Miriam Vos (Emory) and Joel Lavine (Columbia) present the evidence linking fructose to fatty liver disease in this 2013 review.
A healthy liver holds relatively little fat (<5.5% fat fraction). Fatty liver disease occurs when the liver stores too much fat, either by producing and importing too much, or by burning and exporting too little. Nonalcoholic fatty liver disease (NAFLD) is marked in particular by higher circulating fatty acids, greater liver fatty acid production (de novo lipogenesis, or DNL), and delayed liver fatty acid export.
When fructose is consumed, it passes through the small intestine and quickly is taken up by the liver, where it is either burned or converted to free fatty acids and/or glycerol and glycogen. Fructose has been shown to increase liver and visceral fat: the former through increased DNL and the latter as a potential consequence of liver insulin resistance (fatty livers become insulin resistant). Fructose similarly increases circulating triglyceride levels by increasing fat production within the liver. These effects may be exacerbated by the effects of fructose on the gut microbiome, which can trigger additional liver inflammation and the development or progression of NAFLD.
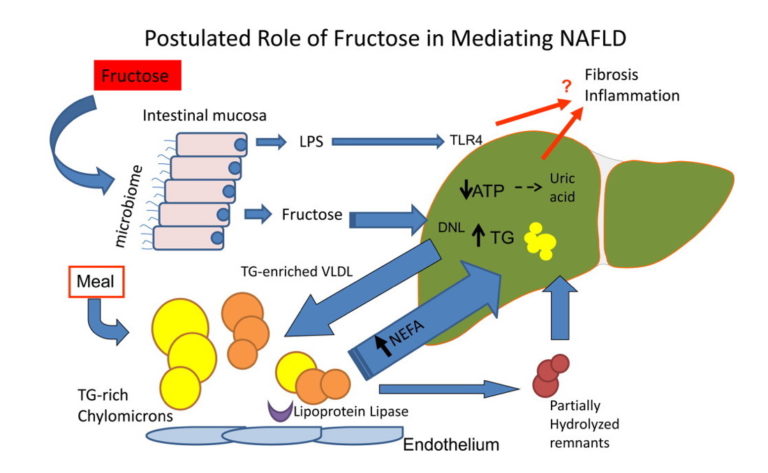
Figure 1: In NAFLD, ingested fructose may alter the microbiome, increasing movement of endotoxin into the portal system because of increased permeability of tight junctions. Endotoxin and fructose enter the liver where endotoxin increases inflammation and insulin resistance through activation of Toll‐like receptor 4 (TLR4). Fructose is rapidly metabolized, consuming adenosine triphosphate (ATP), which may result in increased adenosine monophosphate (AMP) and conversion to uric acid. Excess triglyceride produced through stimulation of de novolipogenesis (DNL) is packaged onto large, TG‐rich very low density lipoproteins (VLDL) or in the setting of imbalance can result in increased steatosis in the liver. Steatosis may also be driven by increased return of nonesterified free fatty acids (NEFA) from adipose tissue. From “Dietary fructose in nonalcoholic fatty liver disease“.
Patients with NAFLD tend to consume more fructose than their peers, and those with more severe NAFLD consume more than those with less severe NAFLD. However, Vos and Lavine note that evidence from direct clinical trials has been inconsistent and only clearly indicates that fructose increases liver fat content in the context of a hypercaloric diet. They conclude, however, “While the understanding of the role of fructose in NAFLD is evolving, the evidence demonstrating increased VAT, hypertriglyceridemia, and insulin resistance from high fructose is sufficient to support decreasing consumption as a clinical recommendation for patients with NAFLD.”
Note: This review was written in 2013. Subsequent evidence, to be presented elsewhere on CrossFit.com, has more broadly illustrated a direct link between fructose consumption and NAFLD.