Part I: Basics
The history of diabetes and its treatment will be a gripping tale of brilliant scientific discovery and remarkable intellectual triumph. The discovery of the hormone insulin changed everything, and its evolution and applications still fascinate. The story is still being written, however, and there will also be a story of ignorance, obstinacy, and other very human behaviors — Frederick Banting, whose insight and determination led to the discovery of insulin, spent much of his life in resentment that his coworker received too little credit and others, too much. Overall, significant human suffering will be constantly present — diabetes can be a terrible disease, a disruptor of many lives, a major cause of blindness and amputations — and the suffering is made worse by the fact that for many, there is a cure, a cure resisted by the medical profession. The various forms of diabetes represent disruptions of carbohydrate metabolism in which insulin appears as the key player. Restricting carbohydrate, the obvious and intuitive treatment, has oddly produced ugly controversy. Real compassion and dedication from individual doctors and health workers are present but remain overshadowed, as they usually do in such chapters, by the dark side of the story.
Under normal conditions, ingested carbohydrate leads to an increase in glucose (sugar) in the blood. Glucose is the major stimulus for secretion of insulin from the pancreas. Blood glucose must be maintained at a more or less constant level because it is a required fuel for some cells, particularly those of the brain and nervous system, and too much is also not good because glucose is chemically reactive. Insulin regulates blood glucose by suppressing production from the liver, enhancing uptake into other tissues, and stimulating the synthesis, storage, and production of glucose when none is present in the diet.
There are two major types of diabetes. For both, hyperglycemia (high blood glucose) is the defining feature. In Type 1 diabetes, the cause is a lack or an absence of insulin. Type 2 is less understood, but while insulin is produced, it is not effective at regulating blood sugar. A patient with Type 2 is said to be insulin resistant. The pancreas may try to compensate by producing more hormone, and in the end, deteriorating pancreatic function may add to further problems. Both forms of diabetes represent carbohydrate intolerance, and before the disease was understood — insulin was pinpointed as the cause in the 1920s — the only treatment was to reduce carbohydrate in the diet (or to undertake a fast, the main effect of which may have been removing the carbohydrate). Cutting down on carbs remains the best treatment. The immediate reaction to the discovery of insulin was to assume injecting the hormone would fix everything. The effects were, in fact, miraculous. Children who were frail and dying — untreated Type 1 patients are generally thin from not being able to use ingested carbohydrate — were suddenly returned to life. Doctors believed people with diabetes could now eat a normal diet; that is, one with carbohydrate, as long as they “covered” the carbohydrate with insulin (many doctors still talk that way), but it was not that simple. Injecting insulin was a tricky business. It still is. Because blood glucose must be maintained at more or less constant levels, the injected insulin must match the amount of glucose that is to be controlled. While hyperglycemia is a risk, bringing glucose down too quickly or too thoroughly can be worse. Hypoglycemia (low blood glucose) can be mild, but in the extreme can be life-threatening because of the brain and nervous system’s demands for glucose. The timing and fluctuations of administered glucose can rarely duplicate the normal control of the built-in glucose-insulin system. Here’s a picture of the responses a kid with Type 1 diabetes has to insulin when on a normal diet and on a low-carbohydrate diet:
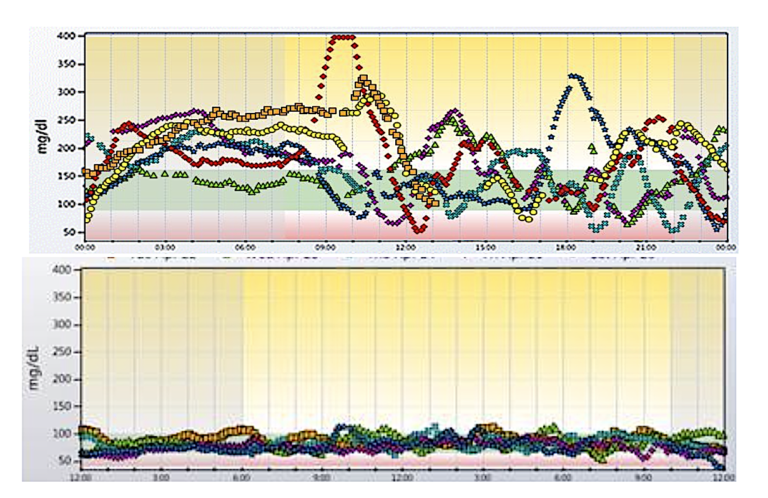
Figure 1: Blood glucose curves. Top: Normal diet. Bottom: Low-carbohydrate diet. (Note: Cutoff for normal glucose is considered to be less than 100 mg/dL) Courtesy R. D. Dikeman.
Diabetes is about carbohydrate intolerance, but it is much bigger than that. Insulin is a kind of master hormone. While it is only one of many hormones — even in the control of blood glucose — it exerts major control over fat and protein metabolism and has major effects on the nervous system. I usually describe metabolism as analogous to American football. There are at least 22 things going on at once, but we can understand a lot by following the quarterback as they do on TV. Not every play depends on the quarterback, and occasionally a good fake will fool the camera man, but it is generally a good place to start. That is why it may help to know about diabetes, even if you are not suffering from the disease. Insulin controls numerous processes — the major reason people with diabetes do not take their insulin is fear of weight gain caused by the anabolic (building up) effect of insulin. The figure below shows the effects of diabetes in the U.S. population. Technical and intellectual advances in medicine undoubtedly account for the significant reductions over the years, but curiously, the risks seem to be on the rise again.
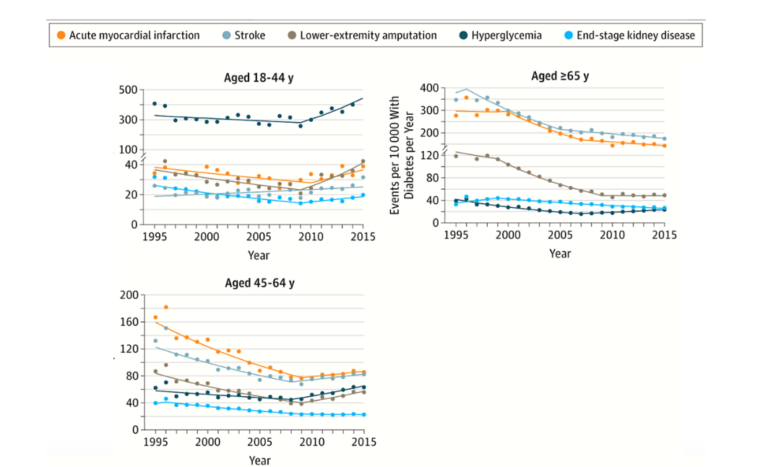
Figure 2: Hospitalizations for major diabetes-related complications. (Data from U.S. CDC. Redrawn from Gregg EW, Hora I, Benoit SR. Resurgence in diabetes-related complications. JAMA online, April 15, 2019.)
Pervasive health effects and great patient harm, not to mention swelling health costs, suggest we should pursue treatment and cure with moonshot dedication. But something has gone terribly wrong. Although much research has pointed to a low-carbohydrate or ketogenic diet as the best treatment — often a real cure for Type 2, and as in the figure above, a powerful adjunct for insulin in Type 1 — the approach is far from being embraced by establishment medicine and instead has been resisted with remarkable vigor.
Looking ahead, I will describe the results that led to our current understanding and the current promise for people with diabetes. I will try to figure out what has caused the political and intellectual disturbance in the medical field and what we can do about it. The value of carbohydrate restriction is encapsulated in our multi-authored review, succinctly described in a previous CrossFit post. The appearance in 2018 of several landmark studies supports the viewpoint in the review. At the same time, a couple of bizarre, irrational blowbacks from the orthodoxy appeared, purporting to tell us that, despite the numerous papers showing great benefit, low-carbohydrate/ketogenic diets will actually kill us.
How is it possible that different groups of physicians and researchers should hold such opposite points of view? The scientific and medical literature is supposed to be the gatekeeper on what is real or, as the cliché has it, evidence-based science. How can the individual patient cope with the information? How do you read a scientific paper to decide if it’s real? That’s next.
 Richard David Feinman, Ph.D., is a professor of cell biology at the State University of New York Downstate Medical Center in Brooklyn, where he has been a pioneer in incorporating nutrition into the biochemistry curriculum. A graduate of the University of Rochester and the University of Oregon, Dr. Feinman has published numerous scientific and popular papers. He is the founder and former co-editor-in-chief (2004–2009) of the journal Nutrition & Metabolism. He is currently researching the application of ketogenic diets to cancer.
Richard David Feinman, Ph.D., is a professor of cell biology at the State University of New York Downstate Medical Center in Brooklyn, where he has been a pioneer in incorporating nutrition into the biochemistry curriculum. A graduate of the University of Rochester and the University of Oregon, Dr. Feinman has published numerous scientific and popular papers. He is the founder and former co-editor-in-chief (2004–2009) of the journal Nutrition & Metabolism. He is currently researching the application of ketogenic diets to cancer.