This 2017 paper reviewed trials of fasting in humans and animals.
Fasting regimens fall into three general categories:
- Intermittent fasting (IF) involves short fasts of less than 48 hours.
- Periodic fasting (PF) involves fasting longer than two days.
- Time-restricted feeding (TRF) involves limiting food intake to only certain hours each day, which extends the amount of time spent in a fasted state.
A specific form of intermittent fasting called alternate-day fasting (ADF) involves fasting or significantly reducing food intake every other day.
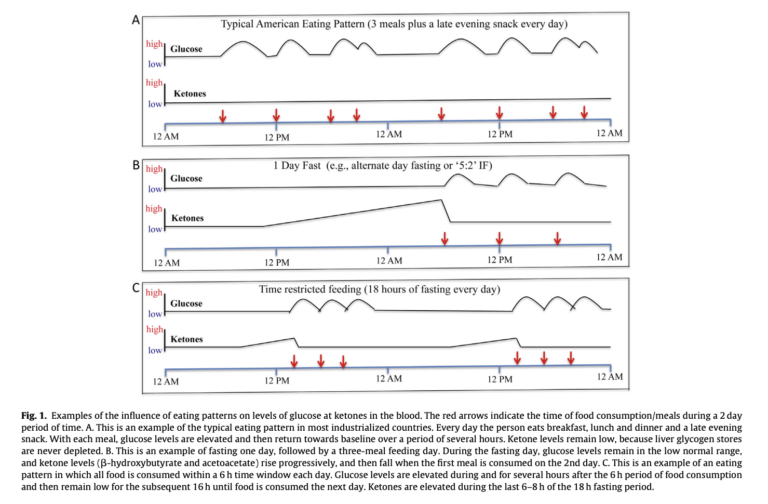
Certain biological effects are shared across all forms of fasting:
- Blood glucose levels stabilize in the low-normal range.
- Glycogen stores are reduced or depleted.
- Fatty acids are mobilized and ketones are produced.
- Circulating leptin levels decrease, and adiponectin levels increase.
These metabolic changes do not occur or occur to a much lesser extent with moderate caloric restriction; they are therefore relatively unique to fasting. Longer fasts increase the magnitude of these changes, as shown in Figure 1 above. Longer fasts, in particular, lead to greater depth of ketosis and greater clearance of energetic stores (i.e., fat and glycogen stores).
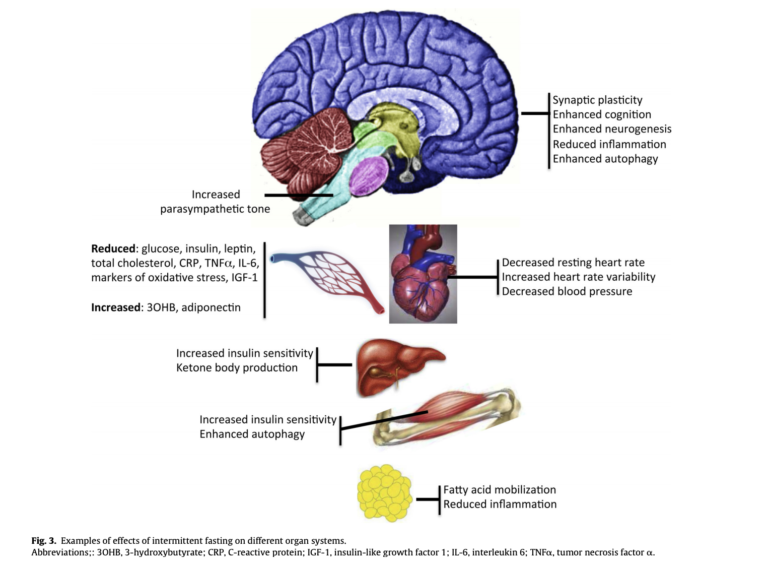
Our understanding of the clinical impacts of fasting is mostly drawn from rat and mouse research. In animal models, intermittent fasting and/or alternate-day fasting have been linked to the following:
- Greater increases in insulin sensitivity and glucose tolerance than moderate caloric restriction, even when similar weight loss occurs
- Reduced resting heart rate and blood pressure
- Normalization of glucose, insulin, and leptin levels in diabetic mice, and reduced risk of diabetes in susceptible mouse models
- Reduced liver fat content
- Reduced risk of Alzheimer’s-like cognitive impairment in certain mouse models
Figure 3 illustrates the impact of intermittent fasting on various organ systems. The metabolic improvements seen in diabetic mice are thought to be linked to improvements in liver and muscle insulin sensitivity, which increase whole-body insulin sensitivity and glucose control.
Existing trials have not, however, compared the impact of different forms of fasting on these or other biomarkers. Additionally, most of this research was done in transgenic mouse models and so may not extrapolate to humans.
Human research is more limited. IF has been repeatedly shown to improve body weight, body fat, and triglycerides, but few of these studies have compared fasting directly to caloric restriction. In diabetic subjects, existing research suggests equal or greater improvements in insulin resistance, HbA1c, and whole-body glucose disposal due to intermittent fasting (compared to similar levels of caloric restriction), but this research is limited, and results have been inconsistent. ADF has been shown to reduce resting heart rate, fasting glucose and insulin levels, blood pressure, and triglycerides while increasing LDL particle size — all of which would reduce cardiovascular risk. However, the direct effect on cardiovascular outcomes has not yet been studied. Similarly, IF reduces IGF-1 levels, which may reduce cancer risk, but there have been no studies showing whether long-term fasting has true preventative effects.
Overall, the authors present a promising but clearly preliminary body of evidence supporting the clinical benefits of various forms of fasting. Existing comparisons between fasting and caloric restriction consistently indicate fasting has equal or greater benefits on a variety of metabolic markers, particularly liver and muscle (and so whole-body) insulin sensitivity. Preliminary evidence suggests fasting may reduce risk of neurodegenerative disease and cancer. Future research and practice will illustrate whether these shifts lead to improvements in hard clinical outcomes such as diabetes remission or heart disease prevention.
Comments on Impact of Intermittent Fasting on Health and Disease Processes
It is clear that society as a whole is suffering from an over abundance of highly processed foods with readily available calories. Couple that with the body of research and pilot studies showing the various benefits of intermittent fasting and calorie restriction and it becomes imperative that we need to make some feeding changes that inevitably restrict these calories. For me, I like time restricted feeding because it meshes with my lifestyle, but I think there are a number of solid choices. But, even if it all seemed to overwhelming, everyone can mindfully increase the interval between the last meal of the day and the first meal of the day.
Impact of Intermittent Fasting on Health and Disease Processes
1