Question: It is now well established that diabetes increases risk of severe COVID-19. Does hyperglycemia specifically increase COVID risk and/or severity?
Takeaway: This large survey of patients from the Hubei province indicates well-controlled diabetes confers little additional marginal risk of severe COVID (compared to nondiabetics), while poorly controlled diabetes increases disease severity and may increase mortality among hospitalized patients as much as tenfold.
Multiple previous studies, including some summarized on CrossFit.com, have indicated Type 2 diabetes increases risk of severe COVID-19 infection and mortality. Previous research has found diabetes increases risk of morbidity and mortality related to a variety of other infections (1), and in particular, of coronaviruses (2). The specific mechanism by which diabetes increases disease risk is not fully understood but may be related to the deleterious impact of diabetes on pulmonary function (3), immune response(4), and the renin-angiotensin system (5). This study provided the most comprehensive survey to date on the severity of COVID-19 infection among diabetic patients.
Researchers surveyed 7,337 COVID-19 patients in China’s Hubei province. Subjects were excluded if they were younger than 18, older than 75, had incomplete medical records, or had a major preexisting medical condition (including Type 1 diabetes). Of these 7,337 patients, 952 were diabetic. The prevalence of diabetes among this sample (13.0%) was not significantly different from that seen in the general Chinese population (10.9%)(6). Diabetics were slightly older on average (mean age: 62, compared to 53 for nondiabetics) and, as expected, had higher rates of a variety of metabolic comorbidities including hypertension, heart disease, and kidney disease.
At entry, diabetics presented with more severe disease as assessed by a variety of markers. A larger share of diabetics had elevated leukocyte and neutrophil levels, decreased kidney function, increased levels of inflammatory cytokines, and increased D-dimer (coagulation status) than nondiabetics. Among diabetics, 18.8% presented with SpO2 below 95%, compared to 13.2% of nondiabetics. After admission, diabetics were more likely to require a variety of treatments, including antibiotics and antifungals. Diabetics were twice as likely to receive noninvasive ventilation and five times as likely to receive invasive ventilation as nondiabetics. In-hospital mortality was 2.9 times higher in diabetics (7.8%) than nondiabetics (2.7%). After adjusting for age, gender, and disease severity upon admission, the hazard ratio for in-hospital death remained 1.49 for diabetes.
Of the 952 diabetics surveyed, 282 presented with well-controlled blood glucose, while 528 had poorly controlled blood glucose. Across all measures noted above — severity of disease at presentation, treatment requirements, need for ventilation, in-hospital mortality — disease severity and outcomes among diabetics with well-controlled blood glucose were similar to, and in some cases better than, those seen among nondiabetics. Conversely, diabetics with poorly controlled blood glucose had a significantly worse prognosis across all measures. Invasive ventilation was required in 0.0% of those with well-controlled diabetes but 4.2% of those with poor control. In-hospital mortality was 1.1% among the well-controlled and 11.0% among the poorly controlled. This increased mortality was related to increased rates of a variety of severe comorbidities among those with poorly controlled diabetes, including significantly higher rates of ARDS, acute heart injury, and acute kidney injury.
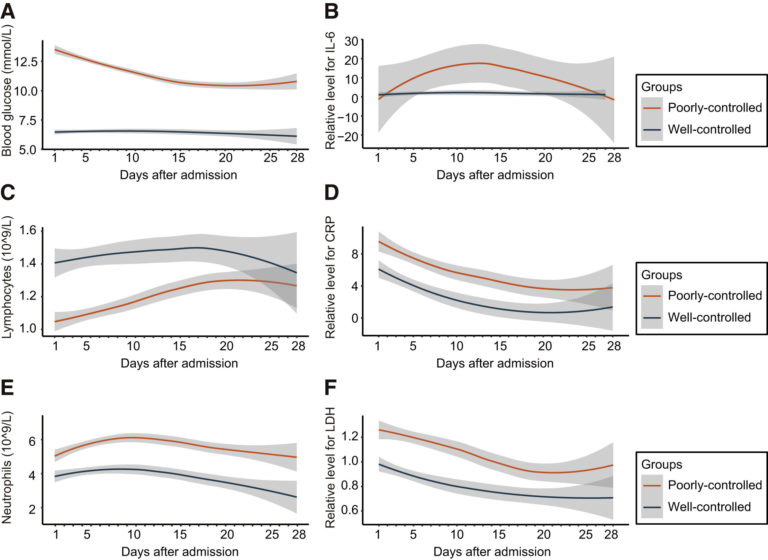
Figure 1: Curves illustrating patterns of multiple markers of immune response and disease severity in those with poorly controlled versus well-controlled diabetes
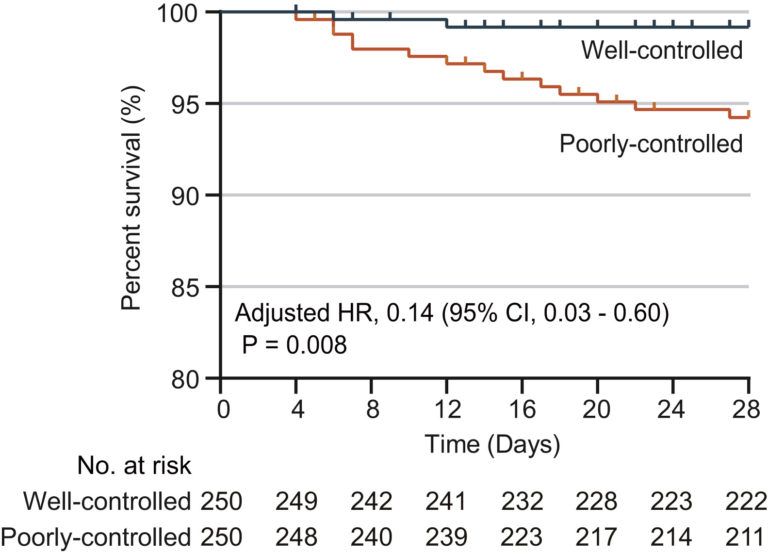
Figure 2: Survival curve for those with well-controlled compared to poorly controlled diabetes
To isolate the effect of glycemic control specifically, researchers compared the disease outcomes of 250 subjects with well-controlled diabetes with 250 with poorly controlled diabetes, matched for age, weight, and comorbidities. The hazard ratio for in-hospital mortality for well-controlled compared to poorly controlled diabetes was 0.14, which suggests hyperglycemia is directly driving the observed effects.
Overall, these results indicate the relationship between diabetes and COVID-19 severity is largely if not entirely driven by the specific deleterious effects of hyperglycemia on disease state. Individuals with poorly controlled diabetes may be particularly vulnerable to severe cases of COVID-19 and possibly other coronaviruses. These same individuals, however, may be able to rapidly reduce their risk by establishing effective blood glucose control. As previously reviewed on CrossFit.com, carbohydrate restriction, the ketogenic diet, and exercise can be used to rapidly establish blood glucose control. This indicates lifestyle changes can play a direct role in infectious disease prevention and management.
Notes
- Influence of diabetes mellitus on immunity to human tuberculosis; Innate immune signaling and its role in metabolic and cardiovascular diseases
- Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area; Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS; Prevalence of comorbidities in cases of Middle East respiratory syndrome coronavirus: a retrospective study
- Diabetic lung, an underrated complication from restrictive functional pattern to pulmonary hypertension
- Comorbid diabetes results in immune dysregulation and enhanced disease severity following MERS-CoV infection
- Prevention of accelerated atherosclerosis by angiotensin-converting enzyme inhibition in diabetic apolipoprotein E-deficient mice; SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor; Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding; A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury
- Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013
Comments on Association of Blood Glucose Control and Outcomes in Patients with COVID-19 and Pre-Existing Type 2 Diabetes
Not surprising, we are seeing a trend.
The ambient tissue glucose level (obviously higher in poorly controlled cases) favors the propagation of the tubule that allows the virus to attach and inject its genetic material into the susceptible cell. Such a simple remedy: keep your blood glucose in check. Such a simple prescription: eat a diet of meat, nuts & seeds, vegetables, some fruit, little starch, and no sugar.
Interesting. Thanks Mary
It’s important to specify LEAN meat. Not all meat is equal. I have eaten to my meter many times and fatty meats (sausage would be one example) my blood sugar is very high. Lean protein and it barely rises.
Association of Blood Glucose Control and Outcomes in Patients with COVID-19 and Pre-Existing Type 2 Diabetes
4