Question: How common are professional conflicts of interest within the leadership of U.S. professional medical associations?
Takeaway: This 2020 analysis found more than three-quarters of those serving on the boards of prominent professional medical associations received some form of industry funding, with a median annual income of $31,805 from industry.
This 2020 paper reviews the frequency and magnitude of financial ties between the leadership of major U.S. professional medical associations and industry.
Recent research has brought increasing scrutiny of the role of conflicts of interest in medical research, guidance, and practice (1). Sponsored research is more likely to favor the sponsor’s work (2); sponsored education leads to greater prescription of sponsors’ drugs (3); and guideline panels are frequently staffed by individuals with financial conflicts of interest, though these conflicts are rarely fully disclosed (4). Simultaneously, others have argued as much as 20% of health-care spending may be unnecessary or misspent (5). Industry influence may directly contribute to this misspending (6). This paper sought to provide the most comprehensive analysis to date of the extent of the financial conflicts of interest among those serving on the boards of the most influential professional medical organizations in the United States.
Since 2013, the U.S. government has maintained the Open Payments Database, which documents payments between doctors and industry (7). The authors of this paper surveyed U.S.-based doctors to identify the most influential medical organization for each of the 10 costliest medical conditions (in terms of total medical spending). The selected organizations are shown in the table below. Any members of the board of directors, or any other primary governing body as applicable, were considered members of leadership. Notably, this paper only surveyed organizations primarily led by and oriented toward medical doctors and excluded organizations with a substantial advocacy focus like the American Heart Association.
The authors identified 328 leaders across these 10 organizations, 235 of whom (72%) received some payment from industry in the year surveyed (i.e., during their term as a leader), the four years prior, or the year subsequent. The survey indicated 80% of medical doctors had some financial conflict. Payments to these leaders totaled $104.6-129.9 million in research grants, $24.8 million of which was distributed for general payments (speaking, consulting, royalties, etc.) and the remainder for various smaller miscellaneous payments. The median payment received was $31,805.
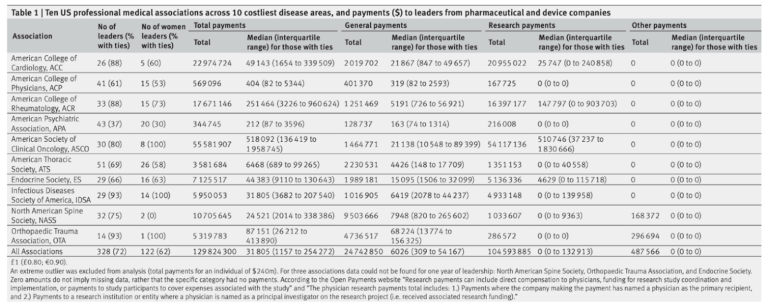
Table 1: Payments from industry to board members at 10 leading professional medical associations
No organization was entirely free of financial ties, but the financial significance of these conflicts varied greatly. Median payments to leadership of the American College of Physicians and American Psychiatric Association were $404 and $212, respectively. Conversely, median industry payments to leadership of the American Society of Clinical Oncology and American College of Rheumatology averaged $518,000 and $251,000. The share of leadership with conflicts similarly varied from as low as 37% (American Psychiatric Association) to as high as 93% (Infectious Disease Society of America and Orthopedic Trauma Association). The largest recipients of research funding were the leadership of the American Society of Clinical Oncology ($54 million in total) and American College of Cardiology ($21 million in total). Guidelines promoted by these organizations frequently support increased use of health care — a trend that may be directly influenced by these conflicts.
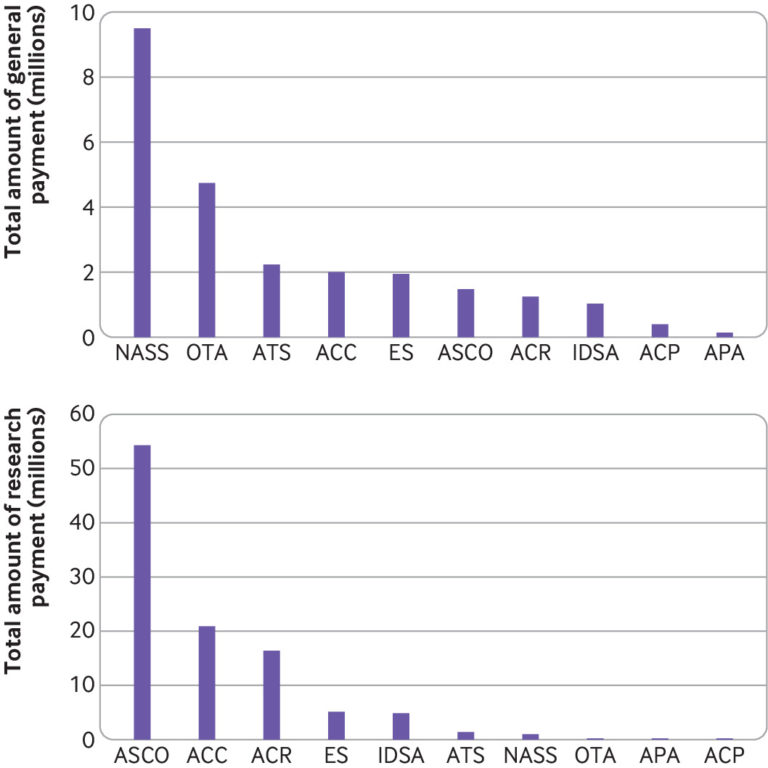
Figure 2: General and research payments to leaders of 10 professional medical associations. General payments include for consultancies, travel, food, and beverages, and royalties. IDSA=Infectious Diseases Society of America; OTA=Orthopaedic Trauma Association; ACC=American College of Cardiology; ACR=American College of Rheumatology; ASCO=American Society of Clinical Oncology; NASS=North American Spine Society; ATS=American Thoracic Society; ES=Endocrine Society; ACP=American College of Physicians; APA=American Psychiatric Association
Previous research has had similar findings. A Japanese study found 87% of the leadership of 19 Japanese medical associations received industry funding (8). A 2014 study found 51% of U.S. medical journal editors received general payments from industry, and 20% received research payments (9). A 2016 study found 87% of U.S. gastroenterologists received industry payments (10).
This study found pervasive conflicts of interest among the leadership of leading U.S. medical organizations, which reveals the level of industry influence may be substantial.
Notes
- Conflict of interest in medical research, education, and practice; Commercial interests, transparency, and independence: a call for submissions; Association between industry affiliation and position on cardiovascular risk with rosiglitazone: Cross sectional systematic review; Conflict of interest disclosure in biomedical research: A review of current practices, biases, and the role of public registries in improving transparency
- Industry sponsorship and research outcome
- Pharmaceutical industry-sponsored meals and physician prescribing patterns for Medicare beneficiaries
- Expanding disease definitions in guidelines and expert panel ties to industry: a cross-sectional study of common conditions in the United States; Professional Medical Associations and Divestiture from Industry: An Ethical Imperative for Pain Society Leadership
- Eliminating waste in US health care; OECD: Tackling wasteful spending on health
- Mapping the drivers of overdiagnosis to potential solutions
- Centres for Medicare & Medicaid Services. Open Payments database
- Pharmaceutical company payments to executive board members of professional medical associations in Japan
- Payments by US pharmaceutical and medical device manufacturers to US medical journal editors: retrospective observational study
- Assessment of pharmaceutical company and device manufacturer payments to gastroenterologists and their participation in clinical practice guideline panels
Financial Ties Between Leaders of Influential U.S. Professional Medical Associations and Industry