appears to make possible the treatment of obesity on a calorically unrestricted diet composed chiefly of protein and fat. The limiting factor on appetite, necessary to any treatment of obesity, appears to be provided by increased mobilization and utilization of fat, in conjunction with the homeostatic forces which normally regulate the appetite. Ketogenesis appears to be a key factor in the increased utilization of fat. Treatment of obesity by this method appears to avoid the decline in the metabolism encountered in treatment of caloric restriction. (19, p. 347).
Pennington also notes that some patients become hungry on the low-carbohydrate diet and need to “increase their fat intake” (23, p. 36). He writes: “Provided carbohydrate is restricted sufficiently, there does not seem to be any need to restrict fat at all … . Although the emphasis has often been put on protein in constructing diets for the obese, it seems that the emphasis should be put on fat as the major source of energy, with carbohydrate restricted to the degree necessitated by the obesity defect, and ample protein allowed for its well-recognized benefits to health” (23, p.36).
Pennington’s ideas strengthen Atkins’ understanding that a low-carbohydrate diet that induces ketosis and reduces hunger without requiring significant caloric restriction is the solution for his own weight problem — and perhaps for many others who have a similar problem.
Atkins is further encouraged by a recent publication showing that the Pennington diet reduces hunger and produces weight loss in the majority: “Our results do show that satisfactory weight loss may be accomplished by a full caloric, low carbohydrate diet. The patients ingested protein and fat as desired. Careful attention was paid to keeping carbohydrate intake to a minimum” (25, p. 1413).
The authors continue: “All the other methods of weight reduction mentioned earlier have been utilized by the author in the past. The diet discussed was found to be the most satisfactory of all these methods in our hands. Weight reduction occurred dramatically with a rapid fall early and proceeding slowly but surely” (25, p.1414).
Perhaps Atkins also reads the chairman’s address, presented by George L.Thorpe, MD, of Wichita, Kansas, at the 106th Annual Meeting of the American Medical Association in New York on June 4, 1957 (26). There, Thorpe repeats the Pennington interpretation of how a low-carbohydrate diet induces weight loss in the obese: “That the usual low-calorie diet is rarely successful is readily understood in the light of our present knowledge of carbohydrate and fat metabolism … (as) the presence of carbohydrate suppresses the fat-mobilizing ability of the pituitary gland and increases the fat-depositing activity of insulin” (p.1364).
Thorpe says, “It is possible to lose weight without counting the calorie intake, without being weak, hungry, lethargic, irritable, and constipated. There is no magic or mystery, no fancy rules to follow, and the entire program may be successfully conducted without radical change to one’s normal routine … but the key to long-term success is the simple return to normal eating habits. Normal eating habits might be described in technical language as adhering to a high-protein, high-fat, low-carbohydrate diet” (p. 1364).
Thorpe then describes how his own consumption of high-carbohydrate foods had caused him to develop a “personal problem of excess weight” and how, in trying to solve this personal issue, he had discovered the low-carbohydrate diet promoted by Stefansson, Donaldson, and Pennington.
This information likely confirms to Atkins that the solution to his personal weight problem is the same as it was for Thorpe: a low-carbohydrate diet.
The studies of Kerwick and Pawan
Atkins finds one final piece of evidence to further support his growing conviction that he has discovered a “cure” for obesity. Dr. A. Kerwick and Mr. G. L. S. Pawan from Middlesex Hospital Medical School had also become disillusioned with the calories-in, calories-out model of human weight control (27-29). As they wrote, “If deficiency of calories accounts for loss of weight, low calorie diets should induce the same rate of weight loss in the same patient, no matter what the composition of the diet. Manifestly they do not do so” (29, p. 449).
A series of their studies shows that whereas subjects eating a low-calorie (1,000 cal), high-protein or high-fat diet for seven days lost substantial amounts of weight, eating a high-carbohydrate diet resulted in little if any weight loss (28). They conclude, “An alteration in metabolism takes place (in those eating low-carbohydrate diets)” (28, p. 161). This alteration in metabolism apparently explains the greater rates of weight loss in those eating low-carbohydrate diets.
We now know that Kerwick and Pawan’s conclusions are in error. Marjorie Yang and Theodore Van Itallie subsequently show that, in the short term, any differences in absolute weight losses on isocaloric diets differing in their fat, protein, and carbohydrate contents can be explained entirely by much greater water losses on the higher fat and protein diets (30). However, this applies only to short-duration studies of less than perhaps 14 days or so. The one fact established by these studies is that high-carbohydrate diets promote fluid retention, most likely as a result of an insulin effect increasing water retention by the kidneys (31).
Fortunately, at the time, Atkins is unaware of this error.
The Eric Westman, MD, Connection
By the late 1960s, Atkins has converted his private medical practice to focus purely on weight loss using the low-carbohydrate diet. Although he treats tens of thousands of patients during this period, he has little interest in documenting the results of his diet prescription on their health. He is happy to be surrounded by so much clear evidence of success.
In 1997, Dr. Eric Westman, a physician practicing at the Duke University Medical Center in Durham, North Carolina, is becoming concerned that some of his patients have chosen to follow what had by then become known as the Atkins Diet. In particular, he is worried that the high fat content of the diet will increase his patients’ blood cholesterol concentrations, placing them at risk of “artery clogging” and heart attacks. He is initially so skeptical of Atkins’ dietary advice that “he didn’t believe Atkins actually had gone to medical school and earned his M.D.” (2, p. 167).
Yet Westman’s patients continue to show impressive weight loss. At their suggestion, he agrees to read Atkins’ first book (32). He remains puzzled about how Atkins can claim success from a diet that conflicts with everything Westman has been taught in his medical training. He can’t understand how, first, his patients are losing weight eating so much fat, and second, why their blood cholesterol concentrations don’t seem to be reaching dangerous levels.
When faced with such a paradox, the majority of physicians simply ignore it as if what they are seeing hasn’t really happened. But Westman is different. He writes to Atkins, who invites him to come to New York to sit in on some patient consultations. Later, Westman recalls, “I was both surprised and impressed that he actually had an office and was seeing patients. I had to see through the veneer of the book before I could actually start to believe the concept behind the diet” (2, p. 169).
By the end of his visit, Westman has convinced Atkins that he needs to fund rigorous scientific studies to prove to a growing body of medical skeptics that his diet is safe and can successfully treat obesity and Type 2 diabetes mellitus (T2DM).
Westman findS a low-carbohydrate diet can put T2DM into remission
Westman uses Atkins’ funding to undertake a six-month pilot study of the effects of a low-carbohydrate (<25 g/day) diet “with no limit on caloric intake” on body weight and blood lipid parameters in 51 overweight/obese healthy volunteers (33). The 41 subjects who adhere to the program lose an average of 9.0 kg (19.8 lb.) and improve all their blood parameters, including lowering their total cholesterol and LDL-cholesterol concentrations. The authors conclude rather modestly, “A very low carbohydrate diet program led to sustained weight loss during a 6-month period (without any adverse effects in the 41 subjects who completed the program).”
The study leads to a larger study, this time with 120 subjects, 60 of whom follow a hypocaloric low-fat diet and the other 60 a low-carbohydrate diet for 24 weeks (34). The study finds that “compared with a low-fat diet, a low-carbohydrate diet program had better participant retention and greater weight loss.” The authors observe, “During active weight loss, serum triglyceride levels decreased more and high-density lipoprotein cholesterol levels increased more with the low-carbohydrate than with the low-fat diet” (p. 769).
Predictably, when the same study is presented at the American Heart Association (AHA) meeting in November 2002, the Association feels compelled to issue a media advisory that conveys its “concerns with the study” in the following terms:
- The study is very small, with only 120 total participants and just 60 on the high-fat, low-carbohydrate diet.
- This is a short-term study, following participants for just 6 months. There is no evidence provided by this study that the weight loss produced could be maintained long term.
- There is no evidence provided by the study that the diet is effective long term in improving health.
- A high intake of saturated fats over time raises great concern about increased cardiovascular risk — the study did not follow participants long enough to evaluate this.
- This study did not actually compare the Atkins diet with the current AHA dietary recommendations. (35)
The advisory concludes with a statement from Robert O. Bonow, MD, President of the AHA: “‘Bottom line, the American Heart Association says that people who want to lose weight and keep it off need to make lifestyle changes for the long term — this means regular exercise and a balanced diet.”
Bonow adds, “People should not change their eating patterns based on one very small, short-term study. Instead, we hope that the public will continue to rely on the guidance of organizations such as the American Heart Association which look at all the very best evidence before formulating recommendations.”
This advisory echoes some of the sentiments published in the Journal of the American Medical Association 29 years earlier in a highly critical review of Atkins’ first book (36). The article is attributed to Philip L. White, D.Sc., Secretary of the American Medical Association Council on Food and Nutrition. White is not a trained medical practitioner.
White’s relevant points include the following:
- “The low-carbohydrate diet approach to weight reduction is neither new nor innovative” (p. 1415).
- “If such diets are truly successful, why then, do they fade into obscurity within a relatively short period only to be resurrected some years later in slightly different guise and under new sponsorship?” (p. 1415).
- “Moreover, despite the claims of universal and painless success for such diets, no nationwide decrease in obesity has been reported” (p. 1415).
- “Dietary carbohydrate, particularly sugar, is considered by some advocates to be a nutritional ‘poison’ that promotes ‘hypoglycemia’, diabetes, atherosclerosis and, of course, obesity” (p. 1415).
- “… the weight reduction that occurs in obese subjects who are shifted to a low-carbohydrate diet seems to reflect their inability to adapt rapidly to the marked change in dietary composition” (p. 1416).
- “There appears to be no inherent reason why body weight cannot be maintained on a diet devoid of carbohydrate if the other essential nutrients are provided” (p. 1416). (Dr. White appears to have forgotten this is a discussion on diets for weight loss, not weight maintenance.)
- Many human populations remain lean “on diets extremely high in carbohydrate (by American standards) and correspondingly low in fat.” Thus, “there is equally no inherent reason to associate a diet rich in carbohydrate with obesity” (p. 1416).
- Potential hazards of low-carbohydrate diets include hypercholesterolemia and hypertriglyceridemia (p.1416-1417). (White does not realize hypertriglyceridemia is caused by high-carbohydrate diets in those with carbohydrate-sensitive hypertriglyceridemia, but he is right to note hypertriglyceridemia is a risk factor for coronary heart disease).
- Other potential hazards include hyperuricemia, fatigue, and postural hypotension. (Note: Postural hypotension is a benign condition and indicates that the diet is producing an overall reduction in blood pressure. This surely is good since high blood pressure is common and in most is described as “essential hypertension.” In other words, medicine has no understanding of what is causing the hypertension, but if a low-carbohydrate diet causes hypotension, could this not possibly be an indication of a possible mechanism for hypertension — high-carbohydrate diets in persons with insulin resistance?)
- “The assertion that carbohydrates are the principal elements in foods that fatten is, at best, a half-truth” (p. 1417). White argues instead that higher rates of dietary fat intake explain the high rates of obesity in North Americans: “Obesity is relatively rare in large areas of the world where the ‘hidden sugar’ of rice starch comprises a very high proportion of the total daily food intake” (p. 1417).
- White concludes: “The ‘diet revolution’ is neither new nor revolutionary” (p. 1418). He argues the low-carb diet is simply a variant of a diet that has been promoted for many years. The rationale used to promote the diet is “for the most part without scientific merit” (p. 1418). The unlimited intake of saturated fat and cholesterol-rich foods may well increase “coronary artery disease and other clinical manifestations of atherosclerosis … particularly if the diet is maintained over a prolonged period” (p. 1418). “Any grossly unbalanced diet, particularly one which interdicts the 45% of calories that is usually consumed as carbohydrate, is likely to induce some anorexia if the subject is willing to persevere in following such a bizarre regimen” (p. 1419). “Bizarre concepts of nutrition and dieting should not be promoted to the public as if they were established scientific principles” (p. 1419). “Patients should counsel their patients as to the potentially harmful results that might occur because of the adherence to the ‘ketogenic diet’” (p. 1419). And finally: “Observations on patients who suffer adverse effects from this regimen should be reported in the medical literature or elsewhere, just as in the case of an adverse drug reaction” (p. 1419).
Important points missing from White’s critique include the following:
- He ignores evidence from North America that establishes a high-fat diet can manage T2DM (see subsequent discussion). He also ignores Pennington’s work, which shows obesity can be effectively treated with this dietary intervention.
- He ignores opinions from Britain, especially the published work of John Yudkin, a former Professor of Nutrition and Dietetics at the University of London. Unlike White, but like Pennington (and Atkins), Yudkin had actually studied the low-carbohydrate diet in real patients and become convinced of the value of this diet for the management of obesity (37-41). Thus, Yudkin wrote in 1972: “I have no doubt that in practice the low-carbohydrate diet will be found to be the most effective and, nutritionally, the most desirable for the management of obese patients” (41, p. 154). In the same article, he warned of the danger of drawing conclusions from theoretical considerations rather than practical experience.
- White ignores the editorial by Thorpe, advocating the value of this diet in the same journal two decades earlier (26).
- He ignores Atkins’ extensive discussions of the role of carbohydrate intolerance (insulin resistance) in obesity and T2DM, as well as Atkins’ explanation of why the high-fat diet works in persons with this condition. White, who is not a medical practitioner and has no personal experience in the treatment of persons with obesity/T2DM, fails to appreciate that Atkins’ advocacy was for a diet that worked best for persons with carbohydrate intolerance/insulin resistance.
- White’s errors are further underscored by the absence of reports in the medical literature of “adverse effects from the regimen” in the 46 years since he made the plea that all such negative outcomes should be reported.
None of White’s misgivings deter Westman, who negotiates with Atkins to fund another trial, this time in persons with T2DM. The resulting study finds that 21 patients with T2DM who followed the diet for 16 weeks lost an average of 9 kg (19.8lbs), reduced their blood HbA1c values by 1.2% (Figure 1), and improved all their blood markers, including reducing blood triglyceride concentrations by an average of 1.1 mmol/L (42). Seventeen of the 21 patients reduced or stopped using anti-diabetic medications, indicating disease “remission” or perhaps even “reversal” in some.
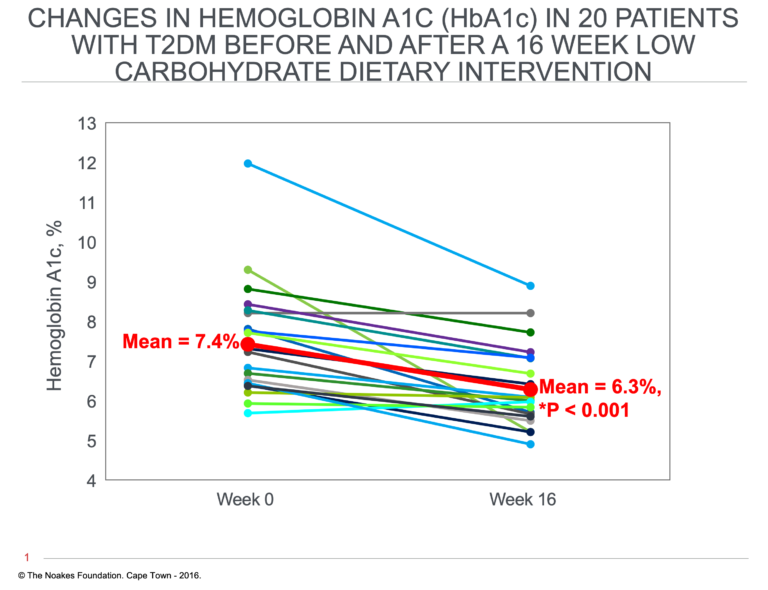
Figure 1: Changes in glycated hemoglobin (HbA1c) concentrations in 21 patients with T2DM who ate a low-carbohydrate diet for 16 weeks. HbA1c concentrations are a measure of the average 24-hour blood glucose concentrations over the previous three months. Values greater than 6.5% are considered diagnostic of T2DM. According to this measurement, 14 of 21 (67%) patients put their T2DM into “remission” on this eating plan. Reproduced from reference 42.
Since an HbA1c below 6.5% is considered to be the upper end of the “normal” range, perhaps this is the first study in the modern literature showing “remission” or “reversal” of T2DM while using nothing more than a dietary intervention. Importantly, there is no single report in the medical literature documenting T2DM “remission” or “reversal” while following usual medical care including the prescription of insulin or other medications.
For historical completeness, it’s appropriate to mention that Leslie Newburg and colleagues at the University of Michigan began to use a high-fat, low-carbohydrate diet to treat T2DM in the 1920s (43-49). It seems probable that among the 73 patients they reported in their first paper (43), some may have gone into “remission” on the high-fat diet. Indeed, their second paper (44) shows a number of patients whose random blood glucose concentrations fall below 5.5 mmol/L (0.10%), as does their third paper (45). The authors also argued that mortality in the group treated with this diet was no worse and might even have been slightly better than that for similar patients treated with the low-fat, low-calorie diet then promoted at the Joslin clinic.
In 1973, J.R. Wall and colleagues also reported the use of a carbohydrate-restricted diet produced “good diabetic control on diet alone, in two-thirds of cases by the time of the second visit — that is, within 2 to 3 weeks” (51, p. 578). The authors’ main focus was not on “reversal” of T2DM. Rather, they wished to determine whether weight loss or carbohydrate restriction was the key to successful management of T2DM. They concluded that “control of diabetes in obese patients who respond to diet alone is due to carbohydrate restriction rather than to weight loss” (p. 578).
These studies show that already in the 1920s, there were those who argued that a carbohydrate-restricted diet is beneficial for the management of T2DM.
Westman and his colleagues establish this as fact, and their study shows that on a carbohydrate-restricted diet, some T2DM patients do not require medications to maintain good glucose control (42).
It takes another 13 years for a larger study to confirm these findings and bring the value of the low-carbohydrate diet for the management of T2DM to a much wider audience.
The studies of Steven Phinney and Jeff Volek
Drs. Jeff Volek, Ph.D., and Stephen Phinney, MD, are two other scientists whose research was funded by the Atkins Foundation. They undertake a number of studies of low-carbohydrate diets in different populations, ultimately focusing on changes in blood lipid profiles in those with metabolic syndrome (52-58).
The key difference between their work and Dr. Gerald Reaven’s is, for the reasons I will suggest in due course, that Reaven balks at studying truly low-carbohydrate diets. Instead, Volek and Phinney choose to study properly low-carbohydrate diets (<50 g/day), and in the end, that makes all the difference.
Some of the most important findings from these studies are shown in Figure 2.
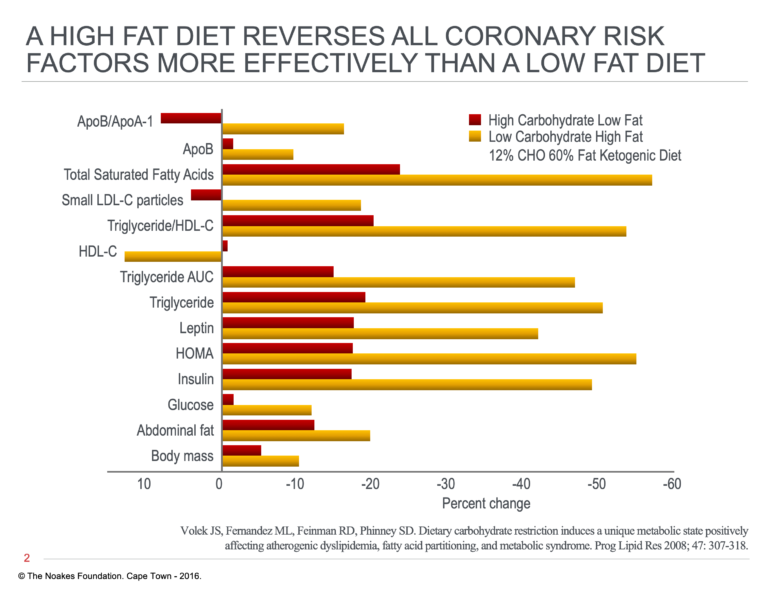
Figure 2: Changes in metabolic and other health markers in person with metabolic syndrome, randomized to either a high-carbohydrate (56%), low-fat (24%) diet or a high-fat (59%), low-carbohydrate (12%) diet. Both diets were hypocaloric (~1,500 cal/day). Note that all variables show greater improvement on the low-carbohydrate diet than the low-fat diet. Data from reference 54.
The evidence clearly shows that all variables improve to a greater extent on the low-carbohydrate diet. The greatest reductions are in blood triglyceride, insulin, and saturated fatty acid concentrations, with a marked increase in blood HDL-cholesterol concentrations as well.
The authors conclude:
Restriction in dietary carbohydrate, even in the presence of high saturated fatty acids, decreases the availability of ligands (glucose, fructose, and insulin) that activate lipogenic and inhibit fatty oxidation pathways. The relative importance of each transcriptional pathway is unclear, but the end result — increased fat oxidation, decreased lipogenesis, and decreased secretion of very low-density lipoprotein — is a highly reliable outcome of a low-carbohydrate diet. (55, p. 309)
In their most recent study, Phinney and Volek find that these benefits can occur rapidly and are not dependent on weight loss (58). There, they conclude: “Overall, this work highlights the importance of the dietary carbohydrate-to-fat ratio as a control element in Metabolic Syndrome expression and points to low carbohydrate diets as being uniquely therapeutic independent of traditional concerns about dietary total and saturated fat intakes … . Based on these results, any long-term trials in participants with Metabolic Syndrome should include low carbohydrate diets” (p. 11).
Phinney and Volek’s studies confirm and extend Reaven’s findings from between 1987 and 1994 (59), and address the impact of low-carbohydrate diets on the metabolic profile and other health markers of persons with the metabolic syndrome.
Logically, Reaven’s group should have completed and published studies identical to these already by the turn of the last century. Why they did not is a mystery I will explain subsequently.
Sami Inkinen and the Virta Health study confirm Atkins is correct
Certain that the low-carbohydrate diet could correct the metabolic syndrome (55) and might even “reverse” T2DM in some individuals (41), some time around 2014, Phinney has the opportunity to speak to recently retired Sami Inkinen, who was planning to row across the Pacific from San Francisco to Honolulu on a carbohydrate-free diet (60, 61). Phinney, together with Jeff Volek, wishes to repeat the Westman study (41) in a larger group. But Phinney and Volek need help, so they ask Inkinen if he would be interested.
Inkinen agrees on one condition: that the study becomes part of a startup tech company, the ultimate goal of which is to “reverse diabetes in 100 million persons by the year 2025.” And thus, the Virta Health company is founded.
By 2016, the new company has recruited 262 persons with T2DM for a five-year study using a novel model of remote care that focuses on the prescription of a ketogenic, low-carbohydrate diet with regular feedback using relevant biometric measurements of food intake, and blood glucose and insulin concentrations.
In early 2017, the results of the first 10 weeks of the intervention are published (62). They show that the ketogenic diet reduces blood HbA1c by 1% (compare with Figure 1), even though 57% of subjects have either reduced or terminated their use of diabetic medications; 56% of subjects have reduced HbA1c values to below 6.5%, the value traditionally used for a diagnosis of T2DM.
In February 2018, the results for the first year of the study are published (63)*. Average HbA1c levels were now 6.3%, down from 7.6%; average weight loss was 13.8 kg; medication use other than metformin had decreased from 57% to 30%; and 94% of subjects had reduced or eliminated insulin therapy (Figure 3).
*Editor’s Note: As noted on CrossFit.com on May 14, 2019, the trial to which Prof. Noakes refers “was funded and run by Virta Health, a private company that sells the app used in the trial to privately insured employers; as such, the trial involves a conflict of interest similar to a pharma-funded drug trial. Additionally, the 262 subjects all chose to opt into the Virta program and were neither randomized nor blinded. Despite these issues, the significance of this trial can hardly be overstated. This trial represents the first clear, long-term evidence in a large population that a ketogenic diet, when followed properly, can lead to significant improvements in health among Type 2 diabetics, and in many cases (in this trial, the majority) even resolves diabetes completely.”
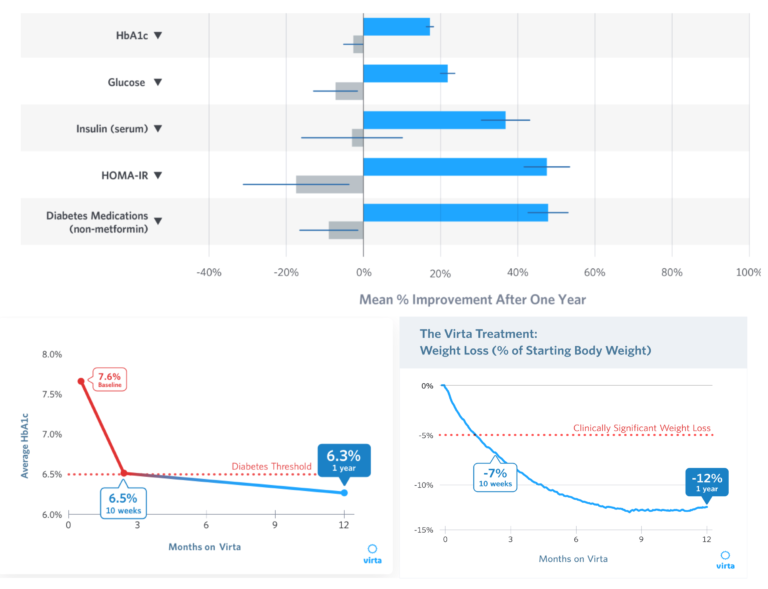
Figure 3: Top Panel: Percent changes in HbA1c, fasting blood glucose and insulin concentrations, Homeostatic Model Assessment – Insulin Resistance (HOMA-IR), and diabetic medication use in persons with T2DM on the Virta Health intervention (blue) compared to patients receiving standard care (gray). Bottom left panel: Absolute changes in average HbA1c levels over the first 12 months of the Virta Health intervention. Bottom right panel: Percent weight loss in T2DM patients receiving the Virta Health intervention. Reproduced from the Virta Health website.
A separate paper compared changes in cardiovascular disease risk factors in the same populations (64). With one exception (circled in Figure 4), all changes in the Virta Health group were greater and considered to be more healthy than those in the usual care group.
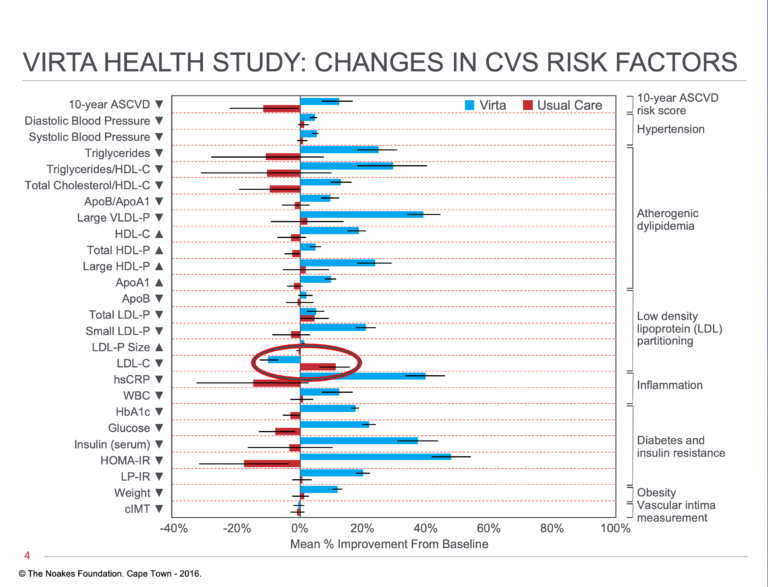
Figure 4: Percent changes in multiple cardiovascular risk factors measured in persons with T2DM receiving either the Virta Health intervention or usual care. All changes favor the Virta Health group, with perhaps one exception (circled) — persons in the usual care group show a reduction in blood LDL-cholesterol concentrations, whereas these concentrations rose in persons on the Virta Health intervention. However, as in the studies from the Volek research group (49, 53), this change was due to an increase in the size of the LDL-cholesterol particles. This is not considered an adverse health consequence. Redrawn from reference 64.
The sole exception was the increase in blood LDL-cholesterol concentrations in the Virta Health group. However, the long-term health consequences of this change are uncertain. For example, the Framingham study, which was designed specifically to determine which biological markers might predict future health risk, established that a falling blood cholesterol concentration with age is an indicator of failing, not improving health. In that study (65), falling blood cholesterol concentrations over the study’s first 14 years were found to predict an increased mortality rate over the next 18 years. The study found “a direct association between falling cholesterol levels over the first 14 years and mortality over the following 18 years” (p. 2176). Thus, there was an 11% overall and 14% CVD death rate increase for each 1 mg/dL per year drop in blood cholesterol concentrations. In contrast, there was “a lack of an association of total serum cholesterol measured after age 50 years with overall mortality” (p. 2179).
Additionally, the increase in LDL-cholesterol concentrations in persons eating a low-carbohydrate diet was due to an increase in the number of large LDL-cholesterol particles (54, 55) and was not considered harmful.
In June 2019, the two-year results of the Virta Health study were reported (66). All the benefits already apparent at one year were sustained, and 54% of participants receiving the Virta Health intervention had reversed their T2DM; another 18% were in remission. No patient in usual care showed this response. Overall medication use fell from 55% to 25% in the Virta Health group so that daily insulin use fell from an average of 89 to 19 units/day.
Another recent study found evidence of significant improvements in non-invasive markers of liver fat and fibrosis (non-alcoholic fatty liver disease) in persons receiving the Virta Health intervention and no change in the usual care group (67).
Summary
Atkins is the single strongest thread binding all those on the North American continent who have promoted the low-carbohydrate diet over the past century.
He is the link from Icelandic Arctic explorer Vilhjalmur Stefansson to the work of the Virta Health company, guided by Finnish entrepreneur and ultradistance athletic explorer Sami Inkinen.
Most importantly, the definitive studies of Westman, Phinney, and Volek, together with those performed by the Virta Health company, prove that Atkins was correct.
So when the 100-millionth patient with T2DM is “reversed” by the Virta Health intervention sometime before 2025, Atkins’s legacy will become one of the most significant in the history of modern medicine.
But what of Reaven? What will be his monumental contribution? How will he be remembered?
We take up that story next.
Additional Reading
Professor T.D. Noakes (OMS, MBChB, MD, D.Sc., Ph.D.[hc], FACSM, [hon] FFSEM UK, [hon] FFSEM Ire) studied at the University of Cape Town (UCT), obtaining a MBChB degree and an MD and DSc (Med) in Exercise Science. He is now an Emeritus Professor at UCT, following his retirement from the Research Unit of Exercise Science and Sports Medicine. In 1995, he was a co-founder of the now-prestigious Sports Science Institute of South Africa (SSISA). He has been rated an A1 scientist by the National Research Foundation of SA (NRF) for a second five-year term. In 2008, he received the Order of Mapungubwe, Silver, from the President of South Africa for his “excellent contribution in the field of sports and the science of physical exercise.”
Noakes has published more than 750 scientific books and articles. He has been cited more than 16,000 times in scientific literature and has an H-index of 71. He has won numerous awards over the years and made himself available on many editorial boards. He has authored many books, including Lore of Running (4th Edition), considered to be the “bible” for runners; his autobiography, Challenging Beliefs: Memoirs of a Career; Waterlogged: The Serious Problem of Overhydration in Endurance Sports (in 2012); and The Real Meal Revolution (in 2013).
Following the publication of the best-selling The Real Meal Revolution, he founded The Noakes Foundation, the focus of which is to support high quality research of the low-carbohydrate, high-fat diet, especially for those with insulin resistance.
He is highly acclaimed in his field and, at age 67, still is physically active, taking part in races up to 21 km as well as regular CrossFit training.
References
- Donaldson BF, Heyd CG. Strong Medicine. Garden City, New York: Doubleday and Company, Inc.,1962.
- Rogak L. Dr Robert Atkins: The True Story of the Man Behind the War on Carbohydrates. London: Robson Books, 2005.
- Duncan GG, Jenson WK, Fraser RI. Correction and control of intractable obesity. Practical application of intermittent periods of total fasting. JAMA 181(1962): 309-312.
- Duncan GG. Intermittent fasts in the correction and control of intractable obesity. Trans Am Clin Climatol Assoc. 74(1963): 121-129.
- Duncan GG, Duncan TG, Schless GL, et al. Contraindications and therapeutic results of fasting in obese patients. Ann NY Acad Sci. 131(1965): 632-636.
- Azar GJ, Bloom WL. Similarities of carbohydrate deficiency and fasting II. Ketones, nonesterified fatty acids, and nitrogen excretion. Arch Intern Med. 112(1963): 338-343.
- Taubes G. Good Calories, Bad Calories: Fats, Carbs and the Controversial Science of Diet and Health. New York: Anchor Books, 2007.
- Stefansson V. My Life With the Eskimo. New York: Macmillan, 1912.
- Stefansson V. The Friendly Arctic. New York: Macmillan, 1921.
- Stefansson V. Not by Bread Alone. New York: Macmillan, 1946.
- Stefansson V. Cancer: Disease of Civilization? An Anthropological and Historical Study. New York: Hill and Wang, Inc., 1960.
- Stefansson V. Discovery – The Autobiography of Vilhjalmur Stefansson. New York: McGraw-Hill Book Company, 1964.
- McClellan WS, Du Bois EF. Prolonged meat diet with a study of kidney function and ketosis. J Biol Chem. 87(1930): 651-668.
- Pennington AW. Obesity in industry; the problem and its solution. Industr Med Surg. 18(1949): 259-260.
- Pennington AW. The use of fat in a weight reducing diet. Del Med J. 23(1951): 79-86.
- Pennington AW. Caloric requirement of the obese. Industr Med Surg. 20(1951): 267-271.
- Pennington AW. A reorientation on obesity. New Engl J Med. 23(1953): 959-964.
- Pennington AW. An alternate approach to the problem of obesity. Am J Clin Nutr. 1(1953): 100-106.
- Pennington AW. Treatment of obesity with calorically unrestricted diets. J Clin Nutr. 1(1953): 343-348.
- Pennington AW. Obesity: Overnutrition or disease of metabolism? Am J Dig Dis. 20(1953): 268-274.
- Pennington AW. Treatment of obesity: Developments in the past 150 years. Am J Dig Dis. 21(1954): 65-69.
- Pennington AW. Pathophysiology of obesity. Am J Dig Dis. 21(1954): 69-73.
- Pennington AW. Pyruvic acid metabolism in obesity. Am J Dig Dis. 22(1955): 33-37.
- Bauer J. Obesity. Its pathogenesis, etiology and treatment. Arch Int Med. 67(1951): 968-994.
- Leith W. Experiences with the Pennington diet in the management of obesity. Can J Med Assoc. 84(1961): 1411-1414.
- Thorpe GL. Treating overweight patients. JAMA 165(1957): 1361-1366.
- Kerwick A, Pawan GLS. Weight loss in the obese. A preliminary communication. Arch Middlx Hosp. 3(1953): 139-149.
- Kerwick A, Pawan GLS. Caloric intake in relation to body-weight changes in the obese. Lancet 271(1956): 155-161.
- Kerwick A, Pawan GLS. Metabolic study in human obesity with isocaloric diets high in fat, protein or carbohydrate. Metabolism 6(1957): 447-460.
- Yang M-U, Van Itallie TB. Composition of weight lost during short-term weight reduction. Metabolic responses of obese subjects to starvation and low-calorie ketogenic and nonketogenic diets. J Clin Invest. 58(1976): 722-730.
- Rocchini AP, Katch V, Kveselis D, et al. Insulin and renal sodium retention in obese adolescents. Hypertension 14(1989): 367-374.
- Atkins RC. Dr Atkins’ Diet Revolution: The High Calorie Way to Stay Thin Forever. New York: David McKay Company Inc., 1972.
- Westman EC, Yancy WS, Edman JS, et al. Effect of a 6-month adherence to a very low carbohydrate diet program. Am J Med. 113(2002): 30-36.
- Yancy WS, Olsen MR, Guyton JR, et al. A low-carbohydrate, ketogenic diet versus a low-fat diet to treat obesity and hyperlipidemia. A randomized controlled trial. Ann Intern Med. 140(2004): 769-777.
- Media Advisory. American Heart Association. Available here.
- White PL. A critique of low-carbohydrate ketogenic weight reduction regimens. A review of Dr Atkins’ Diet Revolution. JAMA 224(1973): 1415-1419.
- Yudkin J. The causes and cure of obesity. Lancet ii(1959): 1135-1138.
- Yudkin J. The treatment of obesity. Med Press 19(July 1961): 64-68.
- Yudkin J, Carey M. The treatment of obesity by the “high fat” diet. The inevitability of calories. Lancet ii(1960): 939-941.
- Stock AL, Yudkin J. Nutrient intake of subjects on low carbohydrate diet used in the treatment of obesity. Am J Clin Nutr. 23(1970): 948-952.
- Yudkin J. The low-carbohydrate diet in the treatment of obesity. Postgrad Med. 51(1972): 151-154.
- Yancy WS, Foy M, Chalecki AM et al. A low-carbohydrate, ketogenic diet to treat type 2 diabetes. Nutr Metab. 2(2005): 34.
- Newburgh LH, Marsh PL. The use of a high fat diet in the treatment of diabetes mellitus. First paper. Arch Int Med. 26(1920): 647-662.
- Newburgh LH, Marsh PL. The use of a high fat diet in the treatment of diabetes mellitus. Second paper. Blood sugar. Arch Intern Med. 27(1921): 699-705.
- Newburgh LH, Marsh PL. Further observations on the use of a high fat diet in the treatment of diabetes mellitus. Arch Intern Med. 31(1923): 455-490.
- Newburgh LH. The dietetic treatment of diabetes mellitus. A restatement of the fundamental principles. Arch Intern Med. 2(1929): 645-649.
- Newburgh LH, Waller DS. Studies of diabetes mellitus. Evidence that the disability is concerned solely with the metabolism of glucose. The mode of action of insulin. J Clin Invest. 11(1932): 995-1002.
- Newburgh LH. The foundation of diet therapy. Clinical lecture at Atlantic City session. JAMA 105(1935): 1034-1037.
- Newburgh LH, Conn JW. A new interpretation of hyperglycemia in obese middle aged persons. JAMA 112(1939): 7.
- Newburg LH. Control of the hyperglycemia of obese “diabetics” by weight reduction. Ann Intern Med. 17(1942): 935-942.
- Wall JR, Pyke DA, Oakley WG. Effect of carbohydrate restriction in obese diabetics: Relationship of control to weight loss. Brit Med J. 1(1973): 577-578.
- Volek JS, Sharman MJ, Gomez AL, et al. An isoenergetic very low carbohydrate diet improves serum HDL cholesterol and triacylglycerol concentrations, the total cholesterol to HDL cholesterol ratio and postprandial lipemic responses compared with a low fat diet in normal weight, normolipidemic women. J Nutr. 133(2003): 2756-2761.
- Volek JS, Sharman MJ, Gomez AL, et al. Comparison of energy restricted very low -carbohydrate and low-fat diets on weight loss and body composition in overweight men and women. Nutr Metab. 1(2004): 13.
- Volek JS, Fernandez ML, Feinman RD, et al. Dietary carbohydrate restriction induces a unique metabolic state positively affecting atherogenic dyslipidemia, fatty acid profiling, and metabolic syndrome. Prog Lipid Res. 47(2008): 307-318.
- Volek JS, Phinney SD, Forsythe CE, et al. Carbohydrate restriction has a more favourable impact on the metabolic syndrome than a low fat diet. Lipids 44(2009): 297-309.
- Forsythe CD, Phinney SD, Feinman RD, et al. Limited effect of dietary saturated fat on plasma saturated fat in the context of a low carbohydrate diet. Lipids 45(2010): 947-962.
- Volk BM, Kunces LJ, Freidenreich DJ, et al. Effect of step-wise increases in dietary carbohydrate on circulating saturated fatty acids and palmitoleic acid in adults with metabolic syndrome. PLoS ONE 9(11): e113605.
- Hyde PH, Sapper TN, Crabtree CD, et al. Dietary carbohydrate restriction improves metabolic syndrome independent of weight loss. JCI Insight 4.12(2019): e128308.
- Noakes TD. It’s the insulin resistance, stupid: Part 2. CrossFit.com. 17 July 2019. Available here.
- Loring M, Inkinen S. An ccean odyssey. Babson. Winter 2015.
- Cava MD. Couple row across Pacific doesn’t divorce. USA Today. 6 August 2014.
- McKenzie AL, Hallberg SJ, Creighton BC, et al. A novel intervention including individualized nutritional recommendations reduces haemoglobin A1c level, medication use, and weight in type 2 diabetes. JMIR Diabetes 2.1(2017): e5.
- Hallberg SJ, McKenzie AL, Williams PT. Effectiveness and safety of a novel care model for the management of type 2 diabetes at 1 year: An open-label, non-randomized, controlled study. Diabetes Ther. 9.2(April 2018): 583-612.
- Bhanpuri NH, Hallberg SJ, Williams PT, et al. Cardiovascular disease risk factor responses to a type 2 diabetes care model including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: an open label, non-randomized, controlled study. Cardiovasc Diabetol. 17(2018): 56.
- Anderson K, Castelli WP, Levy D. Cholesterol and mortality. 30 years of follow-up from the Framingham study. JAMA 257(1987): 2176-2180.
- Athinarayanan SJ, Adams RN, Hallberg SJ, et al. Long term effects of a novel continuous remote care intervention including nutritional ketosis for the management of type 2 diabetes: A 2-year non-randomized clinical trial. Frontiers Endocrinol. 10(2019): Article 10.
- Vilar-Gomez E, Athinarayanan SJ, Adams RN, et al. Post hoc analyses of surrogate markers of non-alcoholic fatty liver disease (NAFLD) and liver fibrosis in patients with type 2 diabetes in a digitally supported continuous care intervention: an open-label, non-randomized controlled study. BMJ Open 9.2(Feb. 2019)