This 2019 review briefly summarizes evidence linking fructose to metabolic syndrome.
Over the past 40 years, sugar intake (and thus fructose intake) has increased dramatically in Western diets, rising to 15-17% of total daily caloric consumption (1). This rise comes alongside increasing evidence linking fructose to diabetes, fatty liver disease, and cardiometabolic risk factors (2).
Fructose most directly contributes to the accumulation of fat in the liver and thus the development of nonalcoholic fatty liver disease (NAFLD). The liver accumulates fat when its total fat intake — from a combination of circulating fatty acids, dietary fat, and de novo lipogenesis (fat production by the liver) — exceeds the total amount of fat it burns or exports as lipoproteins (as VLDL). Fructose is directly metabolized by the liver in an insulin-independent fashion that increases de novo lipogenesis and the liver’s fat burden. By increasing total fat flux into the liver, fructose increases triglyceride-rich lipoprotein production, leading to a worse lipid profile marked by higher apoB and smaller, denser LDL particles (3). In higher doses, fructose also drives liver fat accumulation. Accordingly, the rise in fructose consumption in the U.S. has occurred alongside an equally dramatic rise in the rates of NAFLD, which has become the leading cause of liver disease in Western countries and directly increases the risk of metabolic syndrome and cardiovascular disease (4).
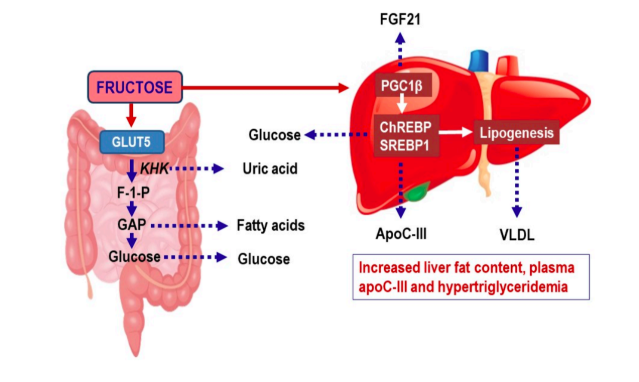
Fructose also may contribute to metabolic syndrome and increased cardiovascular risk by increasing production of uric acid, an independent biomarker for various metabolic disease states (5).
The most compelling direct clinical evidence suggesting fructose plays a causative role in these diseases has come from studies of fructose restriction. Multiple studies have shown that removing fructose from the diet and/or dramatically reducing sugar consumption among children and adults leads to a rapid decrease in liver fat accumulation and improvement of markers of cardiovascular and diabetes risk (6). Weight loss in all forms leads to liver fat clearance, but the impact of fructose restriction (and in some of these studies, carbohydrate restriction) is larger and/or more dramatic than that seen from fat restriction or equal restriction of all calories.
This body of evidence, the authors argue, is sufficient to support the specific restriction of fructose to improve health and reduce risk of metabolic disease, particularly in children and other populations who consume large amounts of sugar-sweetened beverages.
References
- Added sugars intake across the distribution of US children and adult consumers
- Crosstalk between nonalcoholic fatty liver disease and the metabolic syndrome; Does nonalcoholic fatty liver disease cause cardiovascular disease?; Fructose metabolism, cardiometabolic risk, and the epidemic of coronary artery disease; Pathways and mechanisms linking dietary components to cardiometabolic disease: Thinking beyond calories
- Fructose consumption: Recent results and their potential implications; Fructose and cardiometabolic health: What the evidence from sugar-sweetened beverages tells us
- Fructose at the crossroads of the metabolic syndrome and obesity epidemics; Fructose metabolism and metabolic disease; Systematic review: The epidemiology and natural history of non-alcoholic fatty liver disease and nonalcoholic steatohepatitis in adults; Epidemiology of non-alcoholic fatty liver disease, NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom and United States for the period 2016-2030; Fructose and NAFLD: The multifaceted aspects of fructose metabolism; Fructose and sugar: A major mediator of non-alcoholic fatty liver disease; From sugar to liver fat and public health: Systems biology driven studies in understanding non-alcoholic fatty liver disease pathogenesis
- Relationship between resistance to insulin-mediated glucose uptake, urinary uric acid clearance, and plasma uric acid concentration; Prevalence of the metabolic syndrome in individuals with hyperuricemia; Serum uric acid: A strong and independent predictor of metabolic syndrome after adjusting for body composition; A possible role of serum uric acid as a marker of metabolic syndrome; Sugar, uric acid and the etiology of diabetes and obesity
- Effects of dietary fructose restriction on liver fat, de novo lipogenesis and insulin kinetics in children with obesity, Dietary fructose in nonalcoholic fatty liver disease; Short-term isocaloric fructose restriction lowers apoC-III levels and yields less atherogenic lipoprotein profiles in children with obesity and metabolic syndrome; Dietary fat and carbohydrates differentially alter insulin sensitivity during caloric restriction; Randomized comparison of reduced fat and reduced carbohydrate hypocaloric diets on intrahepatic fat in overweight and obese human subjects; Effect of a low free sugar diet vs usual diet on nonalcoholic fatty liver disease in adolescent boys; Isocaloric fructose restriction and metabolic improvement in chilren with obesity and metabolic syndrome; Role of dietary fructose and hepatic de novo lipogenesis in fatty liver disease; Conversion of sugar to fat: Is hepatic de novo lipogenesis leading to metabolic syndrome and associated chronic diseases?
Dietary Fructose and the Metabolic Syndrome