Diabetes has been a known risk factor for previous epidemic illnesses including pandemic influenza (1).
Previous research has linked this increased risk to the chronic inflammatory state and immune system imbalance associated with diabetes and other forms of poor metabolic health (2).
This March 2020 study compares the clinical status and prognosis of 37 diabetics to 137 nondiabetics among 174 Wuhan COVID patients. The average age of both nondiabetic and diabetic patients was similar (average of 58 and 61 years old, respectively).
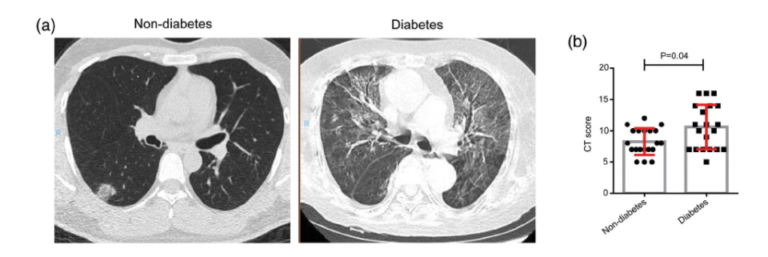
As shown in the figure below, diabetic patients showed more advanced disease as assessed by CT imaging.
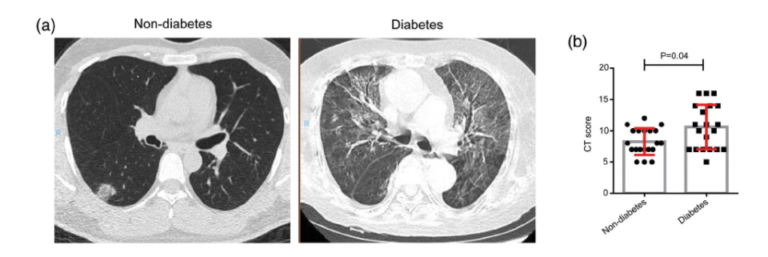
Figure 1: Diabetics display greater disease severity as assessed by CT scan.
Diabetics also showed elevated levels of lactic dehydrogenase (LDH), a-hydroxybutyrate dehydrogenase (HBDH), alanine aminotransferase (ALT), and y-glutamyltransferase (GGT) compared to nondiabetics, though these parameters were elevated relative to baseline in all subjects. Elevated LDH is a marker of myocardial damage; HBDH is a marker of kidney damage; ALT and GGT are markers of liver damage. The elevation of these markers across all subjects is consistent with the understanding that the SARS-CoV-2 virus causes multi-organ damage via binding to ACE2 receptors expressed across many organs. The increased levels of these parameters in diabetics indicates further susceptibility to multi-organ damage.
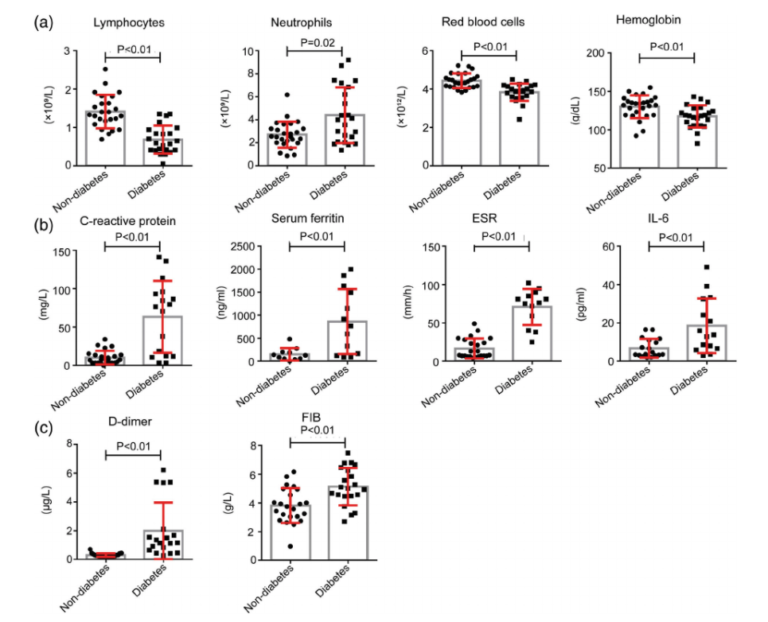
Diabetics also presented with reduced levels of leukocytes and elevated levels of IL-6, ferritin, and C-reactive protein relative to nondiabetics (who also showed less severe distortions in the same direction compared to healthy subjects). This pattern indicates diabetics may have increased risk of the “cytokine storm” that has been a cause of rapid deterioration and death in many COVID-19 patients and played a similar role with SARS and ebola (3). This deterioration may be further exacerbated by the elevated levels of fibrinogen and D-dimer seen in these diabetic patients, which may lead to a harmful hypercoagulable state. Notably, the fact that SARS-CoV-2 may directly infect (and so damage) the pancreas may trigger a vicious cycle, as was seen in SARS (4). This early evidence indicates diabetics infected with SARS-CoV-2 require a higher insulin dose to maintain glucose control, which may worsen the various distorted states noted above.
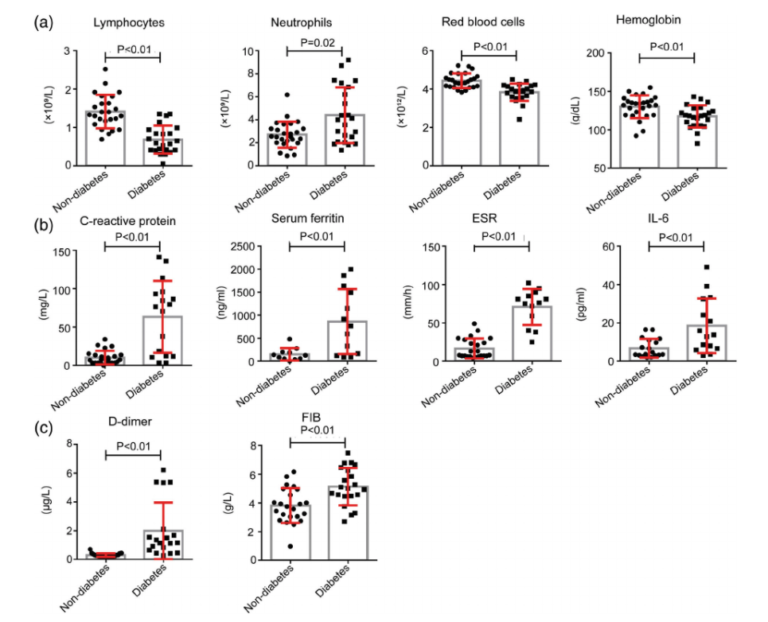
Figure 2: Diabetics show a variety of biomarker changes suggestive of elevated inflammation levels, impaired immune response, and increased vulnerability to a cytokine storm.
The authors conclude the apparent increase in disease severity seen in diabetics is at least in part due to an increased inflammatory response, impaired immune response, and increased susceptibility to multi-organ damage. They repeatedly note similar phenomena have been seen in previous disease pandemics, suggesting diabetes may increase risk for a number of severe diseases.